Our aim is to analyze the differences between sporadic gastrointestinal stromal tumors and those associated with other tumors.
MethodsRetrospective cohort study including patients with diagnosis of gastrointestinal stromal tumors operated at our center. Patients were divided into two groups, according to whether or not they had associated other tumors, both synchronously and metachronously. Disease free survival and overall survival were calculated for both groups.
Results96 patients were included, 60 (62.5%) were male, with a median age of 66.8 (35–84). An association with other tumors was found in 33 cases (34.3%); 12 were synchronous (36.3%) and 21 metachronous (63.7%). The presence of mutations in associated tumors was 70% and in non-associated tumors 75%. Associated tumors were classified as low risk tumors based on Fletcher’s stratification scale (p = 0.001) as they usually were smaller in size and had less than ≤5 mitosis per 50 HPF compared to non-associated tumors. When analyzing overall survival, there were statistically significant differences (p = 0,035) between both groups.
ConclusionThe relatively high proportion of gastrointestinal stromal tumors cases with associated tumors suggests the need to carry out a study to rule out presence of a second neoplasm and a long-term follow-up should be carried out in order to diagnose a possible second neoplasm. Gastrointestinal stromal tumors associated with other tumors have usually low risk of recurrence with a good long-term prognosis.
El objetivo de este estudio es analizarsi existen diferencias entre los GIST esporádicos y los que se presentan asociados a otros tumores.
MétodosEstudio de cohorte retrospectivo de pacientes operados de GIST en nuestro centro. Se dividió a los pacientes en función de si presentaban otros tumores asociados o no, de forma sincrónica o metacrónica. La supervivencia libre de enfermedad y la supervivencia global se calcularon en ambos grupos.
ResultadosSe incluyeron un total de 96 pacientes, 60 (62.5%) eran hombres con una media de edad de 66.8 años (35–84). Se encontró una asociación con otros tumores en 33 casos (34.3%); 12 de manera sincrónica (36.3%) y 21 metacrónica (63.7%). La presencia de mutaciones en el grupo de tumores asociados fue del 70% y en el de no asociados del 75%. Los tumores asociados se clasificaron como tumores de bajo riesgo según la escala de Fletcher (p = 0,001), ya que fueron de menor tamaño y presentaron menos de ≤5 mitosis por 50 HPF en comparación con los no asociados. Al analizar la supervivencia global, hubo diferencias estadísticamente significativas entre ambos grupos (p = 0,035).
ConclusiónLa proporción relativamente alta de casos de GIST con tumores asociados sugiere la necesidad de realizar un estudio para descartar la presencia de una segunda neoplasia y, tras el tratamiento de GIST, realizar un seguimiento a largo plazo para diagnosticar una posible segunda neoplasia. Los GIST asociados a otros tumores suelen tener un riesgo bajo de recurrencia con un buen pronóstico a largo plazo.
Since the description of gastrointestinal stromal tumors (GIST) by Mazur and Clark, the number of diagnoses has increased and they are currently the most common mesenchymal tumors of the digestive tract.1 Almost 60% of GISTs are located at the stomach, followed by the small bowel (30%) and less frequently the colon-rectum (5%) and the oesophagus (1–2%).1 95% of GISTs are sporadic, while 5% can be associated with genetic syndromes such as neurofibromatosis, Carney’s triad, or familial GIST.2 In these cases, the association with other tumors, both benign and malignant, is frequent.3
In the case of sporadic GIST, association with other tumors has been described in a variable percentage (4.5–33%), with a preferential location in the gastrointestinal tract followed by the urogenital one and a higher percentage of adenocarcinomas.4–6
The pathogenesis of GISTs is related to the activation of the tyrosinkinase receptors (c-kit) or the platelet-derived growth factor receptor (PDGRF-α) of the interstitial cells of Cajal.7,8 Likewise, the c-kit receptor is involved in the development and maintenance of erythropoietic stem cells, mast cells, melanocytes and germ cells.
In recent decades, there has been an important advance in the knowledge of the characteristics of isolated GISTs, but there are few contributions on GIST’s that occur in association with other tumors, so their clinicopathological characteristics and prognostic factors are poorly clarified. GISTs can co-exist with tumors located in the gastrointestinal tract or elsewhere in the body. This association has not been well described in the literature, either the pathogenesis or the prognosis, with scarce data.
The aim of this work is to present our experience with GISTs associated with other tumors, both synchronous and metachronous, and to compare them with GIST that occur in isolation.
