To analyse the outcomes of laparoscopic versus open repair for perforated peptic ulcers (PPU).
MethodsAll patients undergoing PPU repair between January 2002 and March 2012 were included in the study. Demographic characteristics, operation time, complications, and length of hospital stay were evaluated.
ResultsTwo hundred and twelve patients (median age, 49 years) were included, 60 in the laparoscopic group and 52 in the open group. Patients operated laparoscopically were significantly younger and had a higher consumption of tobacco, alcohol and cannabis. Median acute symptoms time was shorter in the laparoscopic group (6h) compared to the open group (12h; P=.025) Symptoms time was shorter in the laparoscopic group. Median operating time was significantly longer in the laparoscopic group (104.5min vs. 76min, P=.025). The percentage of conversion to open repair was 25%. There was no difference in morbidity between 2 groups, but there were 3 deaths in the open group. Median hospital stay was significantly shorter in patients treated laparoscopically when compared with the open group (6 days vs. 8 days; P=.041).
ConclusionLaparoscopic and open repair are equally safe in the management of PPU. A shorter hospital stay can be achieved in the laparoscopic group.
Analizar los resultados del abordaje quirúrgico laparoscópico frente al abierto en el tratamiento de las úlceras pépticas perforadas (UPP).
Pacientes y métodosEstudio retrospectivo de todos los pacientes operados de una UPP durante el periodo enero de 2002-marzo de 2012. Se analizaron datos demográficos, tiempo operatorio, complicaciones y estancia hospitalaria.
ResultadosSe incluyó a 112 pacientes (mediana, 49 años), 60 en el grupo laparoscópico y 52 en el grupo abierto. Los pacientes operados por vía laparoscópica eran significativamente más jóvenes y tenían un mayor consumo de tabaco, alcohol y cannabis. La mediana de duración de los síntomas agudos fue menor en los pacientes del grupo laparoscópico (6 h) en comparación con los del grupo abierto (12 h). La mediana del tiempo operatorio fue significativamente mayor en los pacientes del grupo laparoscópico (104,5 vs 76 min; p = 0,025). El porcentaje de conversión a cirugía abierta fue del 25%. La morbilidad fue similar en ambos grupos, pero 3 pacientes fallecieron en el grupo abierto. La mediana de estancia hospitalaria fue significativamente menor en el grupo laparoscópico (6 vs 8 días; p = 0,041).
ConclusiónEl abordaje por vía laparoscópica es una técnica segura y comparable a la cirugía abierta en el tratamiento de la UPP, con la que el paciente se beneficia de una estancia hospitalaria más corta.
Although the need for elective surgery for peptic ulcer has decreased after the addition of proton pump inhibitors (PPIs) and Helicobacter pylori (Hp) eradication to treatment, the incidence and mortality of perforated peptic ulcer (PPU) remain at 5%–10%.1,2 At present, the most common surgery for PPU is simple closure, combined with an effective medical treatment for Hp eradication. In 1990, Mouret et al.3 published the first results of laparoscopic repair of PPU and concluded that it was an acceptable method. Thereafter, 3 randomised trials and one meta-analysis have demonstrated that laparoscopic closure of PPU is viable and safe compared with open repair.4–12 In Spain, only 1 case series has been published, and no study is available comparing laparoscopic versus open repair of PPU.13
The aim of this investigation was to compare the outcomes of laparoscopic versus open repair of PPU in a university hospital.
MethodsPatientsMedical records of all patients who underwent PPU surgery at the Hospital del Mar-University Hospital between January 2002 and March 2012 were evaluated. The patients were operated on by a staff surgeon or by a resident doctor under the supervision of a staff surgeon. The decision to perform laparoscopic or open repair was left to the discretion of the staff surgeon, based on his expertise in minimally invasive surgery. Patients who had evidence of gastrointestinal bleeding preoperatively were excluded from the study.
Study VariablesThe following data were collected: age, sex, duration of symptoms, tobacco consumption, alcohol consumption, use of nonsteroidal anti-inflammatory drugs (NSAIDs), consumption of cocaine and its derivatives, consumption of cannabis and its derivatives, comorbidities, surgical risk classification according to the American Society of Anaesthesiologists (ASA),14 Boey score,15 previous abdominal surgery, heart rate on admission, shock on admission (systolic pressure <80mmHg), number of leukocytes in the blood count on arrival at the hospital, evidence or absence of free air on plain radiographs and computed tomography (CT), type of surgery (laparoscopic or open repair), type of repair performed on the perforation, operating time (defined as the time from initial skin incision to closure), operation room occupancy time (defined as the time from entry into the operating room until exit), location of the perforation, perforation size, necessity for conversion to open repair, complications and their classification according to Clavien-Dindo,16 nasogastric tube use duration during the postoperative period, time of resumption of oral intake, and length of hospital stay.
