A vascular kinking is a malformation, typically arterial, whose most likely origin is embryonic,1 derived from an excessive length of the vessel, which gives it a Z-shape and has been shown to be an independent cardiovascular risk factor.2 Due to its high surface area in contact with the surrounding structures, which it can even totally or partially envelop, it poses a surgical difficulty with a risk of injury.
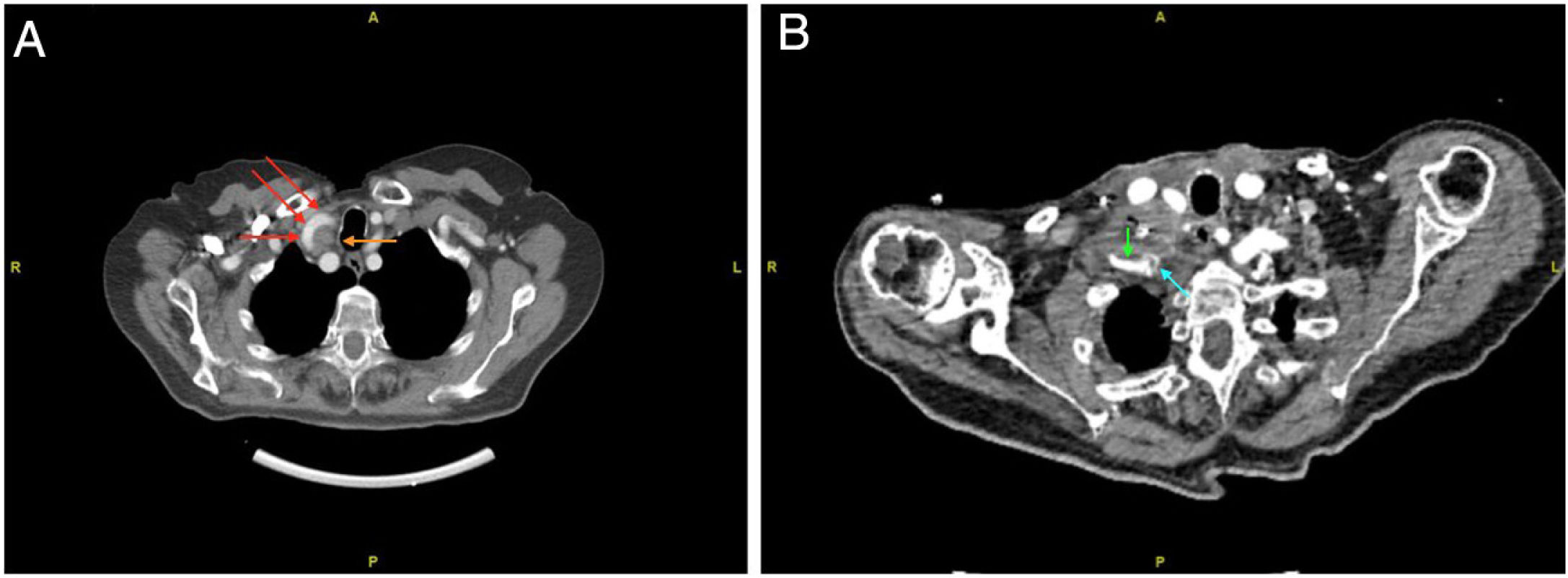
We present the case of an 89-year-old woman with a history of papillary thyroid carcinoma treated by total thyroidectomy and I131 30 years earlier. During follow-up, a TgB elevation of 16 ng/mL was detected in one year, associated with a single palpable lymphadenopathy at the level of the right IV region measuring 27 × 22 × 18 mm confirmed by PET-CT. Because of the high surgical risk due to age and previous surgery, it was decided to treat initially by alcoholisation. The control CT scan (Fig. 1A) showed persistent lymphadenopathy in the cervical level IV on the right side, with no infiltration of vascular structures. As an incidental finding, there was bilateral kinking of the common carotid artery at its proximal origin in the vicinity of the beginning of the subclavian artery, closely related to the suspected lymphadenopathy.
