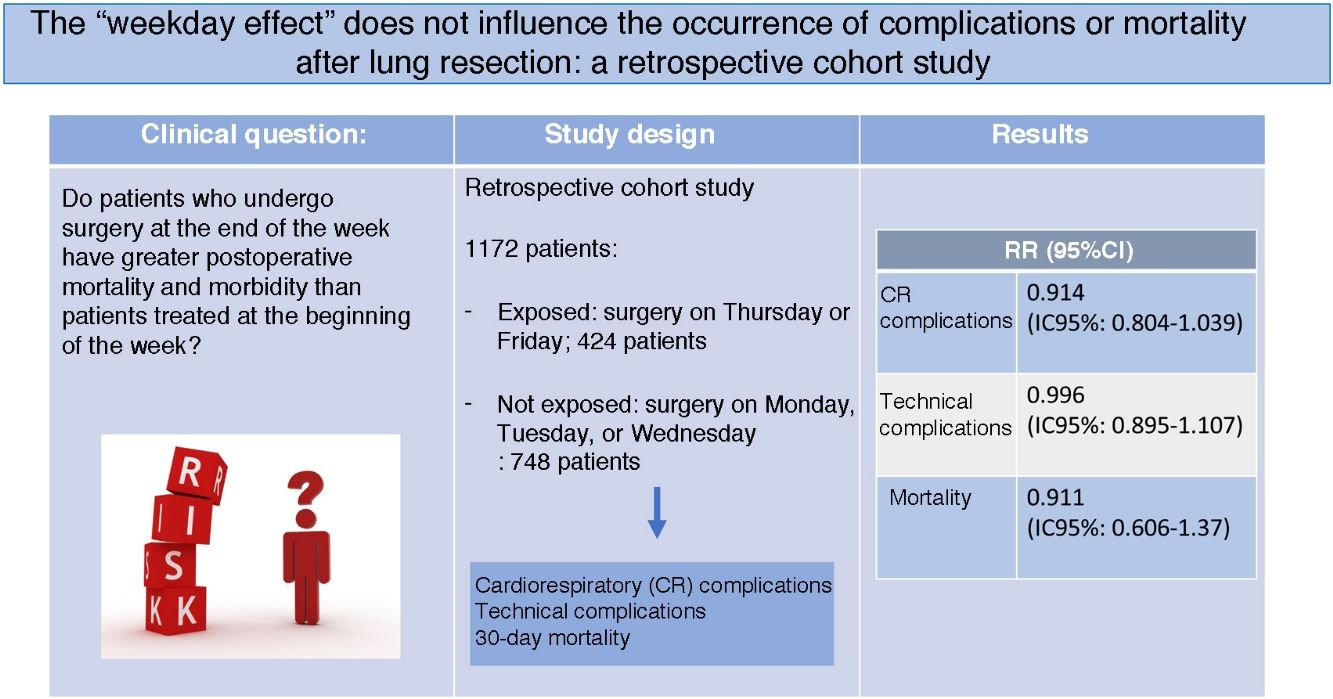
To determine whether elective anatomic pulmonary resection surgery carried out at the end of the week is associated with a higher mortality and postoperative morbidity than surgery performed at the beginning of the week.
MethodHistorical cohort study. All patients undergoing anatomical pulmonary resection between January 2013 and November 2018 in our center were included. Patients operated at the end of the week (Thursday or Friday) were considered «not exposed» and patients operated at the beginning of the week (Monday, Tuesday or Wednesday) were considered «exposed». The likelihood of cardiorespiratory complications and operative death (30 days) was compared in the two cohorts calculated using the Eurolung 1 and 2 risk models. 30-day mortality and the occurrence of cardiorespiratory and technical complications were studied as outcome variables. The incidence of these adverse effects was calculated for the overall series and for both cohorts, and the relative risk (RR) and its 95% confidence interval (95% CI) were determined.
ResultsThe overall mortality of the series was 0.9% (10/1172), the incidence of cardiorespiratory complications was 10.2% (120/1172) and that of technical complications was 20.6% (242/1172). The RR calculated for cardiorespiratory, technical complications and mortality in exposed and unexposed subjects was: 0.914 (95% CI: 0.804–1.039), 0.996 (95% CI: 0.895–1.107) and 0.911 (95% CI: 0.606–1.37), respectively.