Statistical AnalysisData were analysed according to the intention-to-treat principle. The data are expressed as medians with minimum and maximum ranges for quantitative variables and as absolute and relative frequencies for qualitative variables. Categorical variables are expressed as numbers and percentages. Student's t test was used to compare continuous variables. Binary and categorical variables were evaluated with Pearson's 2-tailed test, the Chi-squared test with Yates correction, or Fisher's exact test. The Mann–Whitney U test was used for other nonparametric quantitative data. P values <.05 were considered statistically significant. The Statistical Package for the Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis.
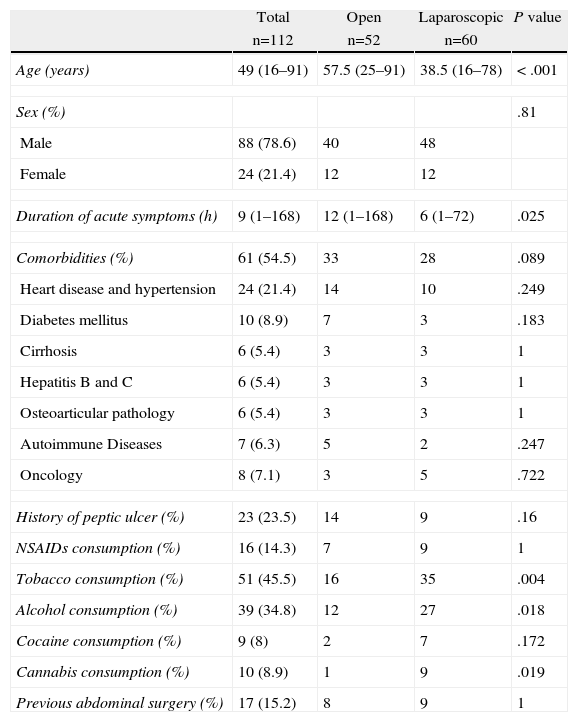
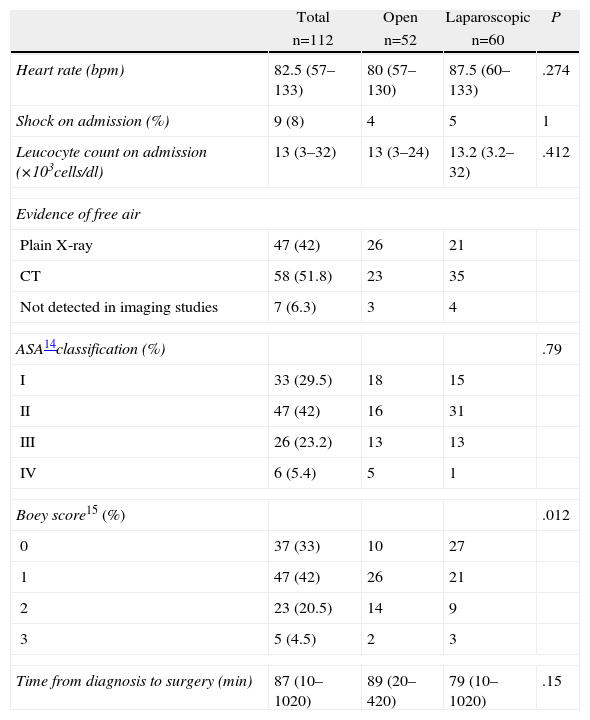
ResultsDemographic and Clinical DataOne hundred and twelve patients underwent PPU surgery during the study period: 52 with open repair and 60 with laparoscopic repair. There was a constant frequency of 11 cases per year, with predominance in March, July, and December. Demographic features of the 2 groups are listed in Table 1. Patients undergoing laparoscopic surgery were significantly younger; their duration of acute symptoms leading to surgery was shorter; and their tobacco, alcohol, and cannabis consumption was greater. Table 2 presents the clinical data of the patients on admission to the emergency department. No significant differences were observed between the 2 groups, except for a greater number of patients with scores of 0 and 1 on the Boey scoring system among those individuals undergoing laparoscopic surgery.
