Aspiration of foreign bodies (FB) is a common emergency in pediatric populations1; however, some adults are also at high risk. FB in the airway should be managed with a bronchoscope. If this fails, surgery is indicated. The associated airway and digestive injury usually occurs when the diagnosis is delayed.2
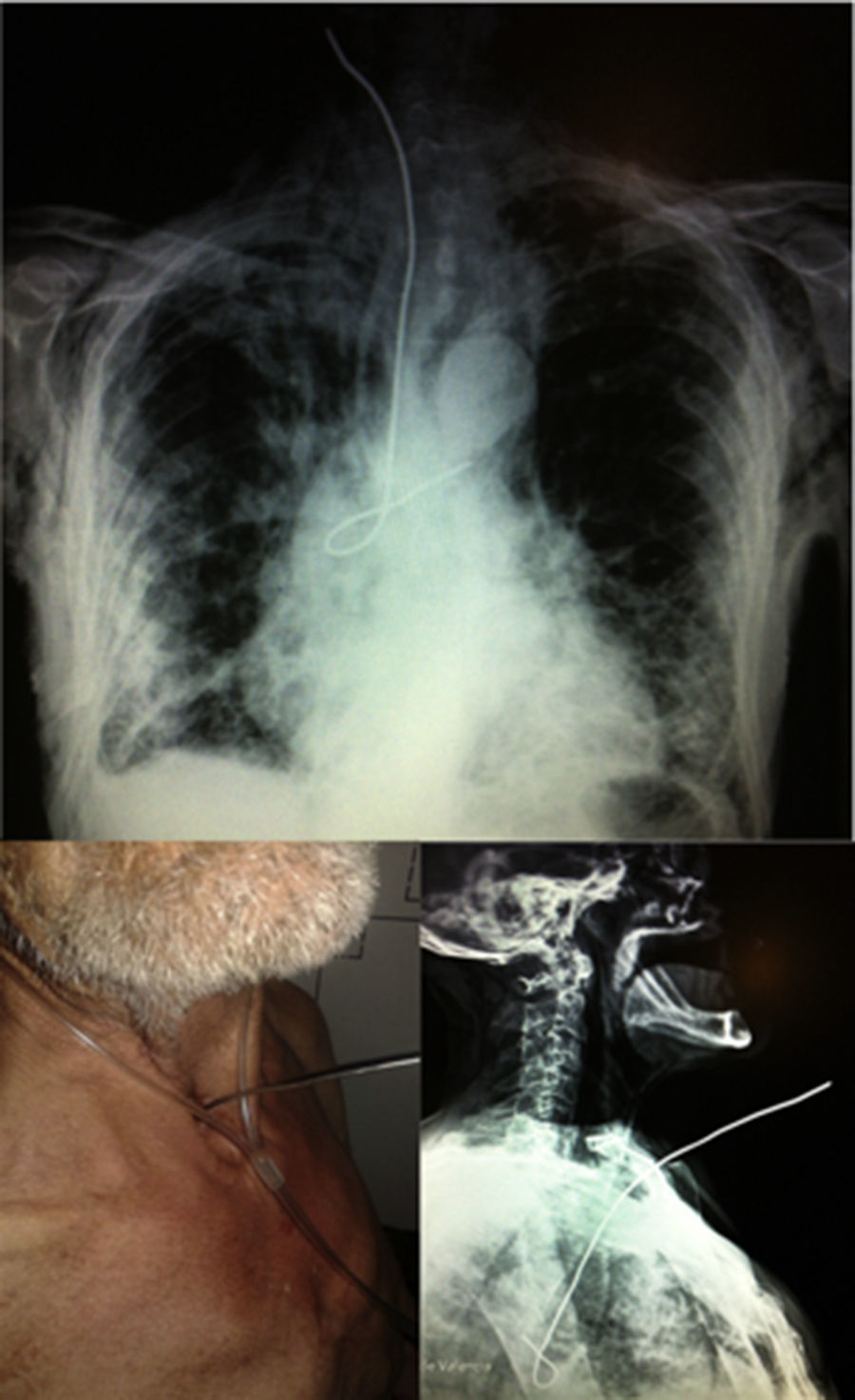
We present the case of a 77-year-old man with a tracheostomy who came to the emergency room due to the impossibility of extracting a wire that he used to “scratch” through the tracheostomy. Upon examination, the patient was hemodynamically stable and had subcutaneous emphysema, diffuse rales, and the end of a metal wire showing through the tracheostomy orifice. The chest X-ray showed the end of the wire in the trachea (Fig. 1).
