The appearance of new barbed sutures is an advance in making knots and anastomosis, mainly in laparoscopic surgery, where the majority of the surgeons find themselves limited dealing with these sutures. Through this review we aim to evaluate both the use and the safety of the sutures in General and Laparoscopic Surgery. Barbed sutures seem to ease the procedures improving key aspects such as reproducibility and operative time.
La aparición de las nuevas suturas barbadas es un avance en la realización de nudos y anastomosis, principalmente en cirugía laparoscópica, donde gran parte de los cirujanos se encuentran limitados en la realización de dichas suturas. Con esta revisión, se pretende valorar el uso que se ha realizado y la seguridad que presentan en cirugía general y digestiva laparoscópica. La sutura barbada parece facilitar la práctica, mejorando claramente aspectos claves en cirugía como son la reproductibilidad y el tiempo operatorio.
From the start of surgery sutures have been secured by tying a knot. In spite of the multitude of materials that have been used, there is no evidence regarding which is the best suture or the best way to secure one. Historically it was assumed that sutures had to be secured by a final knot. The majority of surgeons find it hard to understand a suture without its corresponding knot. Barbed sutures have recently appeared in the market, and make it possible to use a suture without a final knot. This revision aims to analyse the advantages, safety and applications of using barbed sutures. Relevant articles were analysed for this purpose, as obtained by searching the bibliography in the MEDLINE database for ones from 2000 to 2014. The key words used in searching were “barbed suture”, “laparoscopic anastomosis” and “laparoscopic knots”.
In 1956, Alcamo patented the first single direction barbed suture.1 Use of this was first described in 1967 for the repair of hand flexor tendons.2
Suture Property ConceptsMany surgeons may find the idea of using a suture without a final knot to offer dubious safety. Nevertheless, although surgical knots are widely accepted in surgical tradition, they have some disadvantages:
- 1.
Tension. Although at first sight pressure seems to be similar throughout the whole line of suture, it increases in the knot and in the suture that is closest to it. This “tension gradient” could interfere with homogeneous scarring at the edges of the wound.3
- 2.
Slipping. The weakest point of any line of surgical suture is the knot. The second weakest point is the part of the suture immediately next to the knot, with reductions in strength of from 35% to 95%, depending on the state of the material used.3,4 From a biomechanical point of view, these data could explain the effects of slippage of the suture material itself through the knot, and the inevitable elongation suffered at the point of the knot.
- 3.
Human error. To counterbalance this slipping effect knots are sometimes tied “too tightly”, which may cause necrosis or faults in wound scarring.5
- 4.
Foreign body. On the other hand, the knot in itself represents a source of foreign body reactions in any suture. In fact, the inflammatory reaction around the knot has been found to be proportional to the size of the surgical knot.3,5
- 5.
Use in minimally invasive surgery. The arrival of laparoscopic surgery has given rise to a technical challenge, above all in the manoeuvres which require especial skill such as tying surgical knots. Tying knots inside and outside the body requires a large amount of training, and even with this knots tied using laparoscopy have often been found to less secure than those tied by hand.6 In cases where it is difficult to tie a knot, the use of barbed sutures could improve surgical time,7–9 reduce the tiredness of the surgeon and even costs.10
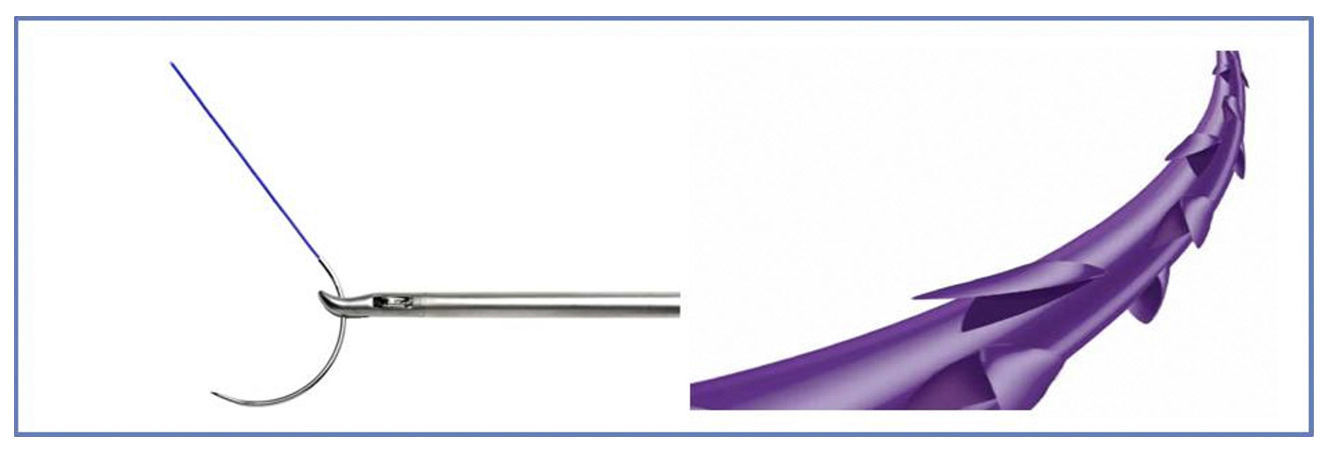
