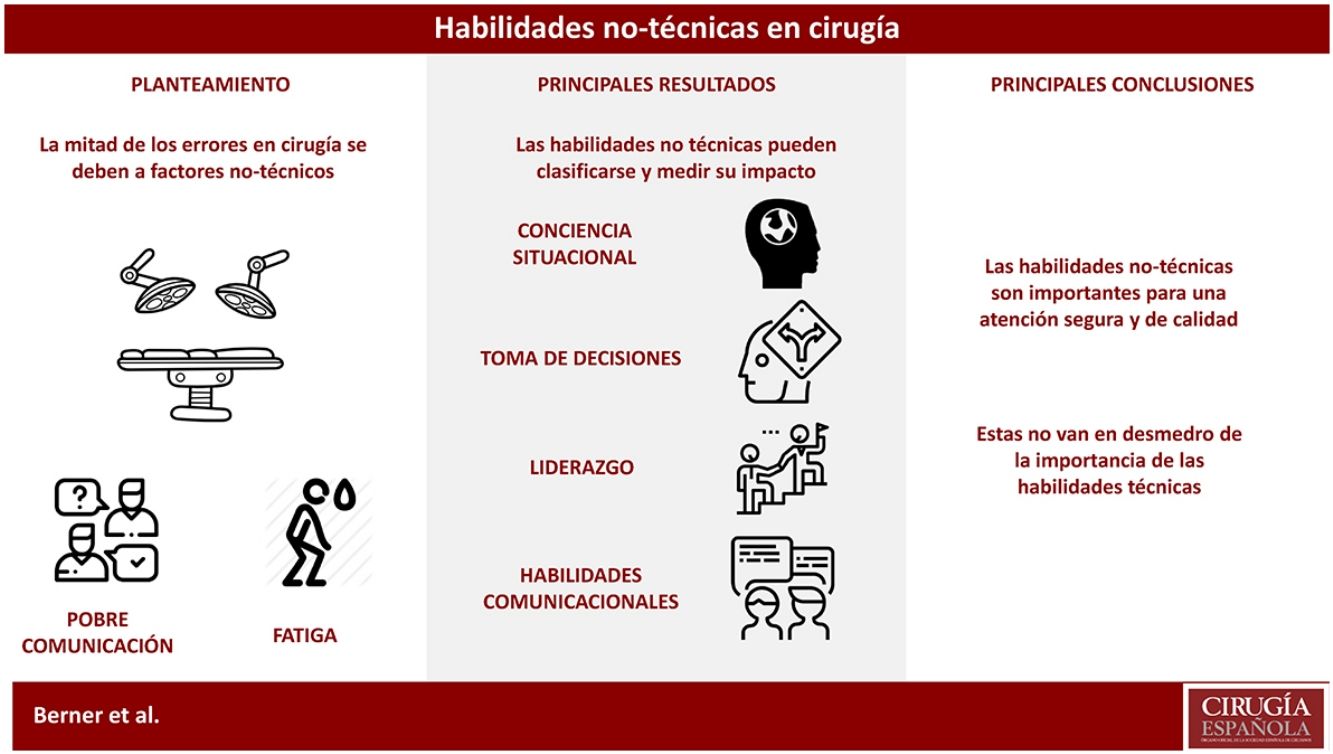
The significance of technical skills and manual dexterity for surgeons is an indisputable fact. However, the systematic study of medical errors has revealed that a significant percentage of these errors are caused by factors related to non-technical skills. The review presented in this article intends to describe and explore the relevance of these non-technical skills, including: situational awareness, decision-making, leadership and communication. In conclusion, the authors propose that adequate importance needs to be given to these aptitudes to provide safe clinical care.
La relevancia de las habilidades técnicas y la destreza manual en cirugía es un hecho indiscutible. Sin embargo, el estudio sistemático del error médico ha expuesto en las últimas décadas que una proporción relevante de estos se relacionan con carencias en habilidades no técnicas. La revisión presentada en este artículo pretende explorar la importancia de estas aptitudes, incluyendo la conciencia situacional, la toma de decisiones, el liderazgo y las habilidades comunicacionales. Como conclusión, los autores proponen que se les dé una adecuada relevancia a estos factores para fomentar una práctica clínica segura.
