There is a wide variability in the management of acute cholecystitis. A survey among the members of the Spanish Association of Surgeons (AEC) analyzed the preferences of Spanish surgeons for its surgical management. The majority of the 771 responders did not declare any subspecialty (41.6%), 21% were HPB surgeons, followed by colorectal and upper-GI specialities. Early cholecystectomy during the first admission is the preferred method of management of 92.3% of surgeons, but only 42.7% succeed in adopting this practice. The most frequent reasons for changing their preferred practice were: patients not fit for surgery (43.6%) and lack of availability of emergency operating room (35.2%). A total of 88.9% perform surgery laparoscopically. The majority of AEC surgeons advise index admission cholecystectomy for acute cholecystitis, although only half of them succeed in its actual implementation. There is room for improvement in the management of acute cholecystitis in Spanish hospitals.
Existe una amplia variabilidad en el abordaje quirúrgico de la colecistitis aguda. Se presenta una encuesta a los miembros de la Asociación Española de Cirujanos (AEC) para analizar sus preferencias en el tratamiento de la colecistitis. La mayoría de los cirujanos que responden no declara ninguna superespecialidad (41,6%), el 21% son cirujanos hepatobiliopancreáticos, seguidos por cirujanos colorrectales y esofagogástricos. El 92,3% prefiere la colecistectomía durante el primer ingreso, aunque solo el 42,7% la realiza. Las razones más frecuentes para cambiar su práctica preferida son: pacientes no aptos para cirugía (43,6%) y poca disponibilidad de quirófano de urgencias (35,2%). El 88,9% realiza la colecistectomía por laparoscopia. La mayoría de cirujanos de la AEC aconseja la colecistectomía en el primer ingreso para la colecistitis, pero solo la mitad de ellos la aplica en su entorno clínico. Existen diversos puntos de mejora en el tratamiento de la colecistitis aguda en los hospitales españoles.
10%–15% of the western population has vesicular lithiasis, and 1%–3% of symptomatic patients develop acute cholecystitis.1 Despite its high frequency and the multiple studies addressing treatment, there is still controversy in the management of acute cholecystitis, ranging from the most appropriate time for surgical intervention to the most appropriate technique or antibiotic treatment.2 Audits on the management of cholecystitis that address these issues confirm the great variability that is available for its treatment,3–7 and in some cases, they have been used for decision-making in health policy.8,9 We do not know the existence of surveys that analyze the treatment of acute cholecystitis in Spain.
This study aims to determine the patterns of management of acute cholecystitis used by Spanish surgeons, with regard to their beliefs about the time of cholecystectomy and surgical technique, the difficulties encountered in applying their preferences to the reality of clinical practice, the empirical antibiotic treatment used and the relationship of these parameters with the degree of super-specialization or size of the hospital in which they exercise their clinical practice.
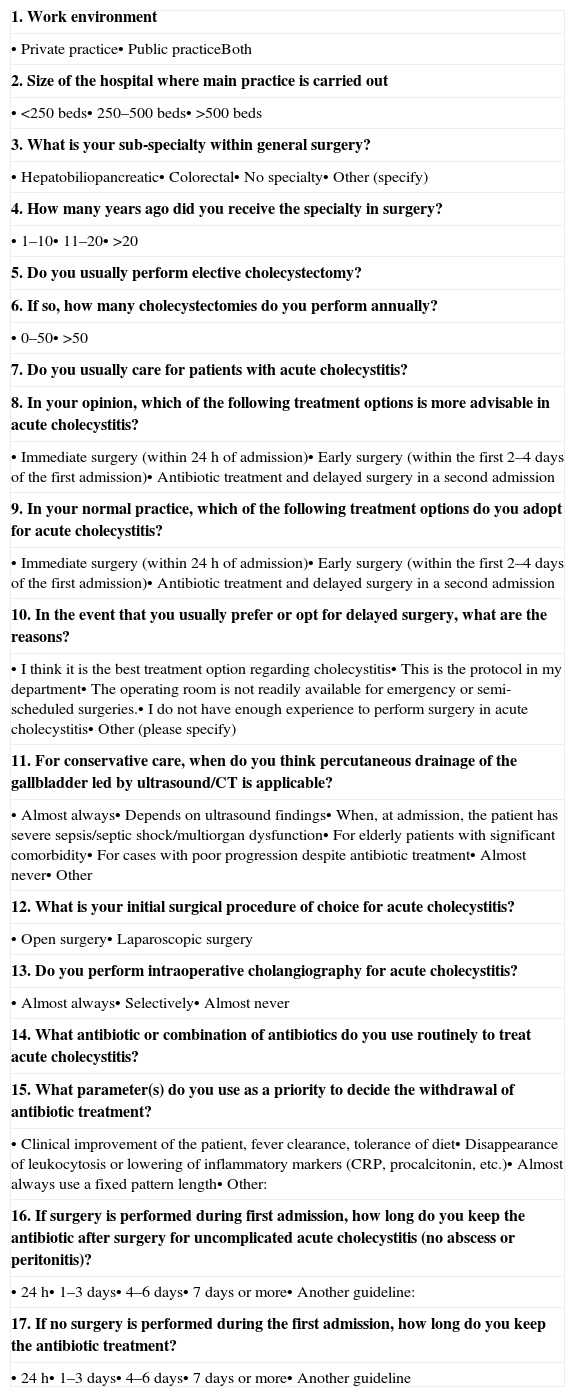
Materials and MethodWe designed an online survey (SurveyMonkey®) with 17 questions on work environment, hospital size, level of surgical expertise and management options for acute cholecystitis (Table 1). Some of the questions were about their beliefs regarding the timing of surgery (cholecystectomy during the first admission or medical treatment followed by delayed cholecystectomy in a second admission), the reality of its performance in practice, the reasons for not sticking to their preferences, type of surgical approach (laparotomy or laparoscopy) and the use of intraoperative cholangiography. Those who opted for delayed surgery were asked about the reasons for this practice, as well as about the situations where they would consider performing percutaneous transhepatic gallbladder drainage.