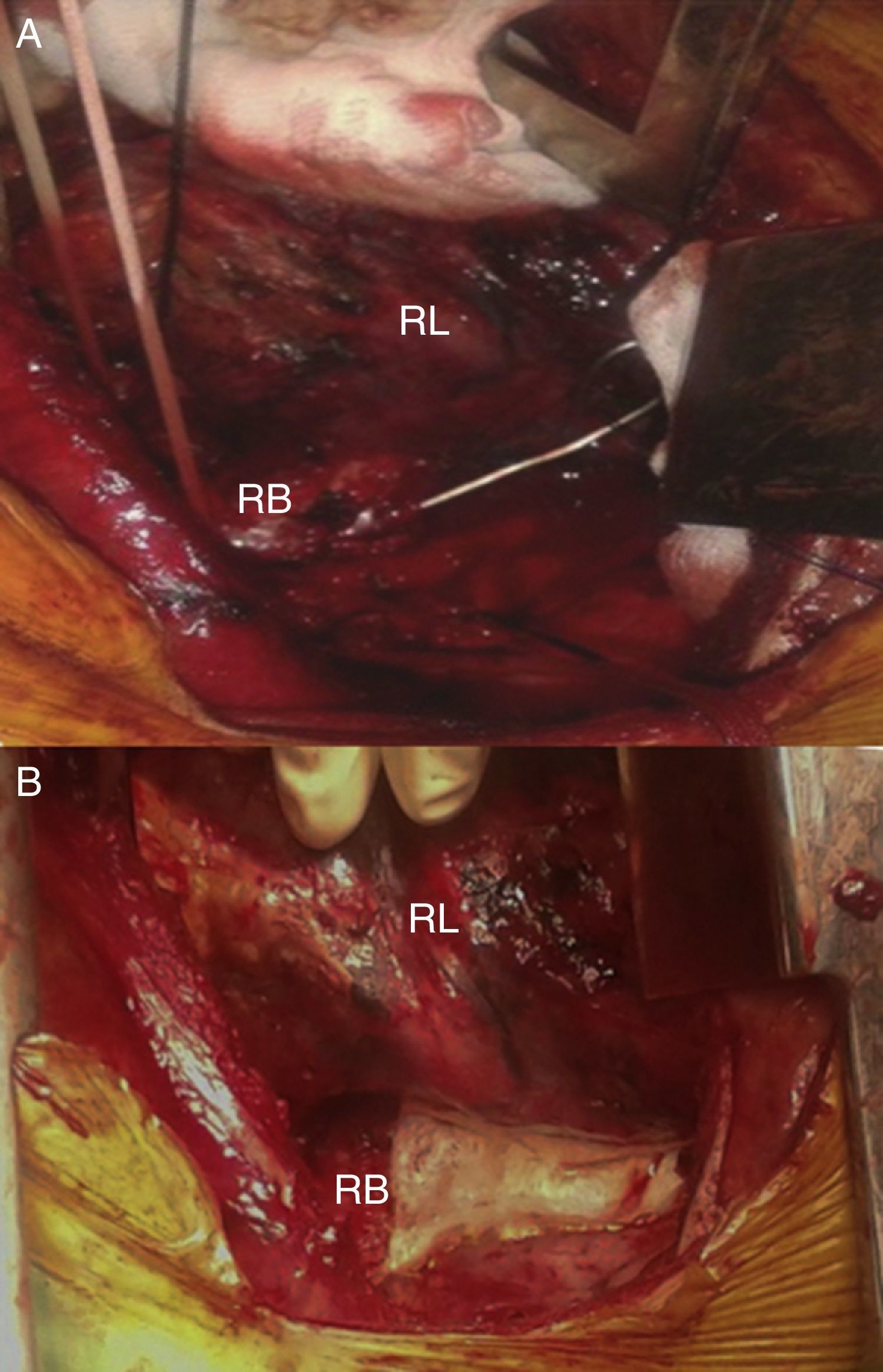
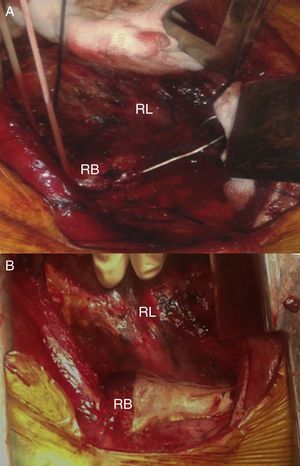
As airway perforation was suspected in a stable patient, we ordered a computed tomography scan. However, on the way to radiology the patient presented desaturation, so the airway was secured and the patient was taken to the operating room, where bronchoscopy was performed. We observed that the wire was perforating the right bronchus, and we decided on immediate operation. Through a right posterolateral thoracotomy, we confirmed the perforation of the right bronchus, associated with a pierced esophagus. We removed the wire from the esophagus and performed a bronchotomy to complete its extraction, followed by the primary closure of both defects reinforced by thrombin patches (Fig. 2). On the 7th day after admission, bronchoscopy verified watertightness of the bronchial repair; the patient also demonstrated adequate oral tolerance, so he was discharged.
The management of an aspirated FB should be that of a critical condition. The airway is a priority, which should be secured according to the needs of the case. The majority of aspirated FB are removed by rigid or flexible bronchoscopy, reaching success rates of up to 95–98%.3 In tracheostomy patients, FB extraction is possible by different means. In our case, the airway was initially secured by a simple endotracheal tube through the tracheostomy and, in the operating room, this was replaced with a double-lumen tube. As bronchoscopy showed evidence of bronchial perforation, we decided to operate.
Intraoperatively, bronchial and esophageal lesions were evident. The esophagus presented a punctiform perforation, so we decided to perform primary closure. However, for the extraction of the rest of the wire, a 2cm bronchotomy was performed, followed by primary closure and reinforcement.
