Paragangliomas are tumors that originate from extra-adrenal chromaffin cells that can secrete catecholamines.1,2 They typically present with hypertension and tachycardia, while presentation with cardiogenic shock is rare.3
We present the clinical case of a 14-year-old male with no history of interest, who came to the emergency department for abdominal pain, headache and oppression of the chest. During his stay in the emergency department, his condition worsened and he developed cardiogenic shock, requiring orotracheal intubation and noradrenaline at 0.2 mcg/kg/min to stabilize. An urgent echocardiogram showed evidence of severe left ventricular dysfunction and generalized hypokinesia. Given the patient’s clinical situation, he was considered a candidate for arteriovenous extracorporeal membrane oxygenation (ECMO) therapy. With a suspected diagnosis of fulminant myocarditis, he received empirical treatment with acyclovir, meropenem, linezolid, doxycycline and nonspecific IgG.
During his stay in Intensive Care, serial echocardiography showed progressive normalization, and withdrawal of the ECMO system was possible on the fifth day.
Afterwards, the patient began to experience abdominal pain. Thoracoabdominal CT scan revealed 2 retroperitoneal masses: one measuring 3.6×3.7 cm next to the head of the pancreas, and a second mass measuring 3.1×4.6 cm near the right diaphragm, posterior to the right crus at the origin of the celiac trunk, as well as multiple retroperitoneal lymphadenopathies.
Laboratory values of metanephrine, normetanephrine and plasma chromogranin A were 16 pg/mL, 380 pg/mL and 219 ng/mL, respectively.
Given the suspicion of a catecholamine-producing tumor, alpha blockade was started with doxazosin (4 mg every 8 h), followed by beta blockade with labetalol (400 mg every 12 h).
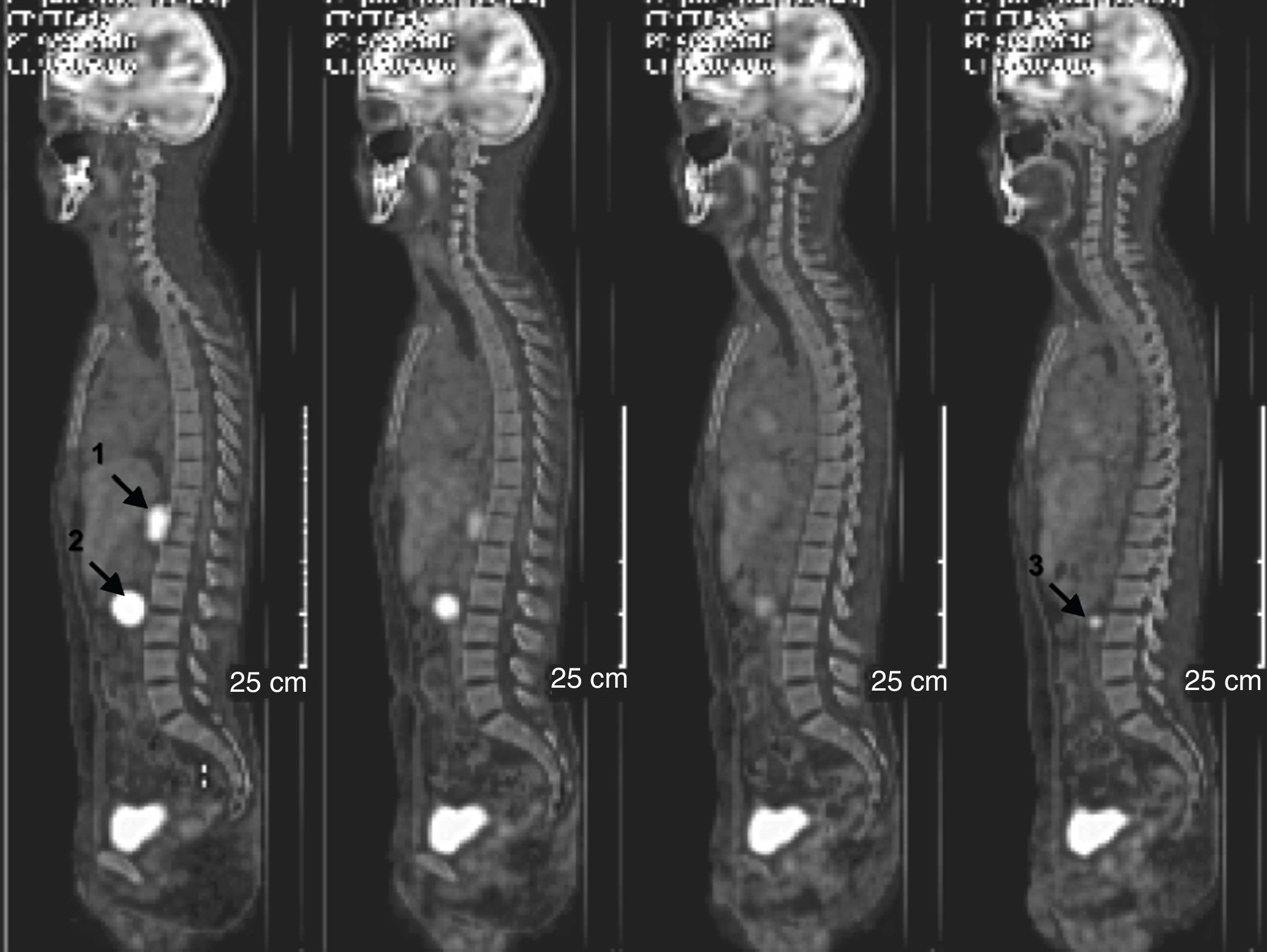
