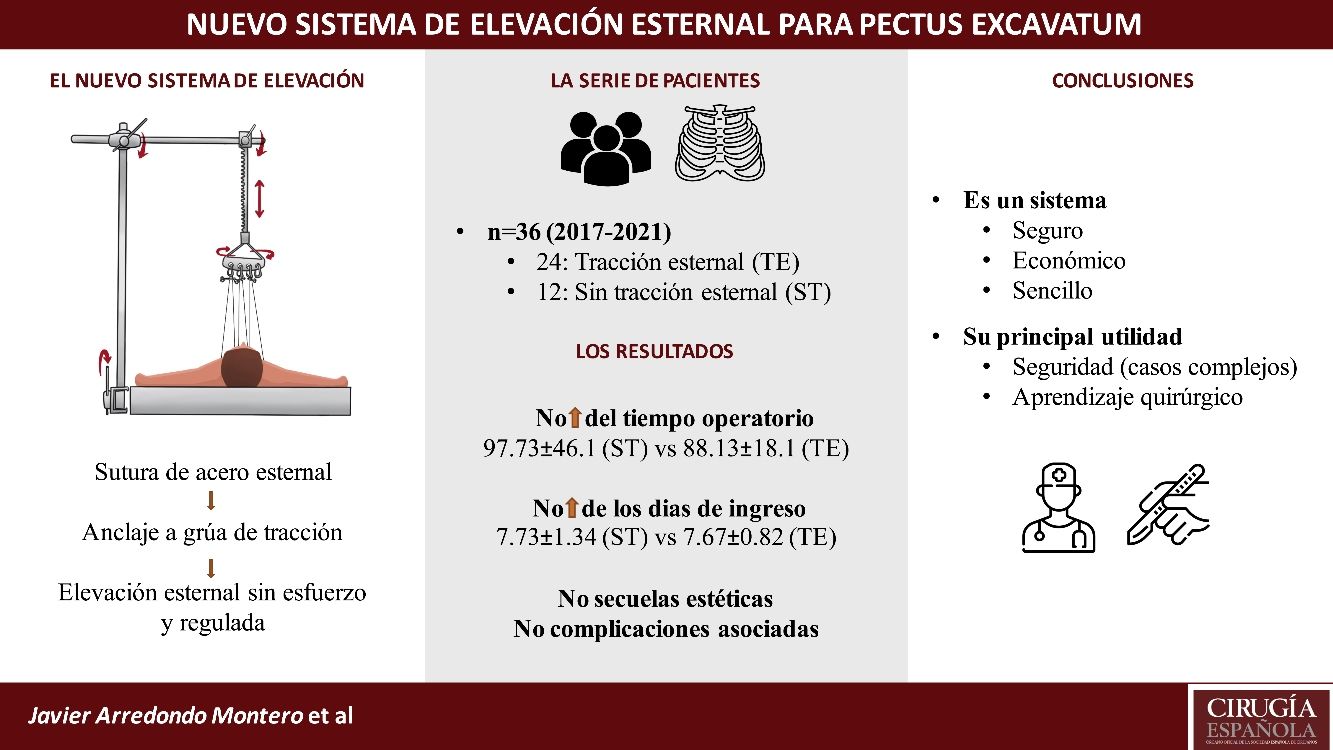
Video-assisted percutaneous thoracoplasty involves a complex surgical access with risk of damaging vital structures during the procedure. Historically, different traction and sternal elevation systems have been applied during the intervention to minimize the risk associated with the passage of the instruments between the sternum and the pericardium.