The location of the lesion during bronchoscopy is significant as it influences the surgical approach. There are 4 approach options: cervicotomy for proximal tracheal lesions; cervical-sternotomy for lesions of the middle third; right thoracotomy for distal tracheal lesions, any lesions in the right bronchus or proximal left bronchus (first 3cm); and left thoracotomy for distal lesions of the left bronchus. Recently, video-assisted approaches (VATS)4 have also been described.
Once the approach is decided on, we must remove the bronchoscope and repair the associated damage. Usually, the repair technique is primary closure. In selected cases, limited resections of the airway (usually up to 2cm) may be performed with primary anastomosis. Some authors recommend reinforcing the suture line with biological patches (muscular, pericardial or omental). However, their use entails risks, such as bleeding or necrosis, with associated re-operation rates of up to 9%.5,6 Thrombin/fibrinogen patches have been described as an option for anastomotic reinforcement, reducing the rate of air leaks.7,8
In conclusion, the aspiration of a foreign body is an emergency, and airway control requires special attention. Once secured, bronchoscopy should be performed to try to remove the object. If this were not possible, surgery should be considered, and the approach should be determined by the location of the FB. Primary closure is the most common airway lesion repair technique, which may or may not be associated with autogenous or heterogeneous reinforcement.
FundingNo funding of any kind was received for the completion of this article.
Please cite this article as: León Espinoza C, Cerón Navarro J, Galán Gil Genaro G, Ortega Serrano J. Extracción quirúrgica urgente de cuerpo extraño en la vía aérea. Cir Esp. 2017;95:351–352.
All the authors have participated in the writing and review process of this article and have approved the final version.