The current challenges of surgery differ greatly from past challenges. Advancements made in the understanding of surgical disease over the last 2 centuries have led to greater professionalization and specialization of surgical activities.1 As a result, highly complex techniques have been developed.2 However, not only have techniques become more sophisticated, but so has the entire system. Technological development has made information available to patients that they did not previously have, reducing the asymmetry in the doctor–patient relationship and empowering them to a level never before seen.3
More informed and empowered patients are able to display their dissatisfaction whenever they please. A recent study published in the United States interviewed 3988 patients about the role they play in their own health care. 34% of patients reported that their treatment goals did not coincide with those of their doctor, and 36% stated they were not satisfied with the amount of time spent with them.4 Currently, surgeons can be judged not only for their technical skills and knowledge, but also for their professional conduct; this also includes doctors-in-training.5
These circumstances have led to the development of a model of care and medical training focused on the patient.6 The concept of safe clinical practice has become a fundamental issue in undergraduate and postgraduate training programs, reflecting the intention to minimize avoidable medical errors.7
In this context, it is reasonable to ask: is technical competence alone sufficient for the challenges we face in modern surgical practice? In other words: to maximize the standard of care provided, improve the patient experience and reduce clinical errors, is technical skill the only aspect on which we should focus?8
The study of human factors related to surgery allows us to observe that providing good quality care is not reduced to the mere technical interaction between the surgeon and the patient on the operating table.9 Through systematic analysis, it is possible to uncover how the final therapeutic result is composed of a series of complex interactions between the surgeon, patient, medical team, equipment and the hospital where it takes place, influenced by a specific local culture and incentives, which in turn are part of an even larger healthcare system.10 In fact, it has been established that only 50% of surgical errors can be explained due to lack of technical skill. The other half is due to non-technical factors, such as communication problems (43%) and work overload (33%).11
Following this logic and appreciating that surgical practice is a high-risk activity, errors can be explained by understanding the interaction between environmental conditions and personal skills, both technical and non-technical.12,13 Although all of these are relevant to patient safety, it is the non-technical skills of surgeons that allow them to recognize and interact with this dynamic system.14
The objective of this article is to analyze the relevance of non-technical skills in medical practice and demonstrate how competence in surgery alone is not enough to ensure quality care. To facilitate this analysis, we will follow the Non-Technical Skills for Surgeons nomenclature, developed by the Royal College of Surgeons of Edinburgh (Table 1).15
Adapted From the Non-Technical Skills for Surgeons.
| Categories | Elements |
|---|---|
| Situation awareness | 1. Obtain information 2. Comprehend information 3. Anticipate future situations |
| Decision-making | 1. Consider options 2. Select and communicate decisions 3. Implement and review decisions |
| Leadership | 1. Establish and maintain standards 2. Handle pressure 3. Support others |
| Communication and teamwork | 1. Exchange information 2. Establish mutual understanding 3. Coordinate the team |
This cognitive ability consists of the ability of an individual to perceive relevant information both about the task being performed and the environment in which it is being developed. This information is then processed to predict possible decision outcomes and future potential scenarios.16
The surgical context usually involves the presence of different sensory stimuli, which include the movement of other team members, alarms or changes in them, feedback given by instruments, etc. This information is processed cognitively and interpreted, assigning value to the stimulus and classifying its priority.17 Knowledge and previous experience are of vital importance at this stage to differentiate which events are relevant and which are not. Finally, the prediction of scenarios based on the information obtained allows action plans and alternative approaches to be established, which are carried out in accordance with the results obtained.18
However, collecting information can be challenging. It is possible that the information is not available or difficult to obtain, such as in cases of patients with extensive clinical records or when there are technological errors that affect clinical information systems. At other times, the stimuli may not be perceived or be perceived in the wrong way. This happens, for example, when performing critical steps of a surgery where maximum attention levels are required or when there are external distractions in the operating ward.19 In Urology, for example, it has been estimated that there is a relevant distractor every 133s.19
The understanding stage, however, presents 2 fundamental problems: the “anchoring” of an idea, and confirmation bias. Anchoring is a form of cognitive bias in which the individual retains only the initial part of the information, omitting later information that could be useful. Confirmation bias, on the other hand, includes only information that confirms a preexisting hypothesis.20 Both biases restrict the projection capacity of possible future scenarios, especially when other members of the team do not participate in this cognitive process.