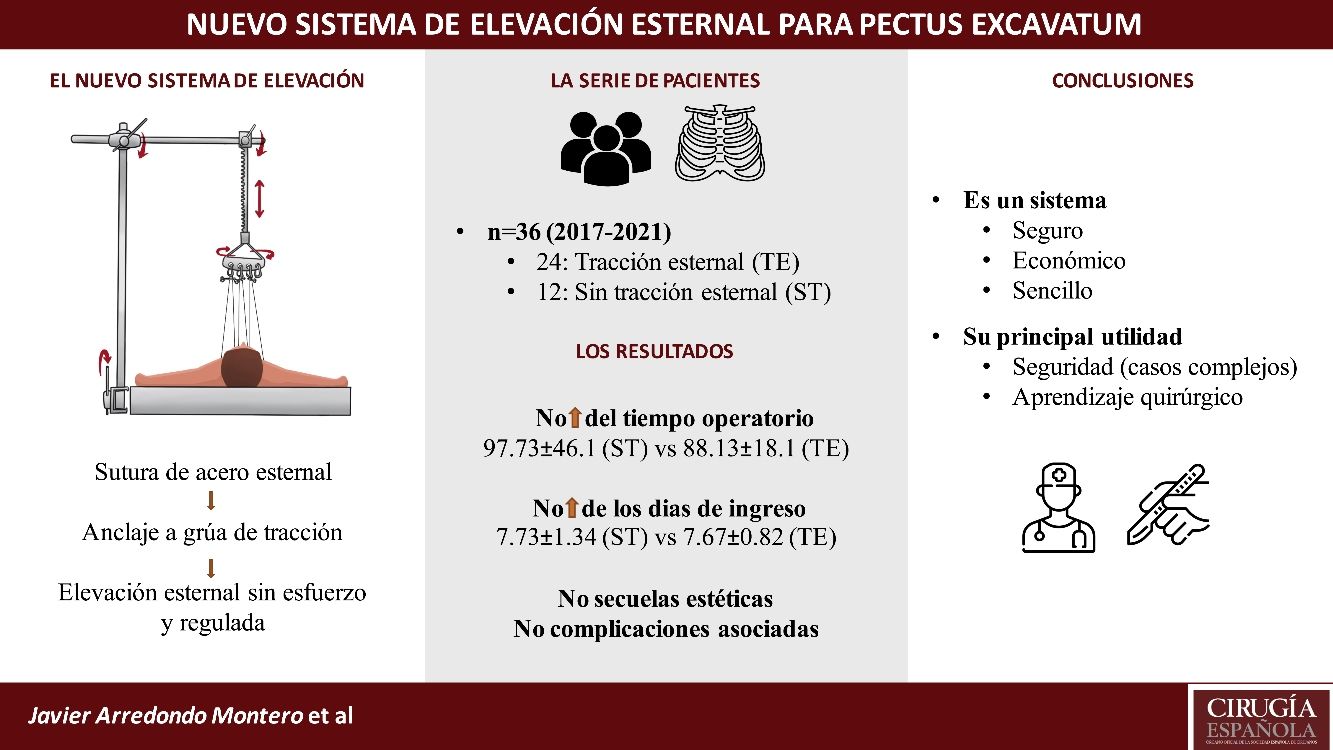
Material and methodsA new sternal traction system is presented by means of an illustrated description. Clinical and sociodemographic data were extracted from the 36 patients operated in our center for Pectus Excavatum between July 2017 and August 2021. The Haller index was not applied as a criterion to determine the use or not of the sternal traction system. Patients were classified according to whether the sternal traction system (TE) or not (ST) had been employed. Statistical analysis of the data collected was performed with STATA, version 15.0 (StataCorp).
ResultsBoth groups were comparable. Haller's Index was 4.19 ± 0.7 for the sternal traction (TE) group and 3.79 ± 0.3 for the no sternal traction (ST) group. In 25 of the patients the described traction system was used, and in 11 no traction system was used. All patients were operated on by the same surgeon. The mean operative time in minutes was 97.73 ± 46.2 for the ST group and 88.13 ± 18.1 for the TE group (p = 0.87). The mean total days of admission was 7.67 ± 0.82 (TE) and 7.73 ± 1.35 (ST). Mean days of intravenous PCA was 6.08 ± 0.72 (TE) and 5.89 ± 1.45 (ST). The mean number of epidural PCA days was 3.79 ± 0.5 (TE) and 3.36 ± 0.5 (ST) (p = 0.01). All patients presented a favorable postoperative evolution. None of the patients presented discomfort at the level of the sternal wounds during hospitalization. Cosmetic evolution was favorable in all patients.
