With the boom in sleeve gastrectomy (SG) for the treatment of morbid obesity, there have been a growing number of complications associated with this procedure.1 Among the most common are staple-line leaks, which result in fistulas.1–3 These leaks are typically located in the proximal third of the stomach, and they present specific characteristics. Several articles have published procedures for the treatment of fistulas after SG. Some recommend the use of esophageal stents in patients whose condition allows for conservative management.2–5 The use of these stents isolates the point of leakage, allowing the leak to close more quickly. Nonetheless, the use of these prostheses is not free of complications, which can include: stent migration and entrapment, food bolus obstruction, dysphagia, sialorrhea, bleeding and even esophageal perforation.5
Case ReportThe patient is a 49-year-old woman with morbid obesity who underwent laparoscopic SG. There were no immediate postoperative complications. Two months after surgery, the patient presented intermittent fever over the course of one week, with no other associated symptoms. Lab work revealed leukocytosis and high PCR levels. Abdominal CT scan showed an abscess in the subhepatic region. We attempted percutaneous drainage of the abscess, but the patient became unstable during the procedure and presented hematemesis as well as signs of septic shock, so she was taken to the operating room for exploratory laparotomy.
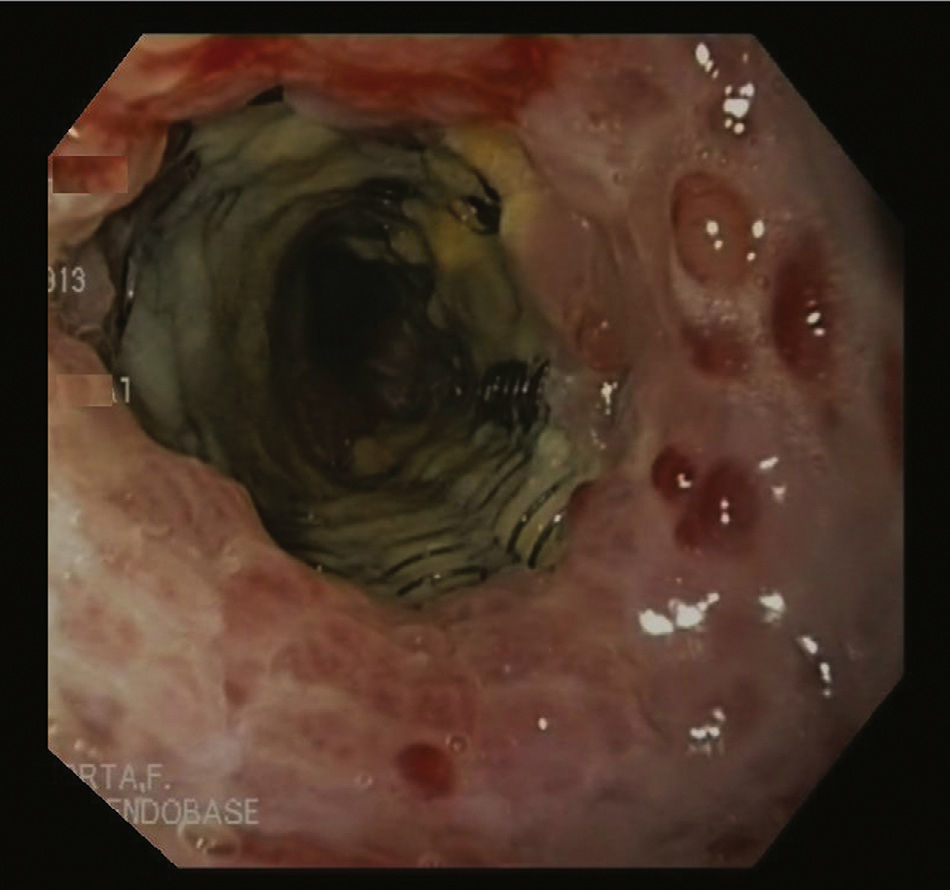
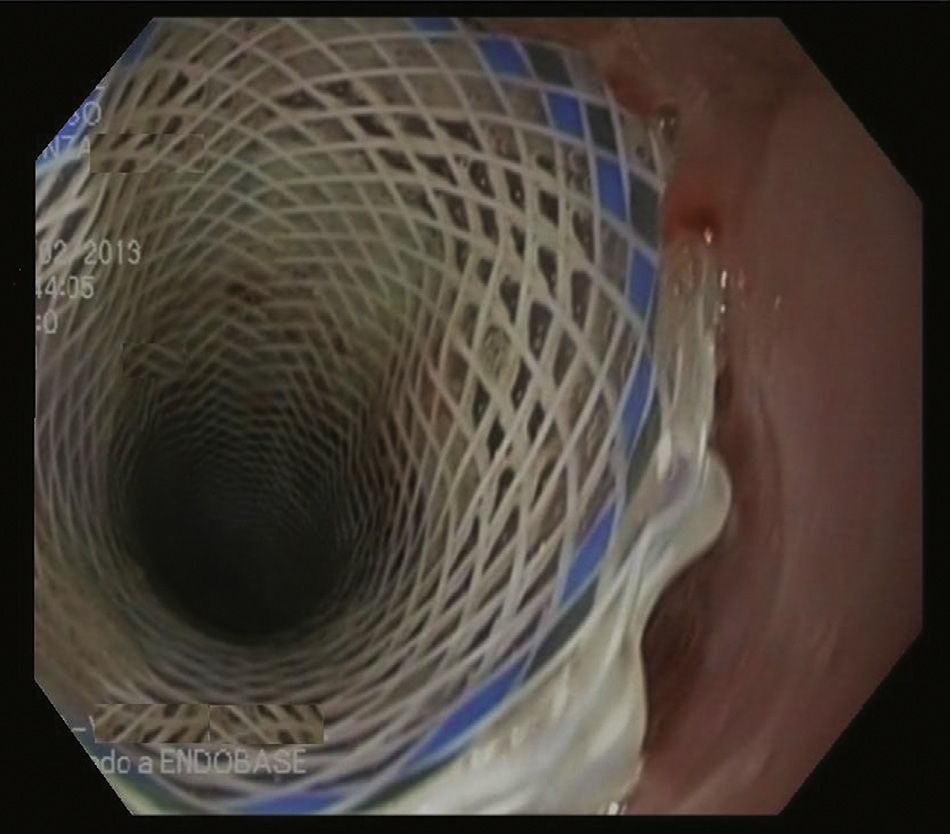
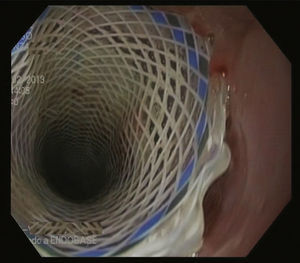
The abscess was drained along the staple line; no leakage was observed, so an intraoperative endoscopy was done, which detected the point of disruption. With this finding, we inserted a partially-coated metal Ultraflex® stent (Boston Scientific®) measuring 12cm long by 18mm in diameter. Four weeks later, we attempted to withdraw the prosthesis, but the procedure was not successful because both ends of the stent were covered by hyperplastic tissue. Due to the risk of esophageal perforation, manipulation of this tissue was complicated (Fig. 1). Therefore, the “stent-in-stent technique” was applied with the coaxial placement of another fully-coated Polyflex® stent (Boston Scientific®) in order to cause necrosis of the hyperplastic tissue. Fifteen days later, another endoscopic study revealed that the initial stent had become separated from the wall, and both prostheses were able to be withdrawn (Fig. 2). The patient had an uneventful recovery and was discharged 3 days later.