Survey Questions.
| 1. Work environment |
| • Private practice• Public practiceBoth |
| 2. Size of the hospital where main practice is carried out |
| • <250 beds• 250–500 beds• >500 beds |
| 3. What is your sub-specialty within general surgery? |
| • Hepatobiliopancreatic• Colorectal• No specialty• Other (specify) |
| 4. How many years ago did you receive the specialty in surgery? |
| • 1–10• 11–20• >20 |
| 5. Do you usually perform elective cholecystectomy? |
| 6. If so, how many cholecystectomies do you perform annually? |
| • 0–50• >50 |
| 7. Do you usually care for patients with acute cholecystitis? |
| 8. In your opinion, which of the following treatment options is more advisable in acute cholecystitis? |
| • Immediate surgery (within 24h of admission)• Early surgery (within the first 2–4 days of the first admission)• Antibiotic treatment and delayed surgery in a second admission |
| 9. In your normal practice, which of the following treatment options do you adopt for acute cholecystitis? |
| • Immediate surgery (within 24h of admission)• Early surgery (within the first 2–4 days of the first admission)• Antibiotic treatment and delayed surgery in a second admission |
| 10. In the event that you usually prefer or opt for delayed surgery, what are the reasons? |
| • I think it is the best treatment option regarding cholecystitis• This is the protocol in my department• The operating room is not readily available for emergency or semi-scheduled surgeries.• I do not have enough experience to perform surgery in acute cholecystitis• Other (please specify) |
| 11. For conservative care, when do you think percutaneous drainage of the gallbladder led by ultrasound/CT is applicable? |
| • Almost always• Depends on ultrasound findings• When, at admission, the patient has severe sepsis/septic shock/multiorgan dysfunction• For elderly patients with significant comorbidity• For cases with poor progression despite antibiotic treatment• Almost never• Other |
| 12. What is your initial surgical procedure of choice for acute cholecystitis? |
| • Open surgery• Laparoscopic surgery |
| 13. Do you perform intraoperative cholangiography for acute cholecystitis? |
| • Almost always• Selectively• Almost never |
| 14. What antibiotic or combination of antibiotics do you use routinely to treat acute cholecystitis? |
| 15. What parameter(s) do you use as a priority to decide the withdrawal of antibiotic treatment? |
| • Clinical improvement of the patient, fever clearance, tolerance of diet• Disappearance of leukocytosis or lowering of inflammatory markers (CRP, procalcitonin, etc.)• Almost always use a fixed pattern length• Other: |
| 16. If surgery is performed during first admission, how long do you keep the antibiotic after surgery for uncomplicated acute cholecystitis (no abscess or peritonitis)? |
| • 24h• 1–3 days• 4–6 days• 7 days or more• Another guideline: |
| 17. If no surgery is performed during the first admission, how long do you keep the antibiotic treatment? |
| • 24h• 1–3 days• 4–6 days• 7 days or more• Another guideline |
A letter was sent via email to all members of the Asociación Española de Cirujanos (AEC) [Spanish Association of Surgeons], with a link to the website containing the survey. In addition, the survey was publicized through AEC's electronic newsletter, and the answer period was kept open for one year. Some questions allowed multiple answers. Results are expressed as percentages of the total answers obtained. Answers were entered into a computerized database that was analyzed by SPSS software (version 10.0, Chicago, IL, USA). The results were analyzed by the chi-square test. Statistical significance was accepted at P<.05.
