Laparoscopic adjustable gastric banding (LAGB) is one of the three most common procedures performed worldwide for treating morbid obesity, with a global reported incidence of 12.1% of all bariatric procedures. However, incidence of different techniques are variable among countries1 LAGB has the advantage of being the least invasive, with the fastest insertion, adjustable restriction, reversibility, and anatomy preservation.2 However, extensive studies on LAGB have reported a complication rate of up to 30–40%, including slippage, port dysfunction, band erosion, food intolerance, bowel obstruction, and band migration to the gastrointestinal tract, with or without perforation, being this last one, extremely rare with only a few cases reported in the literature.3 The objective of this letter is to present a female patient who presented with a gastric band migration into the jejunum.
A 50-year-old female patient was admitted to the hospital with abdominal pain in the epigastric region, nausea, and vomiting after a one-month history of colicky abdominal pain in the same region. The patient had a medical history of LAGB insertion 19 years ago, with the last follow-up 10 years ago. Her body mass index (BMI) at the moment of the bland placement was 55kg/m2. Her current BMI is 40kg/m2. The patient lost 45kg of body weight, for a total weight loss of 31%. The patient was hemodynamically stable and afebrile. Physical examination showed abdominal distension with reduced bowel movements to auscultation accompanied by diffuse abdominal tenderness to superficial and deep palpation, with a tympanic colonic margin to percussion.
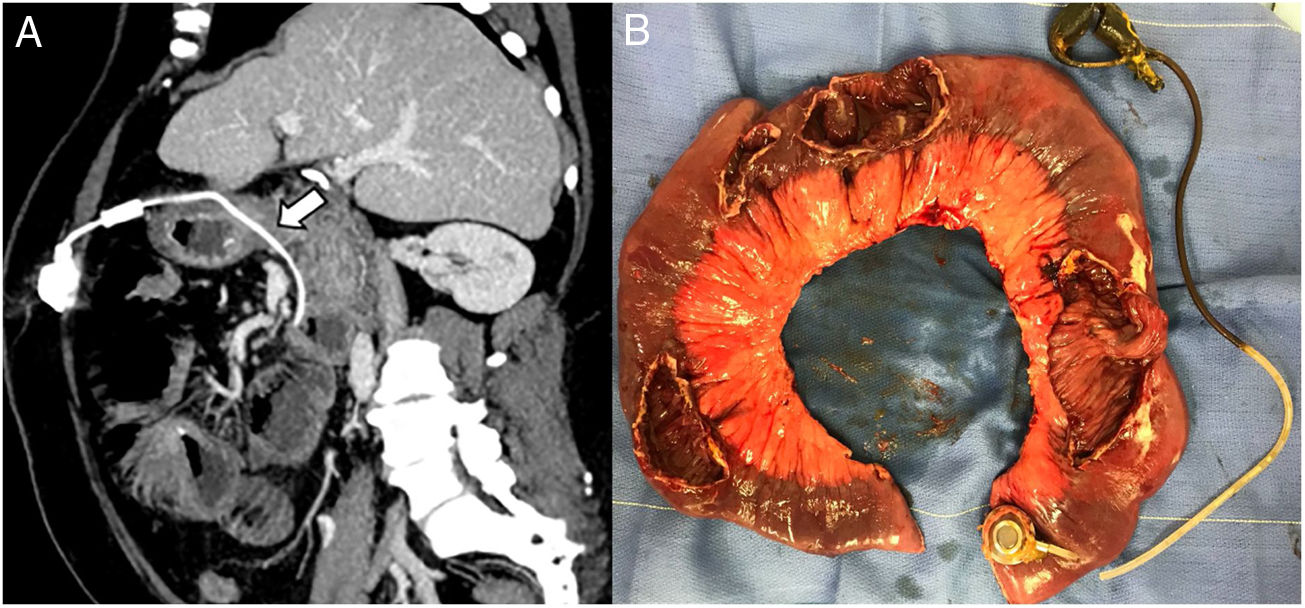
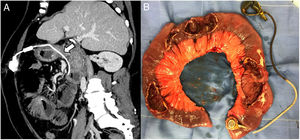
CT was performed, revealing an obstruction of the small bowel due to an intra-jejunal location of the LAGB, and no free fluid in the abdominal cavity was observed (Fig. 1a). The patient underwent an exploratory laparotomy, signs of dilation of the small bowel became apparent. An intraluminal gastric band (SAGB: Swedish Adjustable Gastric Banding, Obtech, Ethicon Endosurgery, Stockholm, Sweden, developed by Hallberg and Forsell) was found in the small bowel at 40cm from the Treitz ligament, and four more perforations were found in the proximal jejunum (Fig. 1b). The connection tubing was cut, and the band was manually extracted from the jejunum. An incision was made over the location of the subcutaneous port where the port was removed. An intestinal resection of 90cm was completed, followed by stapled side-to-side anastomosis using GIA 60 blue (Covidien, Mansfield, Massachusetts, USA). The patient had a satisfactory immediate postoperative outcome, referring only modest pain during the first post-surgical hours. Oral intake was reintroduced on the fourth day without complications. She was discharged home on the seventh postoperative day.