It is not easy for a surgeon, at least at first, to use a suture and not tie it without feeling doubts about its security. The way barbed sutures are made, by making small cuts in the surface of a smooth suture, may clinically give rise to a reduction in its tensile strength as a result of reducing the “functional diameter” of the suture.10 However, existing data indicate that barbed suture has a tensile strength that is comparable to its un-barbed equivalent, as is reported in several in vitro studies11,12 (Fig. 1).
Few experimental studies have been carried out to date, although many of their findings can be extrapolated to our field of action, even though they may not be directly connected with general surgery. The majority of these studies examine the mechanical characteristics of barbed suture in quite a limited number of cases. Studies are required that would evaluate the long-term biological effects of this suture and compare different types of barbed suture, as well as the advisability or not of using other fixing elements at the end of the suture (clips or similar).
In 2011, Vakil et al.12 carried out a study of the closure of an arthrotomy with continuous barbed suture in comparison with single stitches using unbarbed suture. They performed a stress test, exposing the joint studied to 2000 flexions. This left both types of suture intact. Nevertheless, when both sutures were gradually cut, barbed suture resisted longer. The unbarbed sutures gave way after the third cut, while the barbed suture lasted until the seventh cut. The authors therefore conclude that barbed suture is best able to maintain the integrity of suture.
In 2013, Arbaugh et al.13 carried out a series of gastropexies using barbed and unbarbed sutures in dogs, after which they studied the tensile force necessary to cause a suture failure. They found that the force applied to achieve dehiscence was greater for barbed suture, which even led to the tearing of tissue rather than breakage of the suture itself.
In 2012, Gozen et al.7 found that barbed suture was better in terms of the tightness of the suture in a series of pig bladder closures. Following the closure of the defect in the bladder with barbed and unbarbed sutures, they found by using cystometry that the bladder had to be larger in volume for a leak to be created at the closure with barbed suture (419.7ml) than was the case with continuous unbarbed suture (353.08ml) or in single stitches (276.2ml).
In a similar way, Nett et al.14 report greater tightness in the closure of an arthrotomy with barbed suture than is the case with unbarbed suture. They found that following the simulation of a tension hemarthroma, leakage of 89ml occurred from barbed suture while 356ml drained from the unbarbed suture.
Once again in connection with suture tightness, Ehrhart et al.15 studied the pressure at which dehiscence occurs at the suture following the closure of gastric, colic and intestinal defects, without finding any significant differences between single-thread and barbed suture.
Einarsson et al.16 investigate the reaction of tissue to barbed suture at a microscopic level in an ovine experimental model. The procedure consisted of creating 2 defects (bicorn uterus), one of which was then closed using barbed suture while un-barbed suture was used in the other one, so that each sheep functioned as its own control. After 3 months the animals were sacrificed, without any differences being found between the 2 groups in terms of the degree of adherences and arrangement of connective tissue around the scar.
In 2014, Bellon et al.17 published a comparative study in rabbits. They were operated using an average laparotomy of 2cm which was then closed. After 3 weeks the specimens were sacrificed and samples with barbed and un-barbed sutures were studied. No differences were found in the morphological study, collagen expression, macrophage response or the biomechanical study.