ResultsOverall ResultsWe received 771 answers, from a total of 4000 associates. 72.3% of respondent surgeons performed activities in the field of public medicine, and 22.9% combine it with private practice. Hospital levels are spread very evenly, with a third of surgeons in hospitals with <250 beds, a third with 250–500 beds, and all others with >500 beds.
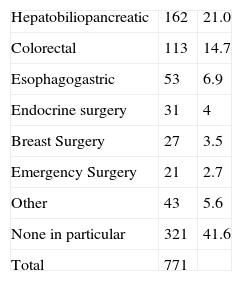
SpecializationSurgeons’ experience, expressed by years spent performing their specialization, is also shared equally into thirds, among intervals of 1–10 years, 11–20 years and >20 years. Of all respondents, the largest group declared having no sub-specialty (41.6%); 21% listed hepatobiliopancreatic surgery (HPB). The rest is distributed into smaller proportions: colorectal surgery, esophagogastric surgery, and other (Table 2). When compared by hospital size, there are significant differences in the degree of super-specialization. For example, there are more HPB specialists in hospitals with >500 beds (26.4% compared to 18.3%, P=.01). However, even in the hospitals with the most beds, 28.3% of respondent surgeons have no super-specialization (Table 3).
Answers by Hospital Size n/No. (%).
| Hospital size | No super-specialty | Preference for delayed surgerya | Real option for delayed surgeryb | No availability of operating roomc | Start with laparoscopic | |||||
| <250 | 173/242 | (71.5) | 25/242 | (10.3) | 80/241 | (33.2) | 75/186 | (39.8) | 201/240 | (83.8) |
| 250–500 | 75/271 | (27.7) | 17/271 | (6.3) | 62/271 | (22.9) | 50/188 | (26.6) | 248/269 | (92.2) |
| >500 | 73/258 | (28.3) | 17/258 | (6.6) | 73/256 | (28.5) | 70/177 | (39.5) | 231/256 | (90.2) |
| Total | 321/771 | (41.6) | 59/771 | (7.7) | 215/768 | (28) | 194/551 | (35.2) | 680/765 | (88.9) |
92.5% of respondents routinely performed elective cholecystectomy, of which 63.3% performed less than 50 cholecystectomies per year, and 36.7% over 50 cholecystectomies per year. 93.1% regularly treat patients with acute cholecystitis.