Demographic and Clinical Features.
| Total | Open | Laparoscopic | P value | |
| n=112 | n=52 | n=60 | ||
| Age (years) | 49 (16–91) | 57.5 (25–91) | 38.5 (16–78) | < .001 |
| Sex (%) | .81 | |||
| Male | 88 (78.6) | 40 | 48 | |
| Female | 24 (21.4) | 12 | 12 | |
| Duration of acute symptoms (h) | 9 (1–168) | 12 (1–168) | 6 (1–72) | .025 |
| Comorbidities (%) | 61 (54.5) | 33 | 28 | .089 |
| Heart disease and hypertension | 24 (21.4) | 14 | 10 | .249 |
| Diabetes mellitus | 10 (8.9) | 7 | 3 | .183 |
| Cirrhosis | 6 (5.4) | 3 | 3 | 1 |
| Hepatitis B and C | 6 (5.4) | 3 | 3 | 1 |
| Osteoarticular pathology | 6 (5.4) | 3 | 3 | 1 |
| Autoimmune Diseases | 7 (6.3) | 5 | 2 | .247 |
| Oncology | 8 (7.1) | 3 | 5 | .722 |
| History of peptic ulcer (%) | 23 (23.5) | 14 | 9 | .16 |
| NSAIDs consumption (%) | 16 (14.3) | 7 | 9 | 1 |
| Tobacco consumption (%) | 51 (45.5) | 16 | 35 | .004 |
| Alcohol consumption (%) | 39 (34.8) | 12 | 27 | .018 |
| Cocaine consumption (%) | 9 (8) | 2 | 7 | .172 |
| Cannabis consumption (%) | 10 (8.9) | 1 | 9 | .019 |
| Previous abdominal surgery (%) | 17 (15.2) | 8 | 9 | 1 |
NSAIDs: Nonsteroidal anti-inflammatory drugs.
Clinical Data on Admission.
| Total | Open | Laparoscopic | P | |
| n=112 | n=52 | n=60 | ||
| Heart rate (bpm) | 82.5 (57–133) | 80 (57–130) | 87.5 (60–133) | .274 |
| Shock on admission (%) | 9 (8) | 4 | 5 | 1 |
| Leucocyte count on admission (×103cells/dl) | 13 (3–32) | 13 (3–24) | 13.2 (3.2–32) | .412 |
| Evidence of free air | ||||
| Plain X-ray | 47 (42) | 26 | 21 | |
| CT | 58 (51.8) | 23 | 35 | |
| Not detected in imaging studies | 7 (6.3) | 3 | 4 | |
| ASA14classification (%) | .79 | |||
| I | 33 (29.5) | 18 | 15 | |
| II | 47 (42) | 16 | 31 | |
| III | 26 (23.2) | 13 | 13 | |
| IV | 6 (5.4) | 5 | 1 | |
| Boey score15 (%) | .012 | |||
| 0 | 37 (33) | 10 | 27 | |
| 1 | 47 (42) | 26 | 21 | |
| 2 | 23 (20.5) | 14 | 9 | |
| 3 | 5 (4.5) | 2 | 3 | |
| Time from diagnosis to surgery (min) | 87 (10–1020) | 89 (20–420) | 79 (10–1020) | .15 |
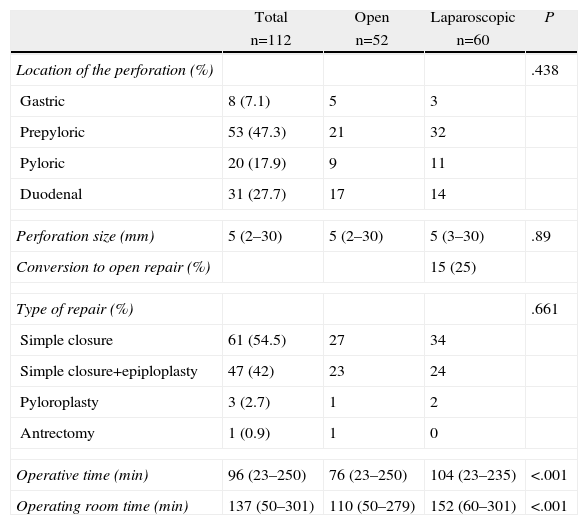
Analysis of the surgical variables (Table 3) revealed no significant differences in the location and size of the perforations. Virtually all patients underwent simple closure of the ulcer, with or without associated omentoplasty. The operating time and operating room occupancy time were significantly longer in the laparoscopic group. The laparoscopic procedure was completed in 45 patients, and 15 (25%) patients required conversion to an open repair for the following reasons: difficulty identifying the perforation site (11 cases), friable ulcer edges (3 cases), and 1 case with a 30mm ulcer diameter.