ConclusionsPatients operated at the end of the week do not present a higher risk of postoperative adverse effects.
Determinar si la cirugía de resección pulmonar anatómica electiva llevada a cabo al final de la semana se asocia con una mayor morbimortalidad postoperatoria que la cirugía realizada al inicio de la semana.
MétodoEstudio de cohortes histórico en el que se incluyeron todos los pacientes sometidos a resección pulmonar anatómica entre el 1 de enero de 2013 y 1 de noviembre de 2018 en nuestro centro. Se consideraron «expuestos» los pacientes intervenidos al final de la semana (jueves o viernes) y «no expuestos» los intervenidos al inicio de la semana (lunes, martes o miércoles). Se comparó la probabilidad de complicaciones cardiorrespiratorias y muerte operatoria (30 días) en las dos cohortes calculada mediante los modelos de riesgo Eurolung 1 y 2. Como variables de resultado se estudiaron la mortalidad a 30 días y la ocurrencia de complicaciones cardiorrespiratorias relacionadas con la técnica postoperatoria. Se calculó la incidencia de estos efectos adversos para la serie global y para ambas cohortes y se determinó el riesgo relativo (RR) y su intervalo de confianza al 95% (IC 95%).
ResultadosLa mortalidad global de la serie fue del 0,9% (10/1.172), la incidencia de complicaciones cardiorrespiratorias fue del 10,2% (120/1.172) y la de complicaciones técnicas, del 20,6% (242/1.172). El RR calculado para las complicaciones cardiorrespiratorias, técnicas y mortalidad en expuestos y no expuestos fue: 0,914 (IC 95%: 0,804–1,039), 0,996 (IC 95%: 0,895–1,107) y 0,911 (IC 95%: 0,606–1,37), respectivamente.
ConclusionesLos pacientes intervenidos al final de la semana no presentan un mayor riesgo de efectos adversos postoperatorios.
Mortality and morbidity rates after anatomic lung resection are estimated to be 1.7% and 15.2%, respectively, according to the latest report from the European Society of Thoracic Surgeons (ESTS) based on the records of 37 463 patients included in its database from the last 5 years1. Recently, this same society has published two risk models, known as Eurolung 1 and 2, which are aimed at stratifying the risk of morbidity and mortality after anatomic lung resections2.
In recent years, a growing number of publications have documented the association between hospital admission during the weekend and the risk of mortality, known as the “weekend effect”3,4. Likewise, this effect has been documented in elective surgical procedures performed on the weekend. Glance et al.5 demonstrated that the risk of mortality and major complications after elective surgery was 3.18 and 2.11 times higher, respectively, when the surgery was carried out during the weekend versus other days of the week.
Although hospitals provide care for their patients seven days a week, non-urgent surgery is mostly performed between Monday and Friday. For this reason, some authors have focused their research on what is known as the “weekday effect”, excluding procedures performed on Saturday and Sunday. However, the results of these studies have led to contradictory conclusions6–10.
The so-called “weekday effect” refers to the increased risk of complications and postoperative mortality in patients operated on at the end of the work week compared to those operated on at the beginning. Several authors have described this circumstance6,7. In a study based on data from patients who underwent elective surgeries for any cause in English public hospitals, Aylin et al.7 showed a 44% increased risk of mortality in patients who underwent elective surgery on Friday compared to those whose surgery was on Monday. However, the “weekday effect” is a controversial and debated issue, as some studies have published opposing results8–10. In the group of patients who underwent lung resection, Aylin et al.7 found that the risk of mortality was 1.75 times higher in patients treated surgically on Friday versus those whose surgery was on Monday, while the risk was 2.66 times higher when the surgery was done over the weekend. A relevant factor that may contribute to these results is the duration of postoperative respiratory physiotherapy.
Considering that the mean postoperative stay after lung resection in our hospital is 4.3 days and that during the weekend the physiotherapy performed by patients is not supervised, patients whose surgery is on Monday benefit from an intensive, supervised and directed physiotherapy program for at least 4–5 days, while those operated at the end of the week have the help of the respiratory physiotherapist for a maximum of only one day.