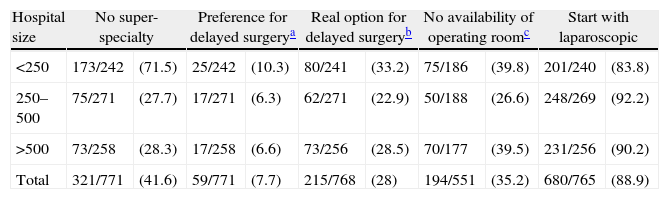
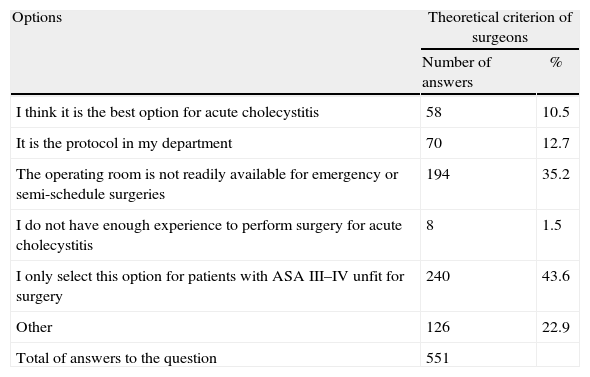
Preference for Surgery TreatmentImmediate cholecystectomy (within 24h of admission) is the preferred treatment option for 58.6% of surgeons, while 33.7% of the respondents prefer early surgery (within the first 2–4 days of admission). In total, 92.3% preferred surgery in the first admission. By contrast, 7.7% think (theoretically) that the recommended option is medical treatment with antibiotics, followed by delayed elective cholecystectomy in a second admission (Table 4). When inquired about how their convictions apply to the reality of clinical practice, 42.7% of surgeons performed immediate cholecystectomy, 29.2% early cholecystectomy (overall 71.9% of surgery in the first admission) and 28% prescribed antibiotics and delayed cholecystectomy. The latter were asked about reasons for their position, and the most common were: in patients with ASA III-IV classification unfit for surgery (43.6%); lack of availability of the emergency surgery operating room (35.2%); adherence to the protocol of their department (12.7%); or initial preference for conservative treatment (10.5%) (Table 5). Other constraints for early treatment (22.9%) are: clinical progression longer than 5 days, jaundice, abnormal liver enzyme profile, and antiplatelet or anticoagulation in clinically stable patients. The 161 surgeons who believe in performing early surgery but defer it, do it for lack of operating rooms (65%) or following their department's protocol (29%). HPB surgery specialists perform surgery most of the times during the first admission (81.3% compared to 69.5%, P=.03) (Table 6).
Comparison Between Theory and Practice of the Ideal Time for Cholecystectomy.
| Options | Theoretical criterion of surgeons | Reality of clinical practice | P | ||
| Answers | % | Answers | % | ||
| Immediate surgery (first 24h) | 452 | 58.6 | 328 | 42.7 | <.0001 |
| Early surgery (2–4 days) | 260 | 33.7 | 224 | 29.2 | <.0001 |
| Antibiotic therapy and delayed surgery during second admission | 59 | 7.6 | 215 | 28 | <.0001 |
Reasons to Opt for Antibiotic Therapy and Delayed Cholecystectomy in Clinical Practice (the Question Allowed Multiple Answers).
| Options | Theoretical criterion of surgeons | |
| Number of answers | % | |
| I think it is the best option for acute cholecystitis | 58 | 10.5 |
| It is the protocol in my department | 70 | 12.7 |
| The operating room is not readily available for emergency or semi-schedule surgeries | 194 | 35.2 |
| I do not have enough experience to perform surgery for acute cholecystitis | 8 | 1.5 |
| I only select this option for patients with ASA III–IV unfit for surgery | 240 | 43.6 |
| Other | 126 | 22.9 |
| Total of answers to the question | 551 | |
When medical treatment is chosen, the most common prescriptions for percutaneous cholecystostomy directed by ultrasound/CT are: elderly patients or with significant comorbidities (61.9%), having severe sepsis at admission, septic shock or multiorgan dysfunction (35%) and poor progression despite antibiotic treatment (26%). A quarter of the respondents to this question (165/675) barely ever resort to percutaneous cholecystostomy.
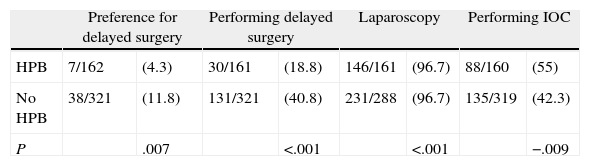
Surgical TechniqueMost respondents begin with laparoscopic surgery (88.9%) compared to 11.1% who perform open surgery. The laparoscopy percentage is greater for HPB surgeons (96.7% compared to 85.6%, P<.001). 54.2% of respondents answered that they almost never perform intraoperative cholangiography (IOC) for acute cholecystitis, 42.3% perform it selectively, and 3.5% practice it almost always. HPB surgeons perform more routine or selective IOC (55.0% compared to 43.4%, P=.009). No differences were observed in treatment timing, laparoscopy percentage or performing IOC depending on the hospital size.