Surgical Data.
| Total | Open | Laparoscopic | P | |
| n=112 | n=52 | n=60 | ||
| Location of the perforation (%) | .438 | |||
| Gastric | 8 (7.1) | 5 | 3 | |
| Prepyloric | 53 (47.3) | 21 | 32 | |
| Pyloric | 20 (17.9) | 9 | 11 | |
| Duodenal | 31 (27.7) | 17 | 14 | |
| Perforation size (mm) | 5 (2–30) | 5 (2–30) | 5 (3–30) | .89 |
| Conversion to open repair (%) | 15 (25) | |||
| Type of repair (%) | .661 | |||
| Simple closure | 61 (54.5) | 27 | 34 | |
| Simple closure+epiploplasty | 47 (42) | 23 | 24 | |
| Pyloroplasty | 3 (2.7) | 1 | 2 | |
| Antrectomy | 1 (0.9) | 1 | 0 | |
| Operative time (min) | 96 (23–250) | 76 (23–250) | 104 (23–235) | <.001 |
| Operating room time (min) | 137 (50–301) | 110 (50–279) | 152 (60–301) | <.001 |
Regarding the immediate postoperative period data, no significant differences were observed in the time of nasogastric tube use (48 vs 48h) or the time of resumption of oral intake (72 vs 72h). The median hospital stay was 8 (3–50) days for the open repair group and 6 (3–40) days in the laparoscopic group; this difference was statistically significant (P=.04).
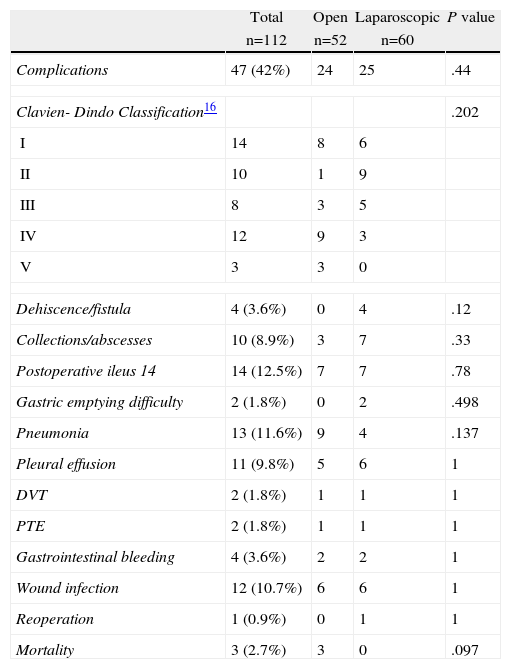
Morbidity and MortalityTable 4 summarises the complications in both groups. No statistically significant differences were found in any of the variables analysed. Four patients in the laparoscopic group had evidence of suture leak. Three cases resolved with medical treatment including antibiotics, percutaneous drainage, and total parenteral nutrition (TPN), but 1 patient needed reoperation and underwent antrectomy with Roux-en-Y gastrojejunostomy anastomosis. Three deaths were observed in the open repair group. The first patient died of a massive pulmonary thromboembolism; the second died of multiple organ failure after presenting severe sepsis of respiratory origin; and the last patient was in shock on admission to the hospital, was subsequently intubated, and died within the first 24h postoperatively.
Morbidity and Mortality.
| Total | Open | Laparoscopic | P value | |
| n=112 | n=52 | n=60 | ||
| Complications | 47 (42%) | 24 | 25 | .44 |
| Clavien- Dindo Classification16 | .202 | |||
| I | 14 | 8 | 6 | |
| II | 10 | 1 | 9 | |
| III | 8 | 3 | 5 | |
| IV | 12 | 9 | 3 | |
| V | 3 | 3 | 0 | |
| Dehiscence/fistula | 4 (3.6%) | 0 | 4 | .12 |
| Collections/abscesses | 10 (8.9%) | 3 | 7 | .33 |
| Postoperative ileus 14 | 14 (12.5%) | 7 | 7 | .78 |
| Gastric emptying difficulty | 2 (1.8%) | 0 | 2 | .498 |
| Pneumonia | 13 (11.6%) | 9 | 4 | .137 |
| Pleural effusion | 11 (9.8%) | 5 | 6 | 1 |
| DVT | 2 (1.8%) | 1 | 1 | 1 |
| PTE | 2 (1.8%) | 1 | 1 | 1 |
| Gastrointestinal bleeding | 4 (3.6%) | 2 | 2 | 1 |
| Wound infection | 12 (10.7%) | 6 | 6 | 1 |
| Reoperation | 1 (0.9%) | 0 | 1 | 1 |
| Mortality | 3 (2.7%) | 3 | 0 | .097 |
PTE: pulmonary thromboembolism; DVT: deep vein thrombosis.
