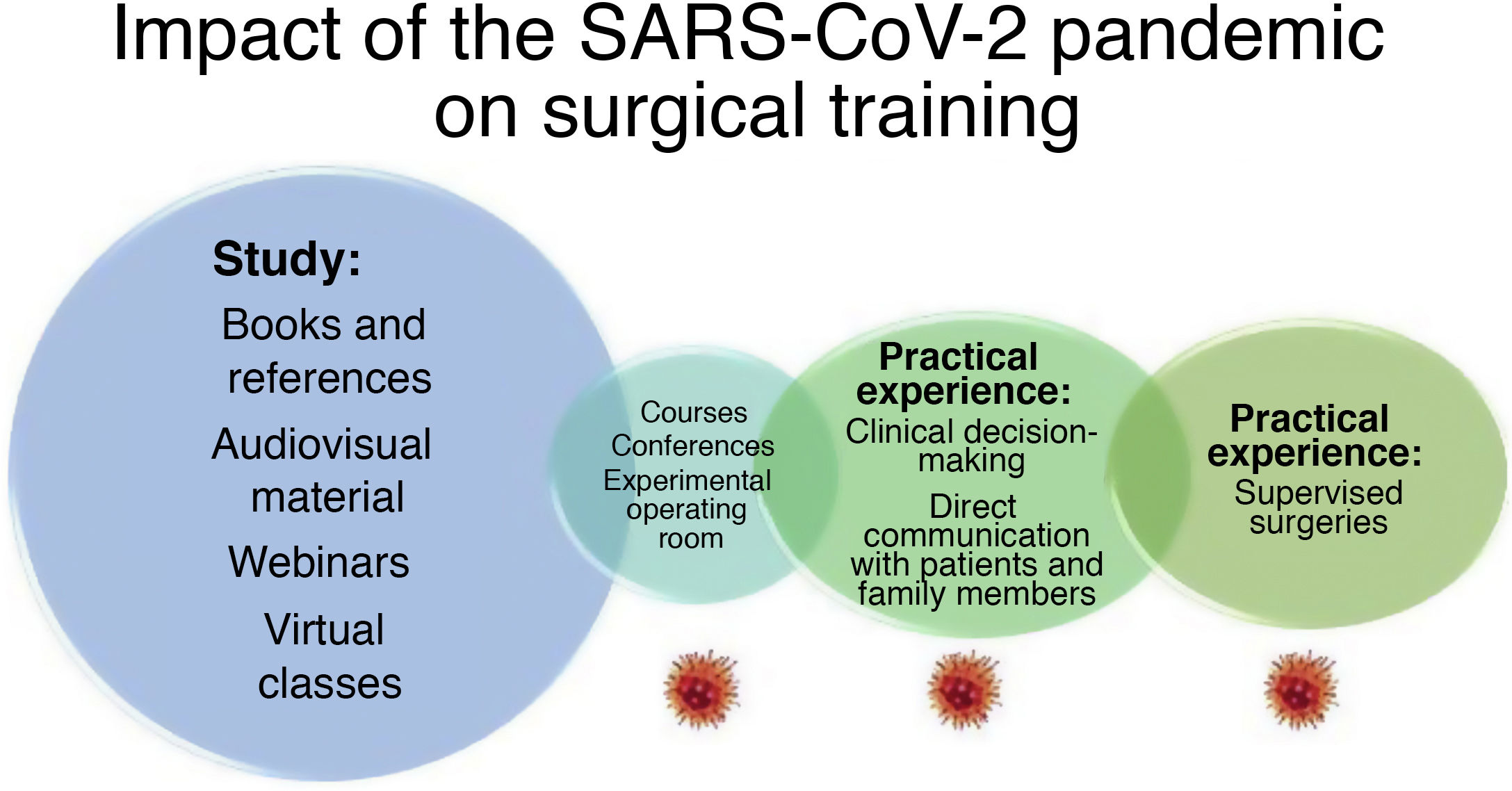
The lengthy duration of the COVID-19 pandemic has resulted in a significant loss of in-person training opportunities for surgeons. First of all, many teaching courses and in-person conferences have been canceled; in addition, the use of hospital and critical care beds and resources for patients with COVID-19 has led to a significant reduction in scheduled surgeries and, therefore, opportunities for direct learning in the operating room for resident surgeons-in-training (MIR).1 This healthcare crisis has had a significant universal psychosocial impact, causing among healthcare professionals great anxiety, fear of transmitting or contracting the disease, depression and even post-traumatic stress disorder, all of which are factors that can negatively influence their ability to learn and perhaps even leave an indelible mark on their future.2–4 Added to this is the fact that some residents and directors of surgical services have been infected by the disease and have had to spend confinements away from their daily duties.5
It is difficult to quantify the actual impact of the training opportunities lost caused by the reduction in surgical activity. It has been heterogeneous in different countries and even in different hospitals in the same country, and its significance will depend on the residents’ year of training (Fig. 1). A survey carried out in Spain and also at the European level using the DYSSA6 scale has reported that 84.4% of Spanish hospitals and 51.3% of European medical centers limited their activity to oncological and urgent surgeries, delaying the majority of benign surgeries except for preferential benign procedures at some hospitals, from March to May, 2020.6 The significant reduction in surgical training is also due to other factors, such as institutional policies that canceled training rotations in fields necessary for the comprehensive training of surgeons, the need to recruit surgical residents for the care of patients with COVID-19 in other non-surgical hospital areas.7 Added to this is the reduction in the participation of physicians-in-training in the surgeries of patients with SARS-CoV-2 due to the shortage of PPE and also to reduce the risks of infection of healthcare workers.8,9 In this regard, the residents most affected by the stoppage due to the pandemic have been years 4 and 5 MIR, as they usually have a greater supervised surgical activity. In a survey conducted by the American College of Surgeons, 84% of residents estimated a loss of more than 50% in the volume of surgical procedures and great difficulty in performing the minimum number of annual cases required for their training; 96% stated that COVID-19 has had a negative impact on their clinical experience.2 Amparore et al.10 have estimated the cancellation of at least 40% of surgical activities in urology residents-in-training in Italy during the pandemic.