ConclusionsThe sternal traction system presented provides safety when performing retrosternal dissection and placement of the thoracoplasty bar, leading to a decrease in surgical time in cases with a Haller Index higher than 3.5. There have been no complications associated with its use, nor has there been an increase in the number of days of hospitalization or analgesic requirements. There are no aesthetic sequelae for the patients.
La toracoplastia percutánea videoasistida implica un acceso quirúrgico complejo y con riesgo de dañar estructuras vitales durante el procedimiento. Históricamente se han aplicado distintos sistemas de tracción y elevación esternal durante la intervención con el fin de minimizar el riesgo asociado al paso del instrumental entre el esternón y el pericardio.
Material y métodosSe presenta mediante una descripción ilustrada un nuevo sistema de tracción esternal. Se extrajeron los datos clínicos y sociodemográficos de los 36 pacientes intervenidos en nuestro centro de Pectus Excavatum entre julio de 2017 y agosto de 2021. Todos los pacientes fueron intervenidos por el mismo cirujano. Se clasificó a los pacientes en función de si se había empleado el sistema de tracción esternal (TE) o no (ST). La asignación a uno u otro grupo de intervención se hizo siguiendo un criterio cronológico, sin aplicar el índice de Haller u otro índice. El análisis estadístico de los datos recogidos se realizó con STATA, versión 15.0 (StataCorp).
ResultadosLa distribución de las variables sociodemográficas muestra que no había diferencias significativas entre los grupos. En 25 de los pacientes se empleó el sistema de tracción esternal (TE), y en 11 no se empleó ningún sistema de tracción (ST). El Índice de Haller fue de 4.19 ± 0.7 para el grupo TE y de 3.79 ± 0.3 para el ST. El tiempo quirúrgico medio en minutos fue 88.13 ± 18.1 para el grupo TE y 97.73 ± 46.2 para el grupo ST (p = 0.87). La media de días de ingreso fue 7.67 ± 0.8 y7.73 ± 1.3 para el grupo TE y ST respectivamente. La media de días de PCA endovenosa fue 6.08 ± 0.7 para el grupo TE y 5.89 ± 1.5 para el ST. La media de días de PCA epidural fue 3.79 ± 0.5 y de 3.36 ± 0.5 para el grupo TE y ST respectivamente (p = 0.01). Todos los pacientes presentaron una evolución postoperatoria favorable. Ninguno de los pacientes presentó molestias a nivel de las heridas esternales durante el ingreso en hospitalización. La evolución cosmética fue favorable en todos los pacientes
ConclusionesEl sistema de tracción esternal que se presenta proporciona seguridad a la hora de realizar la disección retroesternal y la colocación de la barra de toracoplastia, conllevando una disminución del tiempo quirúrgico en los casos con un Haller Index superior a 3.5. No se ha producido ninguna complicación asociada a su uso ni ha supuesto un aumento de los días de ingreso ni de los requerimientos analgésicos. No conlleva secuelas estéticas para los pacientes.
Video-assisted percutaneous thoracoplasty involves a complex surgical approach that involves a complex surgical approach that has an associated risk of damaging vital structures during the procedure. This, added to the limited number of patients with surgical indication and the long learning curve of the technique, contextualize and justify the need for sternal traction systems to be used during surgery.