This study demonstrates that laparoscopic PPU repair is safe and viable, and presents a significant reduction in hospital stay. However, these conclusions must be considered in the context of the study design. This is not a prospective randomised trial but a retrospective study of 2 contemporary cohorts who underwent either technique at the discretion of the surgical team, based on their experience. The thoroughness of the data review is a strong point of this study because the hospital has an electronic medical record system with access to patient data from primary care centres.
The population included in this study, considered as a whole, does not differ from the populations in other publications analysing different aspects of PPU, and particularly does not differ from the populations of the 2 latest reviews published in 2010.17,18 The usual patients would be 50-year-old males, of whom only one-quarter have a history of ulcer, but they most likely have some type of comorbidity and the associated consumption of toxic substances such as tobacco, alcohol, or even illicit drugs. If we refer to the time when the patient comes to the emergency room, we would be encountering a patient with a low risk score (according to the ASA and Boey classifications), tachycardia, and leukocytosis. As reported in other publications,19 very few patients are in shock on admission. It is striking that in our study, unlike other publications,20,21 the presence of pneumoperitoneum—one of the most important features for confirming the diagnosis—was present in less than one-half of patients using plain radiography. However, with the addition of CT, this finding rose to 93%, which is superior to other studies.19 Some differences were observed, most likely inherent to the study design, when studying the cohorts undergoing conventional or laparoscopic repair. Patients were significantly younger in the laparoscopic group, with less comorbidity, and had increased alcohol, tobacco, and drug consumption, which was most likely related to their youth. Furthermore, these patients’ Boey scores and duration of the symptoms precipitating their emergency department visits were significantly lower.
From the surgical point of view, the patients underwent surgery 90min after diagnosis, usually presented prepyloric ulcers, and simple closure with or without omentoplasty was performed in the vast majority; no statistically significant differences were found between the 2 groups, except that the operating times and operating room utilisation were significantly higher among patients in the laparoscopic group. It is notable that the statistical analysis of this study was conducted under the “intention-to-treat” principle. Because 25% of patients for whom the surgery was started laparoscopically required conversion to open repair, this factor might have influenced the observed differences.
The overall mortality in this study was less than 3%, which was much lower than in other recent series reaching 6%–18%.22–24 Four factors that could increase this rate up to 100% have been described: age >60 years, delayed treatment (>24h), shock on admission, and concomitant diseases.25,26 The mortality is also 2 or 3 times higher in patients with gastric perforations.25,27 Considering some of these variables, Boey et al.15 proposed a risk score that has been corroborated by other authors.1,28–30 It is remarkable that all of the mortality occurred in the group of patients undergoing open surgery in our study, but after analysing the causes, it is difficult to relate this finding to the surgical approach.
As in other studies, the most common complications after the PPU surgery were paralytic ileus, respiratory infections, and surgical wound infections. However, no differences were found in the postoperative morbidity globally analysed by the Clavien-Dindo classification or examined in detail for each of the complications between the 2 groups of patients. In a specific analysis, it is striking that all suture leaks occurred in the laparoscopic surgery group. It is likely that this increased incidence might be related to the difficulty of the laparoscopic procedure, which emphasises the requirement for a surgeon experienced in minimally invasive surgery to perform this procedure. In our centre, simple closure is the technique of choice, with or without omentoplasty. Some authors have tried sutureless techniques using fibrin glue or gelatin sponge, but the usefulness would perhaps be limited to small perforations.6,19
In conclusion, the PPU laparoscopic surgical treatment is safe and provides several advantages over open repair.
Conflict of InterestThe authors have no conflict of interest to declare.
To the Academic Mobility Programme of the Postgraduate Iberoamerican University Association and St. Thomas Hospital in the Republic of Panama for financial support during the training of Dr. Gerardo Dominguez-Vega in Barcelona. To all surgical teams of the Surgery Service at the Hospital del Mar-University Hospital who contributed to the treatment of these patients. To Sergi Mojal from the Statistics Unit of Hospital del Mar Medical Research Institute (IMIM, for its initials in Catalan) for assisting with the statistical analyses.
Please cite this article as: Domínguez-Vega G, Pera M, Ramón JM, Puig S, Membrilla E, Sancho J, et al. Tratamiento quirúrgico de la úlcera péptica perforada: comparación entre los abordajes laparoscópico y abierto. Cir Esp. 2013;91:372–377.