The cancellation of in-person classes has also meant a significant loss of educational opportunities. In 2019, the Spanish Association of Surgeons (AEC) gave 186 in-person courses to 2106 students. In the months of March to October 2020, the 150 face-to-face courses planned with a range of themes were canceled: emergency surgery, polytrauma patient care, abdominal wall surgery, bariatric surgery, breast pathology, endoscopy, esophagogastric surgery, proctology, hepatobiliary-pancreatic surgery and transplants, mesenchymal tumors and sarcomas, endocrine surgery, etc. On top of this was the cancellation of most in-person surgery congresses, although some have been transformed to a virtual format. In this context, online training programs have been promoted, with a proliferation of seminars, webinars and virtual meetings. In addition, new proposals for more consistent virtual teaching have emerged, whose continuity have attempted to reduce losses in training.11 The AEC responded to the massive cancellation of in-person classes by proposing an ‘emergency’ teaching alternative, the ‘AEC Virtual Classroom’, and we are still discovering its potential benefits. This virtual classroom concept offers a combined format of weekly one-hour seminars, broadcast live with the options of Q&A and discussion, and educational videos on the topic of the seminar are uploaded to the virtual ‘AEC VideoAtlas’ platform. This combined format of theoretical training together with visual examples of surgical techniques has been a very well received substitute.9 From April 2020 to January 2021, 32 Virtual Classroom sessions were held, with a great reception and very substantial participation, ranging between 115 and 623 surgeons connected to each session (residents and fellows). The session format was rated positively, with an average score of 4.28/5 in satisfaction surveys, and 98% of survey participants thought that these seminars should be maintained even when in-person courses can be resumed. The AEC Virtual Classroom has turned out to be a useful surgical teaching tool that will foreseeably survive the pandemic.
In conclusion, the 2020–2021 pandemic has caused a significant loss of training opportunities for residents of our specialty. The e-learning methods, such as the AEC Virtual Classroom, with which we have tried to correct these deficiencies have been well received and have enjoyed great participation, but they do not fully compensate for the training lost.4,12 It will be essential to design new systems to evaluate training and acquired skills in order to determine whether these new teaching methods are sufficient or whether we should continue innovating in surgical teaching to prevent this SAR-CoV-2 pandemic from leaving an indelible mark on the surgeons of the future and their patients.
Please cite this article as: Sánchez Santos R, Morales Conde S, Ramos Rodriguez JL. Docencia en tiempos de crisis: Aula Virtual AEC. Impacto de COVID-19 en los cirujanos del futuro. Cir Esp. 2021;99:479–481.