Historically, different sternal traction and elevation systems have been applied during the procedure in order to minimize the risk associated with the passage of instruments between the sternum and the pericardium.1–8
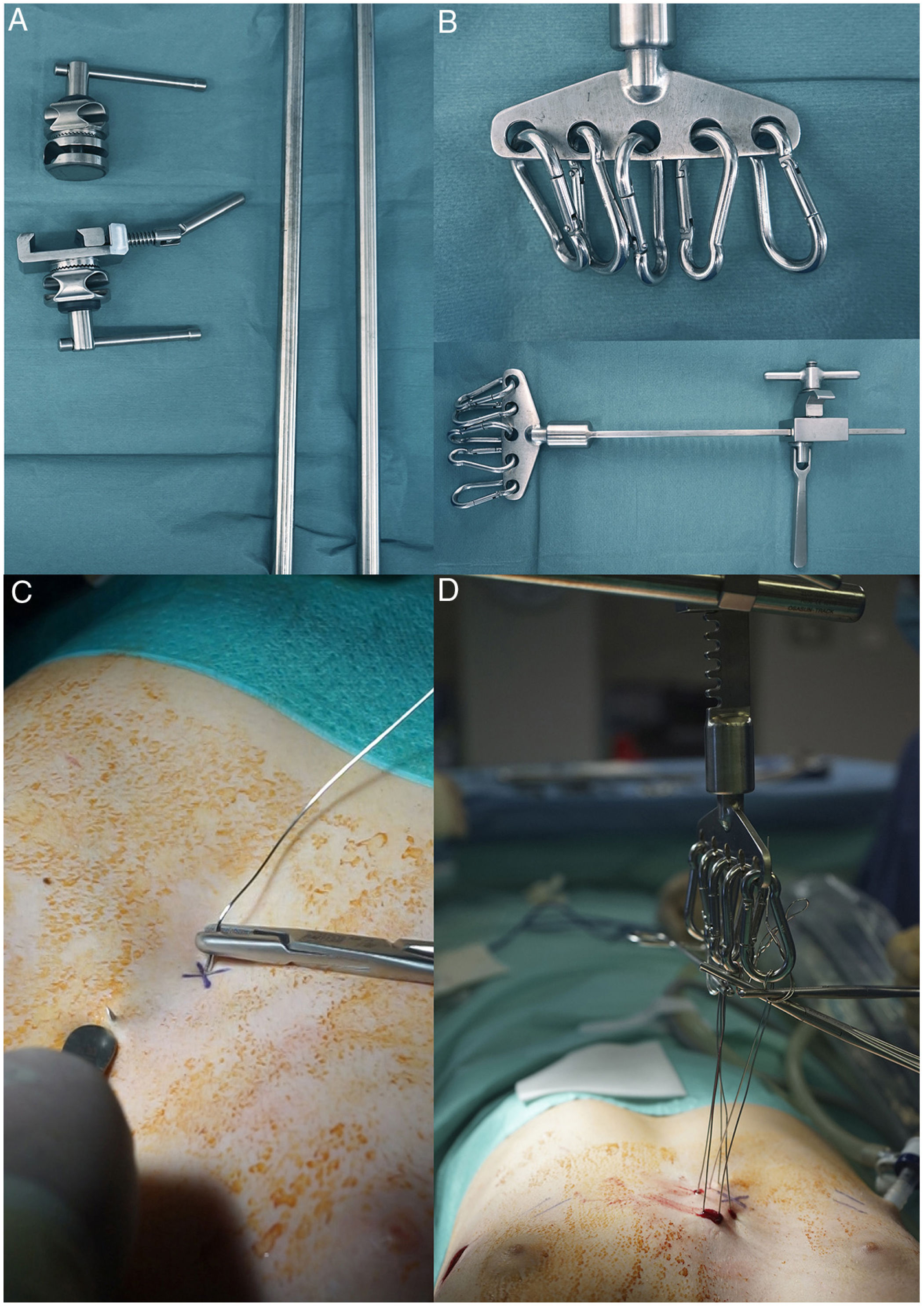
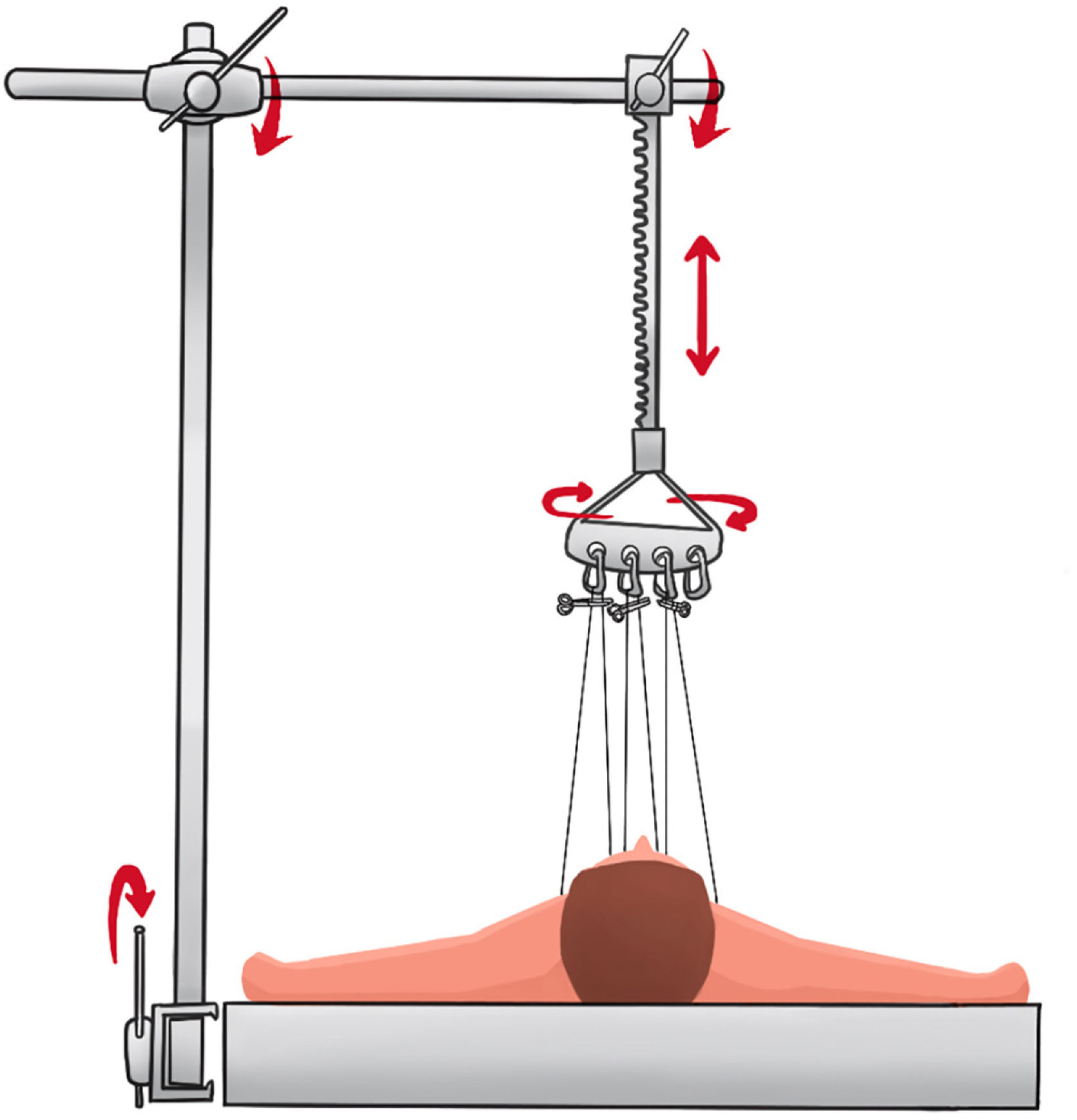
MethodsWe present a traction system that consists of a steel bar that is fixed perpendicularly to the surgical table at the level of the patient’s left axilla. In turn, this is fixed to a second bar with similar characteristics, horizontal to the patient, at an adjustable height, which can rotate 360° to place the traction point at the area of maximum sternal collapse. The traction system includes a lifting mechanism and a rotating head to which the different traction systems can be anchored. During the intervention, transsternal steel sutures are applied longitudinally and in varying numbers depending on the severity of the case and the age of the patient. These sutures pass through the external sternal cortex on entry and exit, without passing through the internal cortex. The surgeon can use a blunt instrument, such as the back of forceps, to control the exit of the needle after applying them (Fig. 1). These sutures are then attached to the carabiners using surgical instruments (Appendix B, Supplement 1). Subsequently, the sternum is elevated at the surgeon’s request using the unidirectional toothed gear system. The procedure is performed without physical effort, and an instantaneous and significant increase is observed in the retrosternal space (Figs. 1–3) (Appendix B, Supplement 2). This allows for easier and safer passage of the dissector through the retrosternal space (Appendix B, Supplement 3).
