Vascular injury secondary to a suture is an uncommon but potentially serious situation in femoral hernia surgery. It normally occurs on the femoral vein (FV), and it is rare for it to occur on the femoral artery (FA).1
We present a case of acute ischemia of the lower limb after femoral hernia repair.
The patient is a 54-year-old woman, with no relevant clinical history. She presented an uncomplicated right femoral hernia, which was treated as outpatient surgery using an anterior approach. A Lichtenstein hernia repair was performed with cylindrical polypropylene mesh fixed with one polypropylene n 0 stitch to the lower side of the inguinal ligament; the procedure apparently proceeded without incident. 72h after the procedure, the patient reported coldness, paresthesia and progressive functional limitation of the ipsilateral lower limb. On examination, no pulses were palpable, she presented limited dorsiflexion of the foot (grade 0 of the Medical Research Council [MRC] muscle strength scale, paresthesia and decreased distal sensitivity.
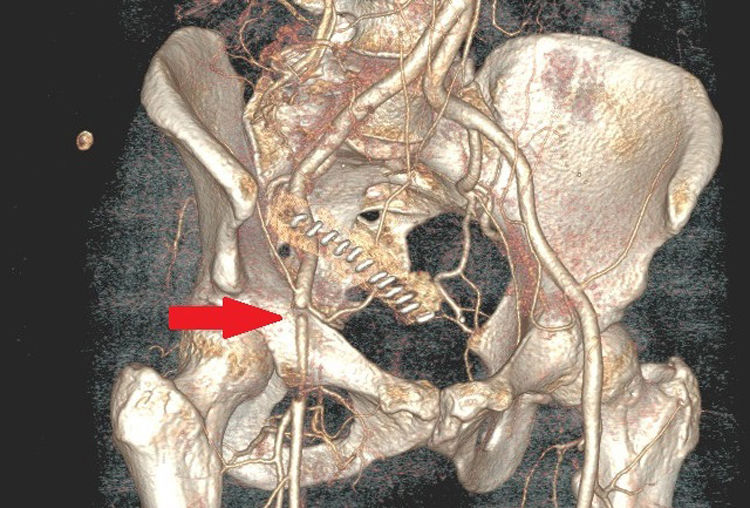
Given the suspicion of acute arterial ischemia, computed tomography angiogram (CT-angiogram) was performed (Figs. 1 and 2), which revealed obstruction of the right common FA with posterior recanalization; the superficial and deep FA were permeable, and another obstruction was found in the third portion of the popliteal artery and the origin of the tibioperoneal trunk.
With the finding of an occlusive thrombus in the lumen of the common FA, urgent surgery was indicated. Upon manual release of the artery, a mechanical obstacle was palpated in the iliofemoral transition that corresponded with the stitch of the hernia repair cone anchored to the adventitia of the vessel.
Transfemoral thromboembolectomy was performed with a 4Fr Fogarty catheter, releasing the point of the stenosis and closing the arteriotomy with interrupted 5/0 polypropylene stitches to recover perfusion of the limb. Closed fasciotomies of the anterior and posterior compartment of the calf were also performed for the anticipated treatment of post-perfusion edema. However, during the postoperative period, the patient presented compartment syndrome, requiring extension of the anterior fasciotomy. She was discharged on the sixth day after the second intervention with ischemic sequela upon dorsiflexion of the foot against gravity (grade 3 MRC). After 6 months of rehabilitation and follow-up, she currently presents no motor limitations (grade 5 MRC).
When performing femoral hernia repair, the sutures are close to the arteriovenous bundle, superficial to the iliac artery and veins. The proximity to these structures implies the possibility of iatrogenic injury. In-depth knowledge of the inguinal anatomy is essential to try to avoid unexpected vascular injuries.
The FA passes through the lateral part of the femoral ring and the FV through the medial part. At the medial level of the ring, the transverse fascia attaches to the femoral adventitia, covering the space between the vessels, and is called the femoral septum. In turn, this is a weak point where hernias can appear.2 Venous injury is much more common than arterial injury due to its more medial position. The artery can be injured when the transverse fascia is included in the stitches used to close the medial aspect of the internal inguinal ring. Care must be taken when setting the needle-penetration depth and assessing the proximity of the external iliac artery (EIA), which can become trapped, causing stenosis, or be injured by direct puncture or avulsion of one of its branches.3
In our case, the suture trapped the adventitial layer on the anterior side of the artery, causing stenosis that led to secondary thrombosis of the common FA and a distal embolism. Postoperative analgesia and the slow progression of functional limitation disguised the symptoms of ischemia, delaying diagnosis for up to 3 days, which initially led to a neurological sequela despite optimal limb revascularization.
Clinical suspicion should guide the correct diagnosis and treatment of these lesions. The loss of pulses or the weakness of the femoral pulse compared to the contralateral limb after inguinal surgery should lead to suspicion of a possible arterial lesion, and symptoms of sudden claudication with coldness and paresthesia are highly suggestive of ischemia.2
Urgent evaluation by a vascular surgeon will avoid potential neuromotor sequelae or even loss of the limb.
In the event of bleeding due to direct injury to the artery, randomly applied hemostatic stitches should be avoided. It is recommended to dissect and correctly expose the artery in order to reliably identify the point of injury and make the repair properly under direct vision, using non-stenosing vascular sutures or patch angioplasty depending on the size of the defect.
Arterial injury after surgery for femoral hernia is a rare but serious complication. It is important to explore the diagnosis of ischemia in patients after recent femoral hernia repair who present absence of pulses in association with coldness, paleness, paresthesia or motor dysfunction of the ipsilateral limb. Proper diagnosis and treatment of a vascular injury minimizes the subsequent consequences of ischemia.1
Please cite this article as: Tellaeche de la Iglesia M, Perfecto Valero A, Rebollo García A, Aranda Escaño E, Apodaka Díez A. Isquemia aguda de extremidad inferior tras lesión arterial secundaria a hernioplastia crural. Cir Esp. 2020. https://doi.org/10.1016/j.ciresp.2020.01.002