Antibiotic TherapyThe most commonly used antibiotics were piperacillin–tazobactam (49.9%), amoxicillin–clavulanate (47.8%) and ertapenem (24.5%). Other antibiotics are prescribed less than 10% each (meropenem, cephalosporins 1st, 2nd or 3rd generation alone or in combination with metronidazole, quinolones or tigecycline). Regarding the duration of antibiotic treatment after early emergency surgery, most surgeons keep it for 1 to 3 days (44.3%), 25% keep it for 4–6 days, and 22.3% prescribe it only during the first 24h postoperatively. Only 5.5% extend it longer than 7 days. Half of surgeons decide on the completion of antibiotic treatment based on clinical improvement, disappearance of fever and tolerance of oral diet (51.2%), while 46.6% use a fixed duration system. 31.6% based their decision on infection/inflammation markers such as absence of leukocytosis and decreased inflammatory markers (CRP, procalcitonin). In the event cholecystectomy is not performed during the first admission and medical treatment is selected, most respondents kept antibiotic therapy for 7 or more days (60.4%), followed by a period of 4–6 days (33.4%), while a small percentage uses a short duration system (0.8% for 24h, 1.6% for 1–3 days).
DiscussionFew diseases are as common as acute cholecystitis, and at the same time, have so much variability in therapeutic management. Despite the vast literature of the last 2 decades, considerable controversy persists over the most appropriate time for surgery, the use of laparoscopy and the cost of the different treatment options, which has even led to designing strategies for decision-making in specific clinical situations.2 Surveys in several countries for the treatment of this disease provide valid information on this variability, and in some cases, have been useful in planning health policy changes.8,10 This study aims to examine the reality of cholecystitis management in Spain through the beliefs and experiences of AEC member surgeons.
Specialization and Hospital SizeSuper-specialization data show no significant differences by hospital size. Surprisingly, even in hospitals with >500 beds, 41.6% of Spanish surgeons claim not to belong to any particular area of interest or super-specialization. Perhaps that is why almost all surveyed surgeons practice elective surgery for cholelithiasis, and usually treat patients with cholecystitis, which gives validity to the results.
Surgical Time of CholecystectomyOne of the main objectives of the survey was to find out the percentage of surgery during first admission for acute cholecystitis, a disease that is perhaps the paradigm of intraabdominal infection with a resectable site of origin. Cholecystectomy obtained the best overall results for treatment and is the main weapon to reduce morbidity and mortality, as well as health costs related to this disease,11 but the ideal moment or timing for surgery has been controversial. The timing of surgery has caused numerous randomized trials for open surgery12–20 and laparoscopic surgery,21–28 with results that leave little room for doubts. The first studies, published between 1970 and 1992, analyzed 916 randomized patients in one group with early surgery in the initial days of the episode, and other group with delayed surgery weeks or months from cholecystitis medical treatment. A similar rate of complications was obtained, but with worse results in the delayed surgery group in terms of increased mortality (not statistically significant) and longer hospital stay. A study performed a financial analysis showing higher health care costs for the delayed surgery group.29 This group also shows 20%–25% failure of antibiotic treatment, requiring surgery at a stage of the disease less suitable for cholecystectomy, and 10% surgery rejection once the initial problem was solved. 15% of patients initially treated with antibiotics suffer symptoms again after discharge and during the period prior to being operated on; 26% of them require emergency surgery.