MethodsA retrospective single center study in a highly specialized upper gastrointestinal unit from a tertiary hospital, was carried out in patients operated of GIST, from 2000 to 2020. Data was collected from a prospective institutional clinical database and subsequently analyzed. Institutional board approval was obtained, and patients signed informed consent. Patients with GIST tumors candidates to surgical treatment were consecutively selected. The diagnosis of GIST was established by histological and immunohistochemical study after surgery. We do not systematically perform puncture-biopsy, except in patient’s candidates for neoadjuvant treatment with Imatinib. General indications for neoadjuvant treatment are in patients with large tumors in order to ensure an R0 surgery.9 The standard dose of Imatinib is 400 mg/day.
All patients underwent pre-treatment staging with chest-abdominal-pelvic CT scan and endoscopic ultrasound in cases located in the stomach, esophagus and duodenum less than 3 weeks before first treatment (either surgery or neoadjuvant therapy). Once the tumor was resected, the presence of mutations was analyzed by isolating DNA and amplifying exons 9, 11 of the c-kit gene and exons 12 and 18 of PDGRF-α, according to the method previously described by us.10
For the analysis of tumor size, the patients were grouped into two groups: ≤5 cm in diameter and > 5 cm. Likewise, we made another classification based on the number of mitoses per 50 HPF: ≤ 5 mitoses and > 5 mitoses.
Patients were divided into two groups, according to whether or not they had associated other tumors, both synchronously and metachronously. Thus, two groups were established:
- •
Non-associated tumors: isolated GIST.
- •
Associated tumors: synchronous or metachronous GIST to other tumors.
The outcome variables were disease free survival (DFS) and overall survival (OS) in the isolated GIST and the group of associated tumors. Other variables analyzed were age, sex, symptoms at diagnosis, diagnosis after accidental finding, tumor location and size, number of mitoses per 50 high power fields (HPF), determination of mutations, presence or not of associated tumors and location of the same.
Screening for disease progression was performed every 6 months during the first two years and annually thereafter. Follow-up was performed by clinical control and chest-abdominal-pelvic computed tomography scan at each visit. In cases of gastric location, biennial gastroscopy was added.
A descriptive analysis was performed, and quantitative variables were tested for normality with the Kolmogorv-Smirnov test. Qualitative data were expressed as n (%) and quantitative data as median (range). The chi-squared test was used for categorical variables. Disease-free survival and overall survival were calculated using the Kaplan–Meier curves and log-rank test to assess for differences between groups. p < 0.05 was considered statistically significant. Statistical analysis was carried with the IBM® SPSS® Statistics Version 19® for Windows (SPSS; Chicago, Illinois. USA).
ResultsA final cohort of 96 patients, 60 (62.5%) of whom were male, with a median age of 66.8 (35–84) years was defined for the study. Of the 96 tumors studied, an association with other tumors was found in 33 cases, which constitutes 34.3% of the total. Of these, 12 were synchronous (36.3%) and 21 metachronous (63.7%). The characteristics of these cases are shown in Table 1.
Characteristics of the patients.
| Non-associated GIST | Associated GIST | p Value | |
|---|---|---|---|
| N = 63 | N = 33 | ||
| Gender | |||
| Male | 39 (61.9%) | 21 (63.6%) | n.s. |
| Female | 24 (38.1) | 12 (36.4%) | |
| Location | |||
| Gastric | 37 (58.7% | 20 (60.6%) | n.s. |
| Duodenum | 2 (3.2%) | 2 (6.1%) | |
| Small bowel | 16 (25.4%) | 10 (30.3%) | |
| Colon | 3 (4.8%) | – | |
| Retroperitoneum | 5(7.9%) | 1 (3%) | |
| Size | |||
| ≤5 cm | 23 (36.5%) | 28 (84.8%) | 0.001 |
| >5 cm | 40 (63.5%) | 5 (15.2%) | |
| Mitosis | |||
| ≤5 | 40 (63.5%) | 31 (93.9%) | 0.001 |
| >5 | 23 (36.5%) | 2 (6.1%) | |
| Risk scale (Fletcher) | |||
| Very low | 8 (12.7%) | 12 (36.4%) | 0.001 |
| Low | 14 (22.2%) | 14 (42.4%) | |
| Intermediate | 11 (17.5%) | 4 (12.1%) | |
| High | 28 (44.4%) | 2 (6.1%) | |
| Malignant | 2 (3.2%) | 1 (3%) | |
| Incidental finding | |||
| Yes | 15 (23.8%) | 15 (45.5%) | 0.03 |
| No | 48 (76.1%) | 18 (54.5%) | |
| Mutationa | |||
| Yes | 40/57 (70.2%) | 24/32 (75%) | n.s. |
| c-kit 9 | 1/53 (1.9%) | 1/28 (3.6%) | |
| c-kit 11 | 26/53 (49.1%) | 14/28 (50%) | |
| PDGRF-12 | 7/53 (13.2%) | 2/28 (7.1%) | |
| PDGRF-18 | 2/53 (3.8%) | 3/28 (9.1%) | |
| No | 17/57 (29.8%) | 8/32 (25%) |
n.s. = non significant.