The I-123-MIBG (Iodine-123-metayodobenzylguanidine) scintigraphy showed pathological uptake of two retroperitoneal functioning lesions, identical to those of the CT scan. PET/CT (Fig. 1) confirmed both masses (the retrocrural with an SUV of 19.2, and the peripancreatic with an SUV of 31.5) and also revealed a third retroperitoneal pathological focus in the left para-aortic space. A Tru-cut biopsy of the retroperitoneal mass confirmed the diagnosis of paraganglioma.
Total body PET/CT scan showing three masses with malignant behavior (arrows): (1) right retrocrural mass (SUVmax 19.2); (2) retroperitoneal mass below the head of the pancreas (SUV max 31.5); (3) pathological retroperitoneal focus (SUV max 7.9; 8.3 mm) in the left para-aortic space.
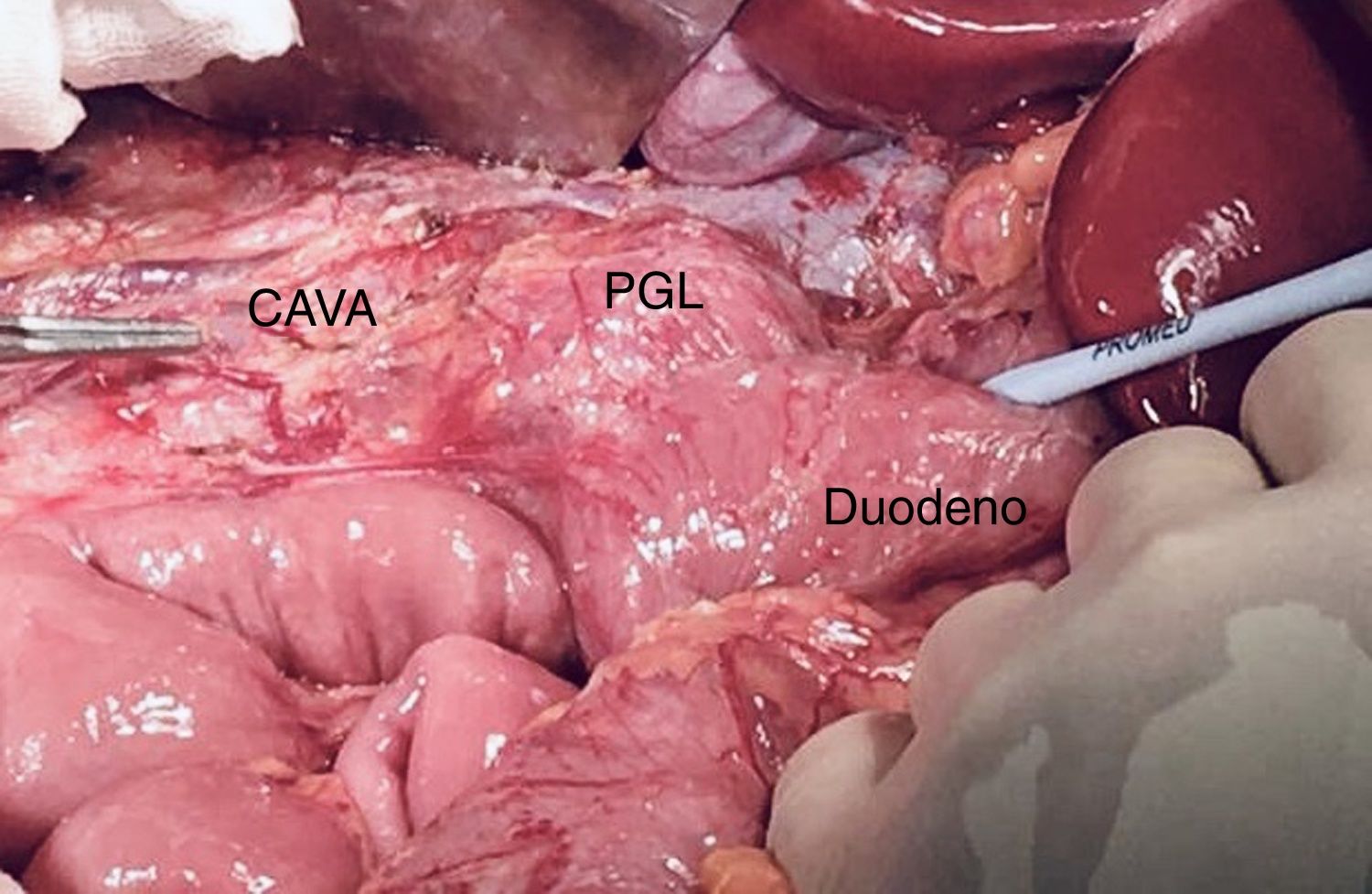
After preoperative optimization with alpha-beta blockade using doxazosin and labetalol, the patient was treated surgically (Fig. 2), with excision of the 3 retroperitoneal masses and interaortocaval lymphadenectomy as well as distal lymph node sampling (iliac lymphadenopathy and mesenteric lymphadenopathy). The patient remained hemodynamically stable throughout the intervention.
The histological and immunohistochemical study (chromogranin, synaptophysin, and S100) was compatible with triple paraganglioma (retrocaval, retropancreatic, and interaortocaval), showing no evidence of metastasis in the lymphadenectomy specimen.
The patient progressed favorably and was discharged 10 days after surgery. During follow-up, the patient presented a tumor recurrence in the form of bone metastases 21 months later.
Paragangliomas are rare tumors in childhood and adolescence, representing 20% of all cases.4 As 80% are benign and sporadic, their slow growth and the production of inactive metanephrine can delay their diagnosis. Symptoms are related to catecholamine secretion, such as hypertension, palpitations, sweating, headache, or dizziness. Cardiac involvement in the form of acute infarction, heart failure, myopathies or arrhythmias is less frequent.3 In a series of 202 paragangliomas, Giavarini et al. observed catecholamine cardiomyopathy in 15 patients, only 1 of whom was diagnosed before the ventricular dysfunction episode occurred.5