Given these factors, we hypothesize that the incidence of postoperative adverse effects (cardiorespiratory complications, technical complications, and mortality) in patients undergoing anatomic lung resection at the end of the week is higher than that of patients operated on at the beginning of the week.
MethodsStudy designRetrospective cohort study.
Study populationThe study included all consecutive patients who underwent elective anatomic lung resection (segmentectomy, lobectomy, bilobectomy, or pneumonectomy) for any cause between January 1, 2013 and November 1, 2018 at our hospital. Patients who underwent atypical lung resections and those who underwent emergency surgery were excluded from the study.
The patient selection criteria were uniform throughout the study period and were based on current guidelines. The patients were treated by three surgeons with more than 15 years of experience who operated on different days of the week and two surgeons with less than 10 years of experience who conducted surgeries with the collaboration of the more expert surgeons. The surgical approach in all cases was axillary thoracotomy without axillary division or video-assisted thoracoscopic surgery (VATS). The patients were extubated in the operating room, and after about 6 h in the resuscitation unit they were transferred to the hospital ward. Postoperative analgesia consisted of an epidural catheter with bupivacaine and fentanyl in thoracotomy patients, or a paravertebral catheter with the same medication in VATS patients for 2 days, followed by paracetamol and non-steroidal anti-inflammatory drugs. Physiotherapy began the day before surgery, and exercise recommendations were maintained after the patient was discharged. From Monday to Friday, the patients performed physical exercise on a cycle ergometer under the supervision of an expert physiotherapist, who also assisted them with deep breathing maneuvers and in achieving an effective cough. In addition, patients performed shoulder and arm exercises to prevent impaired limb mobility. On the weekend, the nurses on the hospital ward encouraged patients to carry out early ambulation and to perform deep breathing maneuvers using the incentive spirometer.
Patient data were registered prospectively in an institutional database. In order to increase the quality of the data added to the registry, the thoroughness and accuracy of the data entered were controlled by a data manager at two different times: first, upon discharge of the patient from the hospital; and later, when the final histological result was included in the patient medical report. Patient data were used confidentially and in accordance with the Ethics Committee protocols at our hospital.
Variables and resultsThe results selected as dependent variables were 30-day mortality, the occurrence of cardiorespiratory complications, and the occurrence of technical complications. Mortality was defined as any death that occurred during postoperative hospital stay or within the first 30 days after surgery. Cardiorespiratory morbidity was defined as an event that occurred during admission or within 30 days after the procedure, including: respiratory failure (need for mechanical ventilation for more than 24 h or need for reintubation at any time), acute respiratory distress syndrome, atrial arrhythmia, ventricular arrhythmia, atelectasis requiring bronchoscopy, pneumonia, pulmonary thromboembolism, acute myocardial infarction, kidney failure, and cerebrovascular accident (CVA). The following complications were considered potentially related to the surgical technique: prolonged air leak (defined as the persistence of air leak through the pleural drain tube for more than 5 days after surgery), hemothorax, pneumothorax with or without air leak that required drainage, bronchial fistula, wound dehiscence, wound hematoma, empyema, chylothorax, recurrent paralysis and phrenic paralysis.
These complications were defined in advance according to the joint variable definition document published by the American (STS) and European (ESTS) Societies of Thoracic Surgeons11.
The independent variable included in the analysis was the day of the week of the operation, which defined the two patient cohorts. Patients operated on during the last two days of the week were included in the ‘exposed’ group, while patients who underwent surgery on Monday, Tuesday or Wednesday were not exposed.
Statistical analysisThe preoperative characteristics of the patients grouped according to the day of the week of the procedure were compared using the Student’s t test for quantitative variables and the chi-square test for qualitative variables.
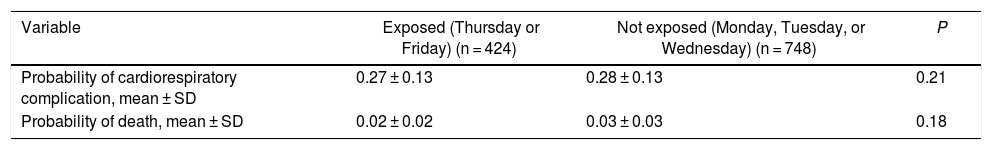
In order to determine whether both groups were comparable in terms of risk, the probability of cardiorespiratory complications and operative death (30 days) was calculated in the two cohorts using the Eurolung 1 and 2 risk models.