Erosion of the band into the gastric lumen and migration of the band out of the stomach are rare long-term complications after a gastric band placement, with an incidence of 1–14.4% on the former and less than 1% on the latter.4 Many theories have been suggested, being the primary one the pressure applied to the gastric wall. Two types of pressures are described, external and internal. The first one is applied either through overfilling of the band or too much gastric tissue insertion during the band placement. The second one is applied as a consequence of large food boluses early after operation.5 Another etiology for this complication to occur is proposed by Meir et al.6 They hypothesized that band erosion might occur more often in a laparoscopic approach because of the impossibility of using the fingers to form the retro gastric tunnel essential to place the band, causing a minuscule perforation damaging the gastric serosa; thus, resulting in a local inflammatory response with likely migration of the band. Another suggested causing factor is a rejection response against the gastric band material.5Table 1 displays all gastric band migrations, to our knowledge, reported on the literature.
Reported cases of LAGB migration to the small bowel.
| No | Reference | Sex/age | GB type/history of GB placement | Presentation/image study | Anatomic region of GB migration | Procedure |
|---|---|---|---|---|---|---|
| 1 | Taskin et al.,9 2001 | F/56 | Kuzmak ®/4 yrs | Signs of high small bowel obstruction/X-ray, CT | 4th portion-duodenum | Laparotomy+duodenorraphy |
| 2 | Bueter et al.,4 2006 | M/65 | SAGB ®/1 yr | Abdominal pain, emesis/X-ray, CT | Jejunum | Laparoscopy+gastrorraphy+jejunorraphy |
| 3 | Lantsberg et al.,7 2008 | F/58 | NA/5 yrs | Abdominal pain and vomiting/X-ray, CT | Proximal jejunum | Laparoscopy+enterotomy+jejunorraphy |
| 4 | Egbeare et al.,10 2008 | M/49 | SAGB ®/3 months | Abdominal pain and vomiting/X-ray, CT | Distal jejunum, | Laparotomy+band retrieved retrogradely+IR+PA |
| 5 | Offodile et al.,11 2010 | M/30 | LapBand ®/2 yrs | Abdominal pain, nausea and emesis/CT | 2nd portion-duodenum | Endoscopic extraction |
| 6 | Shah et al.,12 2011 | F/45 | Kuzmak ®/15 yrs | Abdominal pain, nausea and emesis/X-ray, CT | Proximal jejunum | Laparotomy+jejunorraphy |
| 7 | Bassam et al.,13 2012 | F/54 | NA/8 yrs | Abdominal pain and distension/X-ray, CT | Distal ileum | Extracted per rectum |
| 8 | Salar et al. 14 2013 | F/46 | NA/5 yrs | Abdominal pain, emesis, fever/X-ray, CT | Proximal jejunum | Laparoscopy+enterotomy+jejunorraphy |
| 9 | Sapalidis et al.,5 2013 | M/44 | LapBand ®/4 yrs | Asymptomatic/Endoscopy | Proximal jejunum | Laparotomy+IR+PA |
| 10 | Creedon et al.,2 2014 | F/41 | NA/3 yrs | RUQ pain, nausea/HIDA scan, CT | Proximal jejunum | Laparoscopy+enterotomy+jejunorraphy |
| 11 | Aguirre et al.,15 2015 | F/51 | NA/1 yr | Abdominal pain/Endoscopy, CT | Mid-ileum | Laparotomy+IR+PA |
| 12 | Abeysekera et al.,3 2017 | F/43 | NA/15 yrs | Abdominal pain and distension, nausea vomiting, obstipation/X-ray, CT | Mid-ileum | Laparotomy+IR+PA |
| 13 | Lemaire et al.,8 2017 | F/42 | NA/10 yrs | Abdominal pain in the left flank, nausea, vomiting and ileus/CT | Proximal jejunum | Laparoscopy+enterotomy+jejunorraphy |
LAGB: laparoscopic adjustable gastric band; GB: gastric band; CT: computed tomography; IR: intestinal resection; PA: primary anastomosis.
When a patient who has previously undergone LAGB insertion seeks treatment for abdominal pain, the physician should strongly consider band-related complications. Symptoms of band migration include weight regain, abdominal pain, nausea, and vomiting. An abdominal X-ray should be the first image study to perform to assess the normal gastric band position. However, CT should be considered to visualize the exact position of the band.2
The diagnosis of gastric band migration is generally made during the first three years of follow-up. Contrary to our patient, where migration of the band occurred 19 years after the LAGB initial placement. Jejunal obstruction, followed by intragastric band migration, is highly rare.7 Perforation of the jejunal wall might occur by persistent ischemic pressure ulceration.8 In our case, following erosion through the gastric wall into the lumen, the band traveled into the duodenum and then to the jejunum. As gastric erosion was slow and re-epithelialized, no signs of perforation were present at first, but the constant pressure of the band into the intestinal wall ended up perforating several segments of the jejunum. We hypothesized the band was found proximal to some perforations because the band might have moved along the gastrointestinal tract due to peristalsis. Reporting of this case will inform and alert current and future general surgeons of this LAGB complication.
Ethical considerationsThis research didn’t involve any animal experiments or human subjects.
This research has the approval of the ethics committee of Tecnologico de Monterrey institution, and it complies with the valid normative of bioethical research regulations.
Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare that they have no conflict of interest.