The diagnosis of GIST was incidentally performed during the study of another pathology in 30 cases, 15 (45.4%) of them in the associated group and 15 (23.8%) in the non-associated group (p = 0.038). The locations in which the associated tumors settled are reflected in Table 2.
Location of associated tumors.
| Duodenum (2) | Lung | 1 (50%) |
| Bladder | 1 (50%) | |
| Gastric (20) | Gastric | 5 (25%) |
| Breast | 3 (15%) | |
| Basal cell carcinoma | 2 (10%) | |
| Lung | 2 (10%) | |
| Colon / rectum | 2 (10%) | |
| Bladder | 2 (10%) | |
| Hepatocellular carcinoma | 1 (5%) | |
| Esophagus | 1 (5%) | |
| Leukemia | 1 (5%) | |
| Prostate | 1 (5%) | |
| Retroperitoneum (1) | Gastric | 1 (100%) |
| Small bowel (10) | Basal cell carcinoma | 3 (27%) |
| Breast | 2 (18%) | |
| Hepatocellular carcinoma | 2 (18%) | |
| Colon | 1 (9%) | |
| Vulva | 1 (9%) | |
| Mielodisplasic syndrome | 1 (9%) |
The presence of mutations in associated tumors was 70% and in non-associated tumors, 75%. In both non-associated and associated tumors, the mutation in exon 11 of c-kit was the most frequent (Table 1). There were no differences in the presence of mutations between associated and non-associated tumors. Nor were differences observed when analyzing the distribution of mutations in c-kit located at exon 9 or 11 and PDGRF-α located at exon 12 or 18 between both groups (Table 1).
Tumors with ≤5 mitosis per 50 HPF were more frequently associated with other tumors than those with a mitosis count > 5 (p = 0.07). Likewise, tumors ≤5 cm were more frequently associated with other tumors (p = 0.001) than tumors >5 cm. These facts determine that associated tumors are significantly (p = 0.001) classified as lower risk, based on Fletcher’s stratification scale, compared to non-associated tumors; thus, 78.8% of the associated tumors correspond to tumors with a very low or low risk of recurrence, while in the group of non-associated tumors they constitute only 35% of the sample.
Median follow-up was 76 months in associated cases and 72.9 months in non-associated cases. The median presentation of recurrence was 75.8 and 66.4 months, respectively. Among the associated there was 1 recurrence during the period of study, while in the non-associated group there were 12 recurrences. DFS and OS Kaplan–Meier curves are presented in Fig. 1, appreciating statistically significant differences in both variables.
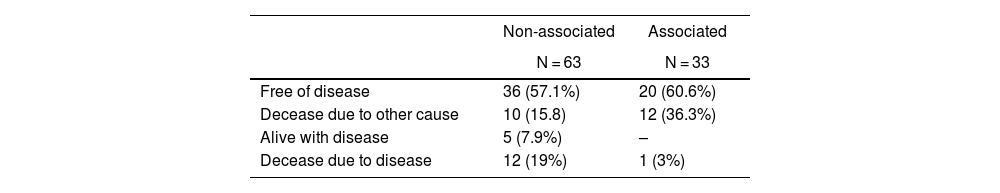
When analyzing OS, we appreciate that in the group of associated tumors there was one death secondary to GIST, while in the non-associated group there were 12 deaths due to it, with statistically significant differences (Fig. 2). The final status of the patients is described in Table 3.