Our case is exceptional due to the association of several singularities: functioning multiple paraganglioma, onset in childhood and debut as cardiogenic shock.
The use of ECMO therapy in refractory cardiogenic shock secondary to functional paragangliomas is anecdotal in the literature, and it is mainly described in pheochromocytomas in adults.6 With the use of ECMO, our patient experienced a complete reversal of the echocardiographic pattern of cardiac failure, presenting a favorable clinical evolution.
Although our patient’s elevated plasma metanephrine and chromogranin levels directed the presumptive diagnosis, the use of adrenaline and noradrenaline for the treatment of shock may cause false positives.
The importance of the combination of CT scan and scintigraphy in the localization of paragangliomas is evident in our case. The initial suspicion of lymphoma on CT scan was modified after MIBG scintigraphy showed two lesions compatible with paragangliomas. Meanwhile, the subsequent PET/CT scan revealed a third lesion that had gone unnoticed, thereby showing its diagnostic superiority and value in the extension study of these tumors.
Malignancy criteria are determined by the presence of metastasis or local invasion of adjacent structures. In our case, no distant metastases were initially evident on imaging tests or in the pathology results of the surgical specimens. During follow-up, malignant behavior was confirmed when bone metastases appeared 21 months after the procedure. In these cases, 5-year survival is 78%, and 10-year is 31%.7
Using ECMO for the intensive management of cardiogenic shock secondary to a functioning paraganglioma can initially save the patient’s life. Surgical resection of all lesions, with previous alpha and beta blockade, is the only alternative with a curative intent.
Please cite this article as: Acosta-Mérida MA, Silvestre-Rodríguez J, Hernández-Ramírez JM, Godoy C, Marchena-Gómez J. Shock cardiogénico como debut de triple paraganglioma retroperitoneal en varón de 14 años. Cir Esp. 2020;98:362–364.