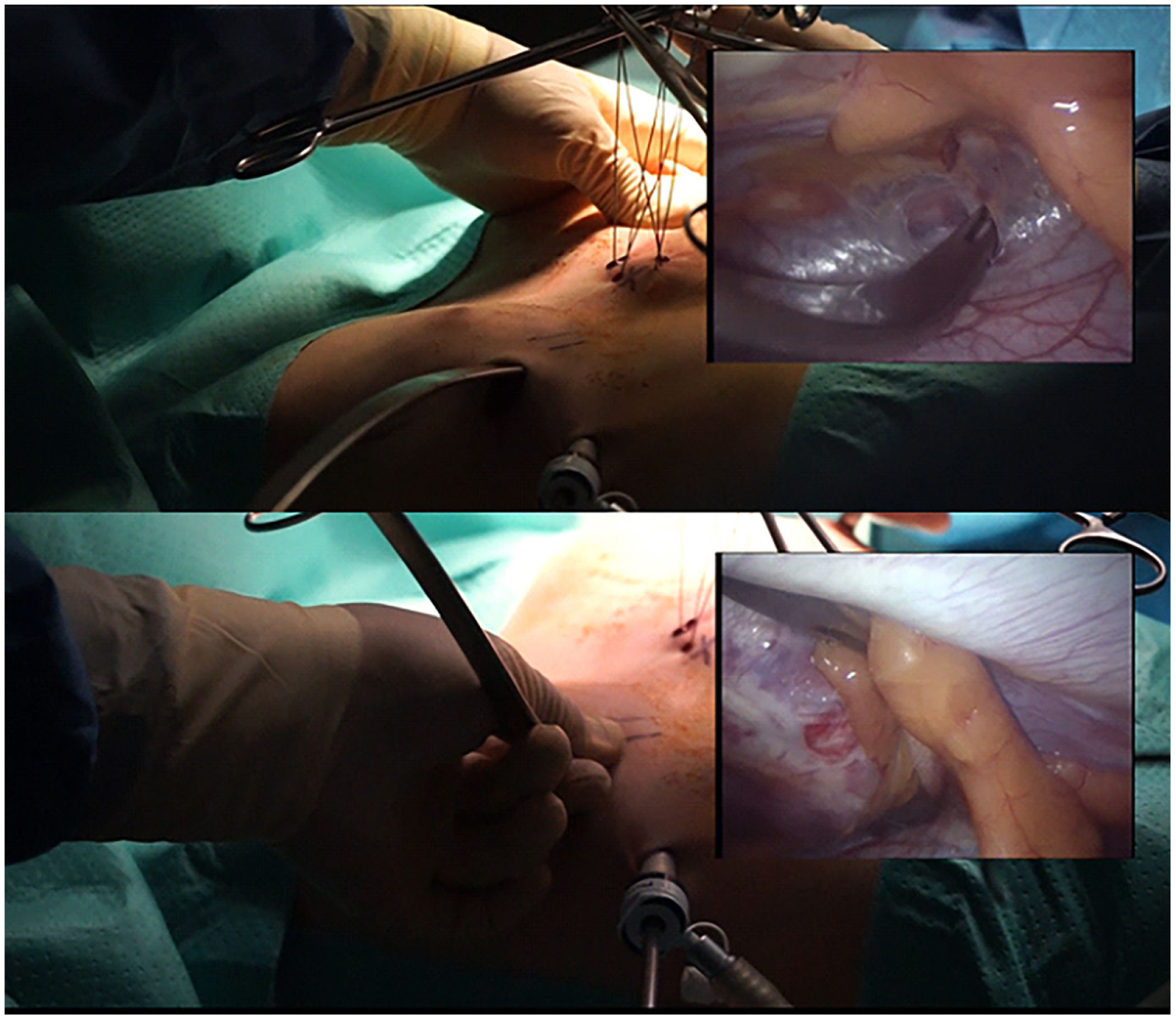
Thoracoscopic view of the traction system. Above: traction system in operation. An increase in the space between the sternum and the pericardium can be seen in the thoracoscopic image (inset on the right), which facilitates dissection and allows it to be carried out with greater safety. Bottom: passage of the tape used as a guide, prior to the passage of the definitive bar. Similarly, this maneuver can be performed more safely and quickly when sternal traction is applied.