Estimation and comparison of the rates of cardiorespiratory complications, mortality and technical complicationsThe incidence was calculated for cardiorespiratory complications, technical complications and mortality of the global series and for both cohorts. Lastly, both groups were organized into 2 × 2 tables, and the relative risk (RR) and its 95% confidence interval (95% CI) were determined.
The statistical analysis was carried out with IBM Statistics SPSS version 22 (IBM Corp, Chicago, Illinois, 2013).
ResultsThe study included 1172 patients: 748 underwent surgery at the beginning of the week and 424 at the end of the week. The characteristics of the population can be seen in Table 1. The probabilities of cardiorespiratory complications and operative death (30 days) in the two cohorts, calculated using the Eurolung 1 and 2 risk models, are shown in Table 2.
Patient characteristics.
| Variable | Exposed (Thursday or Friday) (n = 424) | Not exposed (Monday, Tuesday, or Wednesday) (n = 748) | P |
|---|---|---|---|
| Age (yrs), mean ± SD | 65.74 ± 9.72 | 65.61 ± 10.8 | 0.84 |
| BMI, mean ± SD | 26.94 ± 4.4 | 26.38 ± 4.07 | 0.027 |
| FEV1%ppo, mean ± SD | 71.23 ± 27.96 | 69.62 ± 36.13 | 0.43 |
| Sex (men), n (%) | 290 (68.4) | 560 (74.9) | 0.021 |
| HD, n (%) | 27 (6.4) | 56 (7.5) | 0.554 |
| CVA, n (%) | 14 (3.3) | 13 (1.7) | 0.105 |
| CKD, n (%) | 16 (3.8) | 36 (4.8) | 0.462 |
| Approach (VATS), n (%) | 194 (45.8) | 356 (47.6) | 0.584 |
| Extended resection, n (%) | 39 (9.2) | 86 (11.5) | 0.238 |
| Pneumonectomy, n (%) | 14 (3.3) | 32 (4.3) | 0.439 |
CVA: cerebrovascular accident; SD: standard deviation; HD: heart disease; BMI: body mass index; CKD: chronic kidney disease; VATS: video-assisted thoracoscopic surgery; FEV1%ppo: forced expiratory volume in one second, predicted postoperative.
Probabilities of cardiorespiratory complications and operative death (30 days) in the 2 cohorts, calculated Eurolung 1 and 2 risk models, respectively.
| Variable | Exposed (Thursday or Friday) (n = 424) | Not exposed (Monday, Tuesday, or Wednesday) (n = 748) | P |
|---|---|---|---|
| Probability of cardiorespiratory complication, mean ± SD | 0.27 ± 0.13 | 0.28 ± 0.13 | 0.21 |
| Probability of death, mean ± SD | 0.02 ± 0.02 | 0.03 ± 0.03 | 0.18 |
SD: standard deviation.
The overall mortality of the series was 0.9% (10/1172), the incidence of cardiorespiratory complications was 10.2% (120/1172) and technical complications, 20.6% (242/1172).
The results of the two cohorts can be seen in Table 3. No statistically significant differences were found in terms of mortality or the incidence of cardiorespiratory or technical complications between exposed and unexposed patients.
Incidence of cardiorespiratory complications, technical complications and 30-day mortality among exposed and unexposed patients.