Randomized trials published since 1998 with the laparoscopic technique comparing early and delayed surgery found similar results in terms of operative morbidity, with a shorter hospital stay than for open surgery, and absence of mortality. In 2004, a meta-analysis brings together the results of 12 controlled studies on both open and laparoscopic surgery.30 No differences in morbidity or mortality were found. The rate of bile duct lesion in open surgery is 0.2% for the early group and 0.9% for the delayed group, and for laparoscopic surgery, 0 in the early group and 0.9% in the deferred group. Hospital stay is doubled in the delayed surgery group. The rate of conversion to open surgery was 21% for laparoscopic cholecystectomy. For the early surgery group, this rate tends to be lower than for the deferred group, although not statistically significant. The most recent Cochrane update (2013) analyzes 488 patients operated for cholecystitis by laparoscopic techniques. A lesion of the common bile duct was detected in early surgery (0.4%), and 2 in delayed surgery (0.9%), without statistical significance (Peto OR 0.49, 95% CI: 0.05–4.72). Although there were no significant differences in mortality and morbidity, delayed surgery represented a longer hospital stay and a more delayed return to work. In this group, 18% suffered persistence or recurrence of symptoms before elective surgery, forcing emergency surgery, with a conversion rate to open surgery of 45%.31 Laparoscopic cholecystectomy can be performed without increased complications or conversion rate up to at least 4 days from onset of symptoms.32 A retrospective study of almost 2000 patients found no increased conversion up to 7 days after admission.33
Economic studies in Great Britain and Canada show lower health care costs and a better quality of life for patients when an early laparoscopic surgery policy is applied for acute cholecystitis.9,34
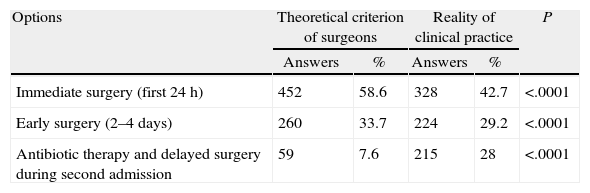
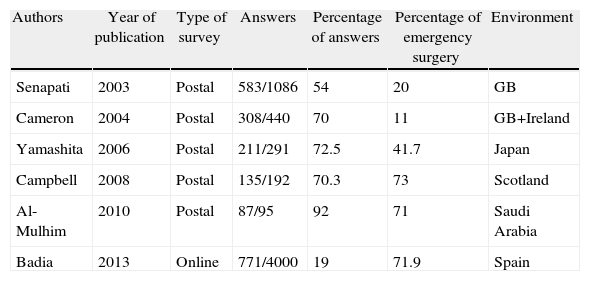
Surveys published between 2003 and 2010, based on questionnaires sent by postal mail, showed 11%–71% cholecystectomy percentages during the first admission (Table 7). Other studies in 2008 show a rate of surgery on first admission of 41% in Los Angeles35 and 29.8% in an English epidemiological study with 25743 patients.10 Unlike other surveys, this one asked not only about the practical reality of care, but also about surgeons’ theoretical convictions and the constraints experienced in adhering to them. It is noteworthy that 92.3% of respondents believe that acute cholecystitis must be tackled within the first 4 days after admission (emergency or early); however, this high percentage drops to 71.9% when the question asks about health care reality. The most important causes that prevent surgeons adhering to their personal beliefs are the poor general condition of patients and a worrying lack of availability of operating rooms for emergency or deferred emergencies. Additionally, 12.7% of surgeons work in departments where deferred treatment of cholecystitis is protocolized, and 7.6% still believe that medical treatment is the best choice. The final result is that 7.6% of those supporting “cooling off” acute cholecystitis rises to 28% when the reality of care in our hospitals is analyzed.
Surveys Published on Therapeutic Management of Acute Cholecystitis.
| Authors | Year of publication | Type of survey | Answers | Percentage of answers | Percentage of emergency surgery | Environment |
| Senapati | 2003 | Postal | 583/1086 | 54 | 20 | GB |
| Cameron | 2004 | Postal | 308/440 | 70 | 11 | GB+Ireland |
| Yamashita | 2006 | Postal | 211/291 | 72.5 | 41.7 | Japan |
| Campbell | 2008 | Postal | 135/192 | 70.3 | 73 | Scotland |
| Al-Mulhim | 2010 | Postal | 87/95 | 92 | 71 | Saudi Arabia |
| Badia | 2013 | Online | 771/4000 | 19 | 71.9 | Spain |
In 2003, we conducted a survey via postal mail (Badia 2003, unpublished data), directed to department Heads in Spanish hospitals. The percentage of surgery during first admission (70%) did not differ much from the current one. This aspect of the treatment of acute cholecystitis in Spanish hospitals has not changed substantially for almost a decade. However, there has been a shift to surgery on the first day of hospitalization. In 2003, immediate surgery was the top choice (<24h) for 18.8% of departments, and in 2011, 42.7% of surgeons performed it. Conversely, in 2003, 51.2% performed early surgery (2–4 days), while in 2011, only 29.2% do.