To reduce the number of distractors in the operating room, methods from the aeronautical industry have been proposed. The ‘sterile cockpit’ concept involves preventing the surgeon from performing parallel activities during the critical phases of a surgery, increasing the amount and quality of the information perceived.21 The implementation of this strategy in cardiac surgery has resulted in a reduction in the number of information breakdowns and critical actions not verbalized by 37% and 75%, respectively.22 In the same way, the planning and instruction of the surgical team prior to the intervention improves the understanding of the information and the prediction of eventual consequences.
Decision-makingThe ability to make decisions is defined as the set of competencies that provide adequate judgment of future situations in a scenario that offers multiple alternatives. This, in turn, can be subdivided into 3 components14:
- -
Evaluation of the situation and consideration of the alternatives
- -
Judicious choice and communication of the decision made
- -
Implementation and re-evaluation of the decision
Decision-making considers a sum of cognitive strategies to select the best option to reach an objective.23 The analytical model has historically been considered the best way to decide among different alternatives. This is based on the analysis of the information available to subsequently assess the advantages and disadvantages and thus reach a verdict.24
Although this process may seem simple, it is inevitably influenced by both internal and external factors. In addition to the previously mentioned anchoring and confirmation biases, the natural tendency to follow our instincts and feelings, simplifying binary options, may end up affecting the process. One way to address this problem is by considering the opportunity cost. Quite simply, if we opt for one option, what is the cost of not opting for the alternative? Another strategy is to consider that the preferred alternative is no longer available, forcing other options to be considered. Both methods allow for expanding the spectrum of possible solutions, which can be even more beneficial when other members of the team are included in the discussion.
Preparing for the worst of circumstances can be useful to moderate the optimism of the expected results. The old principle of always having a lifeline during a procedure can also be considered a non-technical skill.25
When there is not enough time to make decisions analytically, other cognitive strategies become important. Decisions based on orders and rules consist of a system where the operator follows a previously established protocol. Advanced trauma training or critical patient care courses train surgeons in this modality to perform safe and appropriate interventions in critical situations.26
The intuitive model, on the other hand, differs from those previously mentioned, considering that a behavior does not depend exclusively on deductive processes or pre-established protocols, but also on the ability to recognize situational patterns.27 In this manner, the focus is on previous experiences in similar situations, which saves time for developing rational abstractions. It is believed that this is how “experts” make assertive and timely decisions, moving in a continuum between analytical processes and recognition of patterns depending on the circumstances.28
LeadershipLeadership in healthcare can be defined as “the ability to lead a team, demonstrating high standards of clinical care and considering the particular needs of each team member”. To understand the role of leadership in organizations, Pendleton and Furnham have proposed an explanatory model with 3 domains, represented with primary colors in a Venn diagram.29
The strategic domain involves tasks as well as people and focuses on the future, establishing the purpose, mission, and the value and vision of the organization. It also includes the strategic direction for the interpersonal alignment of its members. Its development is fundamentally based on the creative intelligence of those responsible. The interpersonal domain develops in the present and focuses on people. It establishes the relevance of developing and maintaining relationships to direct behavior in line with the strategic direction. The operational domain focuses on achieving the objectives through the effort of the group as a whole and its problem-solving ability. In a certain way, the strategic domain can be described as the brain of an organization, the interpersonal domain as the heart, and the operational domain as the hands and legs.
Teamwork is the way in which the operational and interpersonal domains interact, recognizing the synergy of its members. In this way, group work is more than the sum of its parts. The essence of the leader in this model is in the center, where the 3 domains overlap. In this central zone, we find 5 leadership facilitators, as shown in Table 2.