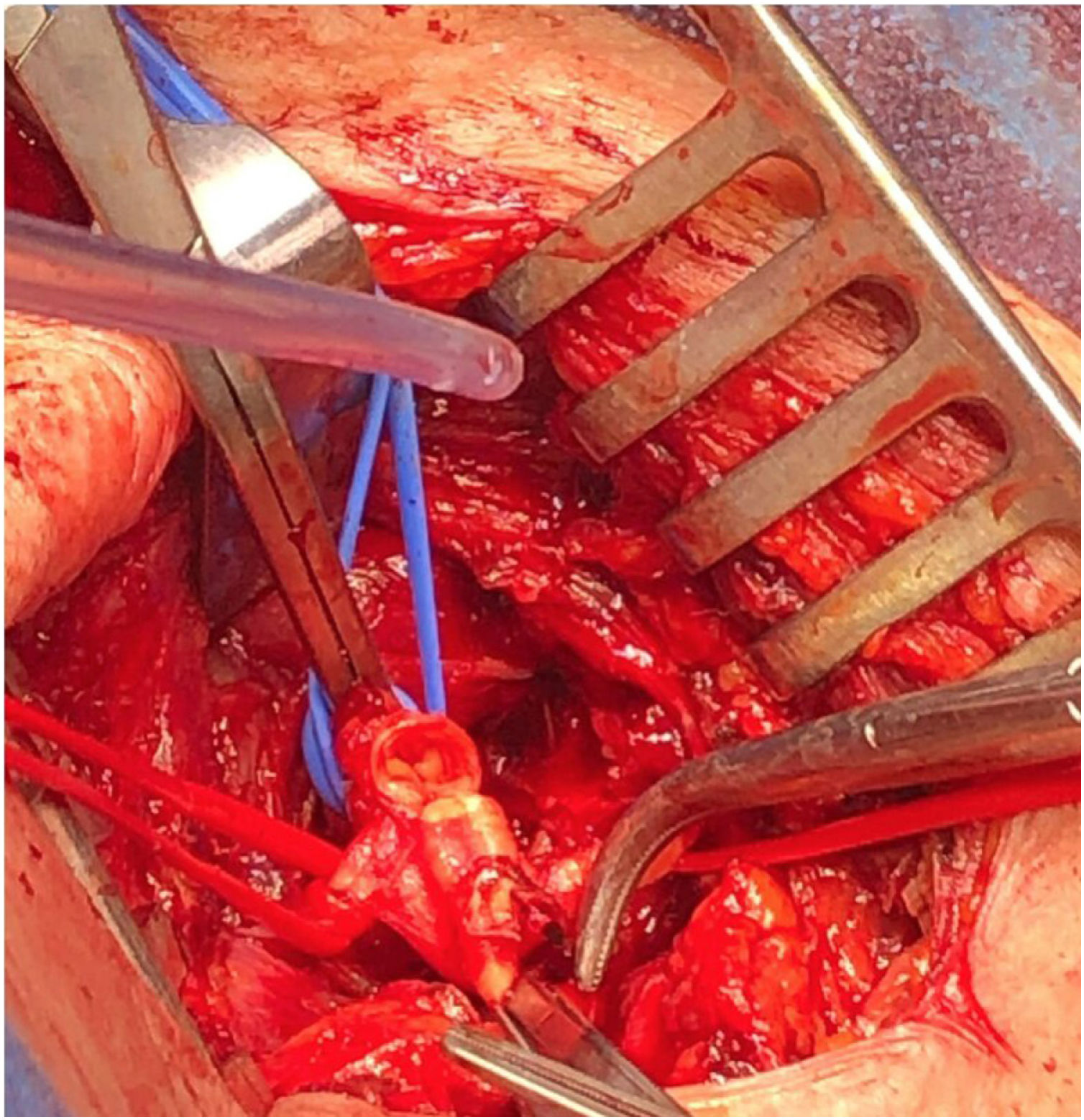
Given the failure of alcoholisation, surgical intervention was decided. During excision of the adenopathy, intense vascular calcification was observed, which made dissection more difficult and led to a partial section of the right subclavian artery (Fig. 2) due to surgical manipulation, which was reconstructed with a subclavian by-pass with an expanded polytetrafluoroethylene (ePTFE) prosthesis (Fig. 1B). On the third postoperative day she was diagnosed with a thrombosis at the level of the right humeral artery. Despite the perceived symptoms, she refused surgical reperfusion and was managed exclusively with anticoagulation therapy. On the seventh day, complete recovery of vascularisation and disappearance of symptoms was observed and the patient was discharged. The patient refused treatment with con I131 and one year later her TgB levels were on the rise, and there was a suspicion of tumour recurrence in the same location detected by CT scan. There are no vascular problems related to the carotid or subclavian territories.
The incidence of lymph node metastases in the lateral cervical compartment in patients with papillary thyroid cancer can be as high as 20.9%,3 with cervical level III being affected more frequently than the others (62,6%).4 Levels III and IV, in addition to being the most frequently affected, are also the most anatomically related to the cervical vascular bundle as they are located along the sternocleidomastoid and are in close contact with the carotid sheath and, in the case of level IV, also with the proximal portion of the subclavian artery. This proximity may imply a high risk of intraoperative vascular injury, especially in patients with aberrant or less common distributions.
In terms of arterial malformations, kinking is the most frequent of all,5 being present in 10%–25% of the population.6 There is currently no clear indication for surgical treatment of kinking if it remains asymptomatic. However, in symptomatic kinking cases, symptom reduction due to decreased blood flow through the kinking has been observed7 and endarterectomy is effective in preventing ipsilateral ischaemic cardiovascular eventss8 without a statistically significant risk of vascular complications from revascularisation surgery.9
Although cervical arterial vascular malformations are infrequent, their presence, especially in older patients, may condition the surgical technique and/or approach, so we believe that the participation of multidisciplinary teams including vascular surgery is beneficial in patients with this preoperative diagnosis. As this is an isolated case, it is difficult to draw conclusions or recommendations, but we believe that it could provide useful information for the treatment of future patients who may find themselves in a similar situation.
Please cite this article as: Botella Casas G, Cassinello Fernández N, Pérez Santiago L, Alfonso Ballester R, Ortega Serrano J. Influencia de la presencia de anomalía anatómica carotídea en la cirugía de rescate por recidiva de carcinoma papilar de tiroides. Cir Esp. 2022;100:657–659.