The Use of Barbed Sutures in SurgeryBarbed suture has been used in recent years in different specialities. In gynaecology, several papers have been published that advise the use of barbed suture to reduce operative time and even, in some cases, intraoperative bleeding. For myomectomy as well as hysterectomy several authors defend its use because it facilitates surgical technique.10,18–20 In the field of urology, with the exception of one author who published unfavourable results with the use of this suture (a high rate of urethropelvic stenosis in a small series [5/6 patients]),21 the large majority of urologists defend its use as it reduces operation time and increases the safety of anastomosis.22,23
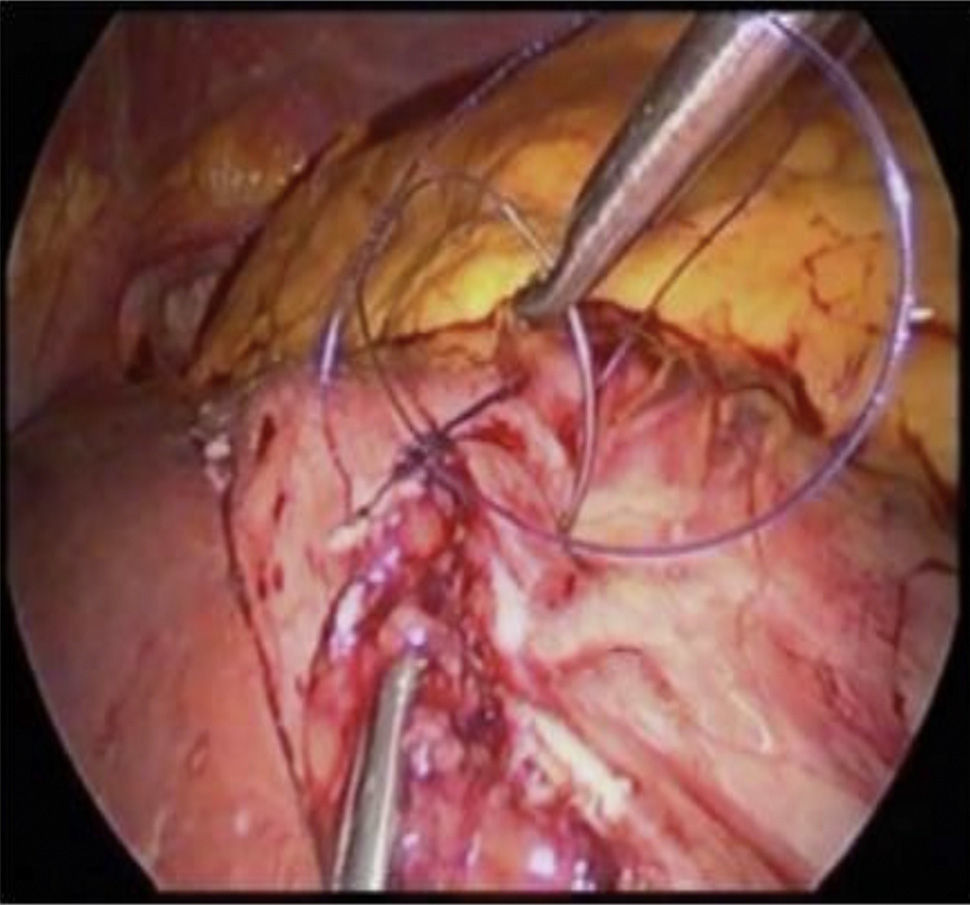
In general surgery, the great majority of publications are about bariatric surgery and its use in laparoscopic gastric bypass. It is well-known that a high level of skill and dexterity is required of surgeons to perform intracorporeal anastomosis (suture and knotting). Therefore, everything that can help anastomosis and make it more reproducible and safer will be appreciated by the great majority of specialists (Fig. 2).
In this way Milone et al.24 included 60 patients in a prospective randomised study in which barbed suture was used in gastrojejunal anastomosis in 30 patients, while in the other 30 Poliglactin 3–0 was used. The main subject of the study was the time taken for the suture and operation, while its secondary subjects were the rate of leakage, bleeding and stenosis. In the barbed suture group significantly less time was required for anastomosis than was the case in the control group (P<.001), while no differences were detected in complications. They conclude by indicating the use of barbed suture for gastrointestinal anastomosis.