GISTs occur sporadically in 95% of cases and in these cases they can be associated with other tumors, either synchronously or metachronously, in a percentage that varies from 4 to 33%, depending on the series consulted.4–6 In our case, associated tumors account for 34.3% of the series, from which 36.3% of the cases were synchronous and 63.7% metachronous. In the literature, data vary from 78% of synchronic tumors reported by Vassos et al.11 to 16% reported by Du et al.12
There are many factors that can contribute to the development of cancer; the exact mechanism has not been yet clarified. Some of those can be age, exposure to toxics, genetic mutations in oncogenes, lifestyle habits (alcohol, drugs, sedentary lifestyle) or hereditary syndromes, among others. Although there is no definitive explanation that explains the coexistence of GISTs and other tumors, some authors have developed various hypotheses to justify it. Miettinen et al. in 2008 described a “nonrandom” association between GIST and myeloid leukemia.26 Stimulation of the "c-kit signaling pathway" as a result of the c-kit or PDGFR-α mutation is the initial event in the pathogenesis of GIST, and the same mutation has been implicated in the development of acute leukemia. The activation of c-kit has been described in a series of neoplasms such as leukemias, mastocytosis, germ cell tumors and GIST.27,28
Sista et al.29 in 2013 suggested that in gastrectomized patients there is an overexcitation of Cajal cells, which could explain the association between GIST and adenocarcinoma of the gastric stump.28 Various authors have shown that there are some carcinogens that can stimulate the development of neoplasms of both epithelial and stromal cells.30–32 The same carcinogen can act in two neighboring tissues simultaneously and condition the development of two different neoplasms in the same organ.33 Although genetic mutations are decisive in the pathogenesis of tumors, there is no evidence that confirm a common mutation in GISTs and other associated tumors. It has been hypothesized that a single carcinogen can influence two different cell lines of the same organ, causing two different tumors.34 As an example, H. Pylori may be related to the genesis of gastric adenocarcinoma and MALT lymphoma.35 Of the mutations described in GISTs, the most frequent occurs in exon 11 and involves c-kit regulation in up to 75–80% of cases.10,24 This fact is confirmed in our series, which shows that 50% of mutations are located in exon 11 in both associated and isolated tumors; fact that is also appreciated by other authors.3,25
Associated GISTs are more often smaller in size than non-associated.13,14 This fact is fulfilled in our work since 85% of GISTs with associated tumors are ≤5 cm. Microscopic GISTs, which are located preferentially at the proximal gastric portion, those diagnosed incidentally in cases of gastric cancer and in patients operated of morbid obesity are frequently described.15 GISTs as an incidental finding have been described in up to 0.2% of all autopsies,16 the incidence of GIST’s incidentally diagnosed is significantly higher in our series in the group of associated tumors. We also observed a higher percentage of cases with <50 mitosis per HPF in the associated group (93.9% vs 36.5%; p = 0.001), a fact that does not agree with the previous data reported by Hechtmann et al. who reported that a higher mitotic index is significantly related to the presence of a second neoplasm.17 This fact together with the predominance of smaller tumors, suggests that the risk of recurrence in associated tumors according to the Fletcher risk classification is predominantly low or very low.18 Therefore, the prognosis in cases of association with other tumors seems to be conditioned by the associated tumor, rather than the GIST itself.19,20
When analyzing both DFS and OS, we observed significant differences with lower recurrence rates and GIST-specific mortality in the cohort of associated tumors. This difference can be explained by the higher proportion of cases with a low or very low risk of recurrence in the group of associated tumors. These facts are similar to those reported by various authors,11,19,21 who propose that the prognosis in cases of association is marked by the associated tumor rather than by the GIST. However, Kramer described that the presence of an associated tumor has a significant negative impact on overall survival.22 Likewise, Smith et al. performed an analysis of the factors associated with the survival of GIST; among the factors that could influence the presence of an additional malignancy six months after the diagnosis of GIST appeared as a negative factor.23 Typically, the detection rate of a second neoplasm in the preoperative studies is low. In our study, we could reach the diagnosis of an associated neoplasm in only 15 patients (45.4%). These facts confirm the need to implant units that are specifically trained in this type of pathology so this detection rate can improve. Some of the reasons that can explain the low detection rate are the small size of the associated GISTs, the fact that they are submucosal tumors and that sometimes they can be misdiagnosed as lymph node metastases.19
There are several limitations to this study. It is a retrospective, single-centre study that required a wide time span in order to recruit a large enough cohort of patients. Moreover, the mutational status of 7 cases and the type of mutation of 15 patients was missing. The strengths of this study are that all data were collected prospectively and surgeries were performed by a highly specialized group in upper gastrointestinal malignancies. Besides, this paper is one of the largest series of associated tumors to GIST that has been reported.
The association of GIST and other tumors is common. However, it should be noted that GIST tumors associated with others usually have good long-term prognosis as they are smaller in size and classified as very low or low risk according to Fletcher classification scale, compared with isolated GISTs. Due to this association, it is necessary to perform secondary tests for its possible detection and to carry out a long-term follow-up.
Author contributionsConceptualization: Roberto Martí Obiol, Mari Carmen Fernández Moreno, Fernando López Mozos.
Data Curation and Formal Analysis: Roberto Martí Obiol, Rosa Martí Fernández, Fernando López Mozos.
Investigation and methodology: Rosa Martí Fernández, Maria Eugenia Barrios Carvajal
Project Administration and software: Roberto Martí Obiol, Rosa Martí Fernández
Supervision: Mari Carmen Fernández Moreno, Maria Eugenia Barrios Carvajal
Validation: Maria Eugenia Barrios Carvajal, Fernando López Mozos.
Visualization: Mari Carmen Fernández Moreno, Fernando López Mozos.
Writing – original draft: all authors.
Writing – review & editing: all authors.
Ethics approvalInstitutional board and ethics approval were obtained for this work (institutional code: (2021/149)).
FundingThis research has not received specific support from public sector agencies, the commercial sector or non-profit entities.
Conflicts of interestThe authors declare they do not have any conflicts of interest.