Clinical and sociodemographic data were collected from 36 patients who underwent surgery for Pectus Excavatum at our hospital between July 2017 and August 2021 using the video-assisted percutaneous thoracoplasty technique, either with sternal traction (ST) or without sternal traction (no-ST). Patients were assigned to one group or the other according to the date of surgery: from July 2017 to June 2018, patients were treated with the no-ST system; from June 2018 to August 2021, we used the ST system presented herein. The Haller index was not used to determine the use of the system. All patients were operated on by the same surgeon and under similar conditions.
We followed standard methodological and ethical principles for scientific publication. Photographs, clinical data, sociodemographic information and radiological images were collected from the patients’ medical records, and the information was anonymized in accordance with current legislation.
The statistical analysis of the collected data was performed with STATA, version 15.0 (StataCorp). For descriptive purposes, the mean and standard deviation were used for the quantitative variables and percentages for the categorical variables. Sociodemographic and clinical variables were compared between patients operated on with an ST system and those operated on without sternal traction (no-ST). Fisher’s exact test was used to compare categorical variables and the Mann Whitney U test for quantitative variables. Statistical significance was defined as P < .05 (2-tailed). Additionally, the patients were classified into 2 groups based on the Haller index (cut-off point 3.5). Mean surgical time, days of hospitalization, days of ICU stay, and days of intravenous patient-controlled anesthesia (PCA) and epidural PCA were compared in both groups.
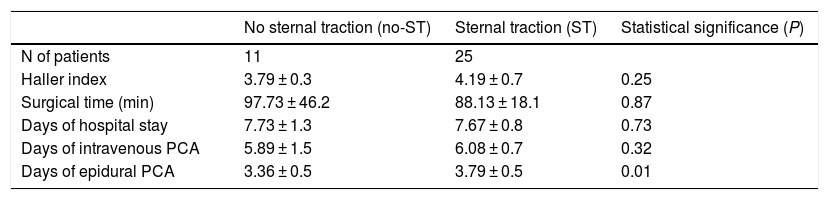
ResultsThe sample consisted of 36 patients, 25 men (69.4%) and 11 women (30.6%), with a mean age of 13.61 ± 4.48 years. In 25 of the patients, the new ST system was used, and in the remaining 11 no sternal traction system (no-ST) was used. Haller’s Index was 4.19±0.7 for the sternal traction (ST) group and 3.79±0.3 for the no sternal traction (no-ST) group (P=.25). The mean surgical time was 88.13 ± 18.1 min for the ST group and 97.73 ± 46.2 min for the no-ST group (P = .87). The mean days of admission were 7.67 ± 0.8 and 7.73 ± 1.3 for the ST and no-ST groups, respectively (P = .73). The mean number of days of intravenous PCA was 6.08 ± 0.7 for the ST group, and 5.89 ± 1.5 for the no-ST group (P = .32); mean days of epidural PCA were 3.79 ± 0.5 (ST) and 3.36 ± 0.5 (no-ST), respectively (P = .01) (Table 1).