De Blasi et al.25 undertook a comparative study of 100 gastric bypass candidate patients. 50 were treated by gastrojejunostomy using single absorbable stitches, while continuous barbed suture was used in the other 50. The anastomosis time was significantly shorter in the barbed suture group (11 vs 8.22min; P>.01), while the cost of the material used to complete reconstruction was lower (26.69€ vs 18.33€; P<.001). No differences were found in postoperative complications. The authors conclude that the use of barbed suture is as safe as the use of conventional sutures, while it permits faster and simpler suturing in gastrojejunal anastomosis, so that it could be included in the standard technique for laparoscopic gastric bypass.
A retrospective study compares standard absorbable single-thread suture with barbed suture for creating gastrojejunal anastomosis, as well as jejunojejunal anastomosis. The new treatment is able to slightly shorten the operation time, without any differences in terms of hospital stay or postoperative complications.26
Palmisano et al.27 publish their experience in creating a gastrojejunostomy and jejunojejunal anastomosis with barbed suture in 2 planes, finishing with placing an absorbable clip at the distal end. Of the total number of 96 patients, 2 had fistulas in the jejunojejunal anastomosis while there were none in the gastrojejunal anastomosis. According to the authors, these data are comparable to those described in the literature, and they suggest that well-designed studies in the future should be undertaken to prove the safety and efficacy of this suture.
As well as bariatric surgery, the use of this suture has other possibilities within the speciality. These have been covered by recent publications. Edil et al.28 used barbed suture in the last 19 patients of a series of 37 in Whipple's procedure for pancreaticojejunostomy. 5% of the patients in the new technique group presented a pancreatic fistula, while the corresponding figure for the standard group was 11%. Additionally, the operation time was shorter for the patients with the new technique (367min) than it was with the standard one (440min). The authors conclude that the use of barbed suture for laparoscopic pancreaticojejunostomy is a safe and effective technique, with similar results to those of other series of laparoscopic Whipple procedures.
Barbed sutures have been safely used in closure of the pelvic cavity following abdominoperineal amputation. Matsuhashi et al.29 present their first results in 2 cases that required laparoscopic Miles with closure inside the pelvic cavity. During follow-up neither of the patients presented complications or signs of relapse. The authors hypothesise that barbed suture may improve the efficacy of closure inside the pelvic cavity following laparoscopic abdominoperineal resection, and they believe it may reduce the stress felt by the laparoscopic surgeon during the operation.
Another use in colorectal surgery is for closure of the rectal wall after transanal endoscopic microsurgery. Wilheim et al.30 compare closure of the horizontal defect in the rectal wall of experimentation animals using single-thread suture with a clip at the end or self-affixing barbed suture. The objective is to measure the pressure at which air leaks through the line of suture as well as the time of leakage. The average pressure for the barbed suture was 45.5mbar, while it was 33.5mbar for the single-thread suture (P=.58). The suture time was the same in both groups. They conclude that the barbed suture permits the same pressure as the single-thread one, and that it seems feasible to use it in the rectal wall.
Several cases have been described in the literature of obstructive symptoms secondary to the use of barbed sutures, possibly due to the contact of the barbed material with intestinal loops and its capacity to hold them, as a result of its characteristics, on the surface.31,32 Surgeons must keep this hypothetic problem in mind, with a high level of suspicion in case of postoperative symptoms of obstruction. It is therefore advisable to avoid contact with the material as far as is possible, and it is recommended that its distal end be cut as close as possible to where it protrudes from the tissue.
ConclusionsIt is possible that the technically most demanding part of laparoscopic surgery in terms of dexterity is anastomosis and suturing inside the body. In spite of the development of laparoscopy and the fact that it is now a standardised technique in many habitual surgical procedures, relatively few diseases require the use of sutures within the body. Barbed sutures may facilitate this practice, avoiding the need to tie knots inside the body as well as the need for the assistant to maintain continuous tension in the suture, clearly improving key aspects of surgery such as reproducibility, operating time and surgeon tiredness. The principles of tension, vascularity and perfect surgical technique must be respected regardless of the material used.
Clinical review of the literature supports its use as a safe and effective technique, one which is at the least equivalent to conventional absorbable sutures. In any case prospective, controlled and randomised studies are necessary to confirm these findings.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ferrer-Márquez M, Belda-Lozano R. Uso de las suturas barbadas en cirugía general y digestiva. Revisión de conjunto. Cir Esp. 2016;94:65–69.