| Result | Risk in exposed (Thursday, Friday) (%) | Risk in unexposed (Monday, Tuesday, or Wednesday) (%) | RR (95%CI) |
|---|---|---|---|
| Cardiorespiratory complications | 37/424 (8.7) | 83/748 (11.1) | 0.914 (0.804−1.039) |
| Technical complications | 87/424 (20.5) | 155/748 (20.7) | 0.996 (0.895−1.107) |
| 30-day mortality | 3/424 (0.7) | 7/748 (0.9) | 0.911 (0.606−1.37) |
Possible mechanisms have been described that could justify the “weekday effect”12,13. For one thing, more experienced surgeons may prefer to operate earlier in the week, and they tend have better results in a wide range of surgical procedures than less experienced surgeons. On the other hand, most of the postoperative care of surgeries carried out at the end of the week is carried out during the weekend, when there are fewer staff to care for patients, fewer specialists and less availability of diagnostic and therapeutic services. The most serious postoperative complications usually occur in the first 48 h after surgery, and failure to rescue the patient could be related to these two circumstances. In patients undergoing thoracic interventions, the duration of intensive respiratory physiotherapy could be considered another predisposing factor. Although physiotherapy has proven to be useful for the prevention of pulmonary complications14–17, patients operated on during the last days of the week benefit from it for less time than those operated on at the beginning of the week.
However, the results of our study indicate that there is no difference in the occurrence of postoperative adverse effects after elective anatomic lung resections according to the day of the week on which surgery is performed. These results confirm the conclusions published by other studies in other areas, such as esophageal surgery8 or cardiac surgery9. However, they are contrary to the Aylin et al. publication7. It should be noted that their research compared the risk of mortality for each day of the week versus Monday, and that the differences were only significant for patients with surgery on Friday or during the weekend. In our study, the patients were grouped into 2 time-frames: beginning of the week (Monday, Tuesday, or Wednesday), and end of the week (Thursday or Friday), so the results are not comparable. Even so, the 30-day mortality recorded was lower in the group of patients operated on at the end of the week compared to those operated on at the beginning (0.7% vs 0.9%), although this relationship was not statistically significant.
In addition, there are no data in the literature regarding the risk of cardiorespiratory complications or the risk of complications potentially related to the surgical technique based on the day of the week of the intervention after anatomic lung resections. Although the former can be associated with the postoperative care of the patient, the latter are closely related to the procedure and surgical technique. One might think that the latter could be more prevalent in patients operated on at the end of the week due to the fatigue accumulated by the surgeon during the previous days, or because less experienced surgeons usually operate on those days. However, this statement has not been confirmed by our research and does not seem likely to influence our series, since surgeons operate indistinctly on different days of the week regardless of their level of experience. Nevertheless, although the results are not statistically significant, the incidence of both cardiorespiratory and technical complications is lower during the latter days of the week. These findings could be justified by the standardization of surgical procedures, improvements in postoperative care, and probably the inclusion of physiotherapy guidelines in both nursing care plans and preoperative patient preparation. In addition, another influence could be the tendency to schedule the most complex patients at the beginning of the week, in the hopes that they may receive more physiotherapy and for more days. Nevertheless, our data do not confirm this statement since, as shown in Table 1, no statistically significant differences were found between the two cohorts in the risk of complications or postoperative mortality, as calculated with the Eurolung 1 and 2 models.
Study limitationsThe main limitation of our study is that the level of experience of the surgeons who performed the surgeries on the different days of the week was not analyzed. We do not believe that this circumstance influenced our results, since the five surgeons operated indistinctly throughout the week, and the less experienced surgeons benefitted from the collaboration with the most expert surgeons. Nevertheless, it is true that the surgeon’s level of experience may be relevant at other hospitals.
Furthermore, this study may have biases inherent to any retrospective analysis. Although the complications were well defined and the variables standardized15, we cannot rule out that there may have been data entry errors, mistaken classifications, or insufficient information.
ConclusionsPatients who undergo surgery at the end of the week do not present a greater risk of postoperative adverse effects, despite having fewer days of intensive respiratory physiotherapy. This is probably due to the inclusion of physiotherapy guidelines in care plans and the preoperative preparation of patients.
FundingThis study has received no specific funding from public, private or non-profit organizations.
Conflict of interestsThe authors have no conflict of interests directly or indirectly related with the content of this manuscript.
Please cite this article as: Gómez Hernández MT, Novoa Valentín N, Rodríguez Alvarado I, Fuentes Gago M, Aranda JL, Jiménez López MF. El «efecto día de la semana» no tiene impacto en la aparición de complicaciones o mortalidad tras la resección pulmonar: estudio de cohortes histórico. Cir Esp. 2021;99:296–301.