LaparoscopyThe vast majority of Spanish surgeon respondents initiate acute cholecystitis surgery laparoscopically, with HPB surgeons and those performing >50 cholecystectomies annually being the ones that use this technique the most (97%). Laparoscopic cholecystectomy is feasible and safe in acute cholecystitis.36 Several controlled studies have compared open surgery with laparoscopy for acute cholecystitis,37–40 and found no substantial differences between the two techniques. However, in severe cholecystitis (gangrenous cholecystitis and empyema), a low threshold must be kept for conversion to open surgery. A meta-analysis studies the results of laparoscopic cholecystectomy in these severe cholecystitis cases intervened with laparoscopy, finding a slight increase in postoperative complications and 3 times more possibility of conversion when compared with mild cholecystitis.41
As in open surgery, laparoscopic technique studies found no differences between early and delayed cholecystectomy in terms of the bile duct lesion, infectious complications, conversion rate or duration of the surgery. Gurusamy et al., in a meta-analysis on the safety and effectiveness of early laparoscopic cholecystectomy compared to deferred laparoscopic cholecystectomy, demonstrates the safety of early surgery, which reduces hospital stay and avoids the risk of emergency surgery during the waiting period of delayed surgery.31
In summary, early laparoscopic cholecystectomy seems to be the treatment of choice for acute cholecystitis; however, it is a technically complex surgery that should be performed by surgeons with experience not only in laparoscopic cholecystectomy, but also in open surgery. This data indicates that the ideal management would be planning delayed emergency surgery, in a morning or afternoon operating room, by a team specialized in HPB surgery and laparoscopy.8 In the few patients who cannot be treated under general anesthesia, imaging-led percutaneous cholecystostomy is a good alternative, except in cases with advanced gangrene or gallbladder perforation.42
Intraoperative cholangiography appears to be little used in Spain, at least for acute cholecystitis. Our results contrast with a published audit in the U.S. where it is performed in 11% of cases routinely, and in 70% selectively.43
Antibiotic TreatmentEmpirical antibiotic treatment guidelines reported by respondents show good coverage for cholecystitis,44 which may be treated with clavulanate–amoxicillin alone (at doses of 2g every 8h and provides good coverage against Gram-negative and anaerobic enterococcus) or associated with aminoglycoside depending on local resistance of E. coli (reaching 10%–15% in some hospitals), or with ertapenem or piperacillin–tazobactam. The current trend to recommend short courses of antibiotic therapy in intra-abdominal infection, especially if the septic focus is well controlled, seems to be popular among Spanish surgeons. 66.6% of surgeons state performing treatment less than 3 days when surgery is performed, which can prevent the emergence of resistance and maintains bacterial ecology of hospitals. Limiting the use of antibiotics is another argument favoring early surgery. Only 5.5% of surgeons keep antibiotics more than 7 days after surgery when operating in first admission, while this figure rises to 60.4% when opting for medical treatment.
Limitations of the StudyIt can be argued that we have obtained a low response rate to the survey. It is difficult to know precisely the response percentage, given the uncertainty about the calculation's denominator: the number of members of the Spanish Association of Surgeons who use AEC email and actually received the contact message or read the notification in the association's newsletter. In any case, the absolute number of answers is high and, taking as the denominator the total number of members, a response rate of 771/4000 seems sufficiently representative. Our online survey is the one with the highest number of answers when compared to the published surveys via postal mail, at the expense of achieving the lowest percentage. Maybe online surveys can obtain the maximum gross number of answers in exchange for a lower answer rate.
ConclusionsTheoretically, management of acute cholecystitis by Spanish surgeons fits the scientific evidence and compares very favorably with the experience published in other countries, in terms of the ideal time for surgery, use of laparoscopy and duration of antibiotic therapy. However, the reality of health care reflects difficulties in the implementation of early surgery, generally due to hospital organizational problems, existence of outdated protocols and unclear recommendations of some scientific societies. We believe that the heads of surgical departments and scientific societies must issue clear recommendations for early laparoscopic surgery and boost organizational measures to ensure that these are met.
Conflict of InterestThe authors declare having no conflict of interest.
Please cite this article as: Badia JM, Nve E, Jimeno J, Guirao X, Figueras J, Arias-Díaz J. Tratamiento quirúrgico de la colecistitis aguda. Resultados de una encuesta a los cirujanos españoles. Cir Esp. 2014;92:517–524.