DiscussionThe use of stents in the esophagus is widely accepted for the palliative treatment of malignant esophageal diseases. In these situations, the aim is to maintain the lumen of the esophagus open, and it is not uncommon to observe new luminal obstructions in the stent, which are attributed to tumor growth. However, when these devices are used in situations where there is no underlying neoplasm, the development of redundant tissue is usually related to a foreign-body reaction.5,6 This phenomenon occurs as a result of a local stimulant that generates proliferation of granulation tissue. The incidence of benign mucosal hyperplasia has increased with the use of stents in benign disease.7–9 Although these cases lack pathologic confirmation, they generate doubt in the management of post-SG fistulas as the degree of stent entrapment is not always evident and there is a risk for esophageal perforation.
The origin of this hyperplasia is not clear, and different opinions exist. Many endoscopists suggest that it is due to the type of stent used, as this phenomenon occurs more frequently with metallic prostheses than with plastic-coated ones.8 In fact, plastic coating is considered an advantage in stent evolution as it was created to induce less local reaction. Nevertheless, there are studies that propose that the appearance of hyperplasia is not related with plastic coating or lack thereof, and they suggest other mechanisms that cause this phenomenon, such as: erosions during stent placement, circumferential pressure insertion, stent diameter, etc.9 Endoscopic specialists coincide in the opinion that the time that the stent stays in the organism is important. This is important in benign diseases, when stents in contact with the esophageal mucosa for prolonged periods determine the appearance of complications. It is therefore recommended to withdraw the stents as soon as possible.7–9
In cases of benign hyperplasia, stent retrieval can be a risky procedure since esophageal perforations during stent extraction have been reported.9 There are several approaches to resolve this complication with as little damage as possible, although the stent-in-stent technique is more widely accepted among endoscopists.10 This technique involves the placement of a plastic-coated stent within the trapped stent. This second stent should be the same diameter as the first, but the length should be longer. The objective is to create a certain amount of pressure on the areas of mucosal hyperplasia from the first stent, thereby causing necrosis of the redundant tissue, which can be freed after both stents. Some authors recommend withdrawing both prostheses 10–14 days after the stent-in-stent technique.10
FundingNo grants or any other type of funding was received for writing this article.
This manuscript was presented as a poster at the National Congress of Endoscopic Surgery, on 24–26 April, 2013, in Murcia, Spain.
Please cite this article as: Zubiaga L, Ruiz-Tovar J, Sola-Vera J, Uceda F, Calpena R. Técnica de «stent in stent» en la hiperplasia benigna del esófago. Complicaciones y tratamiento del manejo de las fístulas tras gastrectomía vertical. Cir Esp. 2015;93:123–125.