Facilitators of Leadership, According to Pendleton and Furnham.
| Inspire | Both emotionally and intellectually, this is key in order to align strategies and operations |
| Focus | Maintaining a clear objective to plan and organize, establishing priorities compatible with the strategic direction and in agreement with the operational domain |
| Enable | The team, giving direction and support |
| Reinforce | With adequate incentive to maintain a good climate for performance |
| Learn | Based on collecting reliable information that can be used for continuous improvement |
As for the benefits of effective leadership in clinical practice, Suliman et al. propose that they can be classified into 4 areas30:
- 1.
Quality and safe patient care
- 2.
Improved work environment
- 3.
Efficient use of resources
- 4.
Modeling local and regional settings, influencing decision-making outside the system
Communication and teamwork promote “work as a team, ensuring that the other members share a common vision, so that they can carry out their tasks properly.”16 For this to happen, 3 consecutive tasks are necessary:
- 1.
Information transfer
- 2.
Common interpretation of the information
- 3.
Team coordination
As in the rest of the previously described skills, there are internal and external barriers to achieve effective communication. External barriers would include: noise, low voice volume, distance, time, or even the lack of visual cues, such as when masks cover facial expressions. Examples of internal factors could be, for their part: language differences, past experiences, organizational culture, mood and the relationships of everyone involved.
For example, if a surgeon is rude to a younger colleague, this will clearly influence the next time the resident wants to speak to the surgeon about a problem. Even not knowing the name of the team members can potentially discourage communication in order to avoid the uncomfortable situation of asking their names again.31
Since a significant proportion of medical errors are attributable to failed communication,11 several ideas have been proposed to address this problem. For example, the use of surgical caps with each person's name and role in the operating room to eliminate the possibility that someone will stop communicating because they have forgotten the name of another member of the team. However, we have found that the methods that have had the best results include the use of information sessions before commencing the first surgery and the use of preoperative checklists. During these, all team members have the opportunity to give their opinion and express their concerns regarding the cases in question. There is no concrete evidence that using these methods will improve the climate during surgery32; however, there is evidence that they can influence indicators like perioperative mortality.33
EvidenceDiscussing the importance of non-technical skills and their role in surgical practice can be difficult and complex, mainly because there is no consensus regarding how to describe these qualities. The Non-Technical Skills for Surgeons not only presents a conceptual proposal, but it is also a validated tool to measure these skills34 and a training curriculum.35 Residents and surgeons who have been exposed to a one-day intensive course in these subjects have repeatedly demonstrated to be more effective in solving critical situations in simulated scenarios compared with other colleagues who have not had this training.36–38 Although there is no evidence of the impact that this course may have in clinical practice, the recent validation of a patient-based results tool could facilitate research in this field.39
This methodology has been adopted outside the United Kingdom, mainly in English-speaking countries like Australia and Canada, which also have Royal Colleges of Surgeons that oversee the specialty. However, its satisfactory implementation in Japan and Denmark make its adaptation in Spanish-speaking countries more promising.40,41 Although other conceptual frameworks are available, according to a recent review of the literature on educational interventions for non-technical skills to date, the Non-Technical Skills for Surgeons would remain the taxonomy of reference.42
ConclusionBy describing this series of skills, our intention is to state that neither technical skills nor knowledge and surgical skills alone are sufficient to provide comprehensive care. It is the use of both, in addition to the understanding of the human factors that interact in surgical practice, that enable us to provide safe and satisfactory patient care. Although importance should be given to non-technical skills in surgery, 50% of the remaining errors are still associated with deficient technical skills. The essence of surgical practice continues to be technical knowledge and manual skills.
To our knowledge, there are no previously published experiences about the use of these methodologies, or similar ones, in the Spanish language. Through the publication of the Spanish version of this article, our intention is to encourage initiatives like these in our region.
The context of increasing modernization in residency and recertification programs for specialists in Spanish-speaking countries presents an opportunity to incorporate these concepts and methodologies. Once adapted to our language and organizational cultures, they could benefit not only surgeons-in-training and previously trained surgeons, but also the patients in their care.
Conflict of InterestsThe authors have no conflict of interest to declare.
Please cite this article as: Berner JE, Ewertz E. Importancia de las habilidades no técnicas en la práctica quirúrgica actual. Cir Esp. 2019;97:190–195.