Clinical and surgical characteristics of the patients.
| No sternal traction (no-ST) | Sternal traction (ST) | Statistical significance (P) | |
|---|---|---|---|
| N of patients | 11 | 25 | |
| Haller index | 3.79 ± 0.3 | 4.19 ± 0.7 | 0.25 |
| Surgical time (min) | 97.73 ± 46.2 | 88.13 ± 18.1 | 0.87 |
| Days of hospital stay | 7.73 ± 1.3 | 7.67 ± 0.8 | 0.73 |
| Days of intravenous PCA | 5.89 ± 1.5 | 6.08 ± 0.7 | 0.32 |
| Days of epidural PCA | 3.36 ± 0.5 | 3.79 ± 0.5 | 0.01 |
In the 31 patients who presented a Haller index greater than 3.5, the mean surgical time was significantly shorter than in those with a Haller index less than 3.5 (86.61 vs 140.63 min) (P = .004). The traction system was used in 71% of patients with a Haller index greater than 3.5. No significant differences were found in the remaining variables analyzed between the groups created based on the Haller index.
All patients had a favorable postoperative course. None of the patients presented discomfort of the sternal wounds during hospitalization. The cosmetic evolution of the sternal wounds was satisfactory in all patients.
DiscussionIn this study, we present the results of 36 patients treated surgically at our hospital between July 2017 and August 2021 for Pectus Excavatum, 25 of whom were treated with the new ST system, while 11 were not. No significant differences were found between groups for the Haller index, surgical time, days of hospital stay, or days of intravenous PCA. However, the days of epidural PCA were significantly fewer in the group treated with the new ST system.
As for the shorter surgical time in patients operated on with a Haller index >3.5, we attribute this fundamentally to the manner in which sternal elevation facilitates retrosternal dissection and the passage of the bar, as well as to the progressive experience of the surgical team. As a limitation to consider, in the group of patients operated on with a Haller index >3.5, the use of the traction system accounted for 71% of the group, not the total.
Video-assisted percutaneous thoracoplasty, developed by Donald Nuss in 1997,9 was a true revolution in the surgical management of Pectus Excavatum. However, the advantages of minimally invasive thoracic surgery find their counterpart in the greater technical difficulty of the approaches and procedures and in the existence of a more complex and longer learning curve than in the case of open surgery. Likewise, this development is often limited by the small existing volume of pediatric thoracic pathology and by the tendency to centralize treatment at specific hospitals authorized for this purpose.
Given this scenario, it is legitimate to consider whether we can develop technical or surgical resources that facilitate procedures and approaches that enable us to perform the technique under conditions of greater safety for the patient.10 Given the anatomical and surgical implications of video-assisted percutaneous thoracoplasty, a general safety framework is required for its performance. This system is a useful resource for highly complex cases and for the progressive training of new generations of surgeons involved in the procedure.
We believe that the main strength of this paper lies in a large sample size. The application of the technique in our cohort has confirmed its safety and its viability in clinical practice. The main limitation of this study is the lack of randomization to the type of intervention. However, no significant differences were found between the two groups in terms of either sociodemographic or clinical variables, such as the Haller index. On the other hand, the learning curve of the surgeon and the participation of resident interns must be taken into account, which may have influenced the surgical time, as previous studies have also suggested.11
ConclusionsThe sternal traction system we have presented provides safety when performing retrosternal dissection and placement of the thoracoplasty bar, leading to a reduction in surgical time in cases with a Haller index >3.5. There have been no complications associated with its use, nor has it led to an increase in hospital days or analgesia requirements, and there has been no higher prevalence of aesthetic sequelae for patients. Because it is a simple, safe, and inexpensive method, we believe that it should be considered a technical resource for video-assisted percutaneous thoracoplasty in Pectus Excavatum surgery.
Conflict of interestsThe authors have no conflicts of interest to declare.