The duodenal diverticulum is a relatively frequent entity (5%–22%)1 whose diagnosis has been increased over time with the development of new diagnostic and exploratory techniques.
Nearly 200 cases of duodenal diverticular perforation have been reported in literature2 and several treatment options have also been described based on the presentation and the clinical context of the patient.3
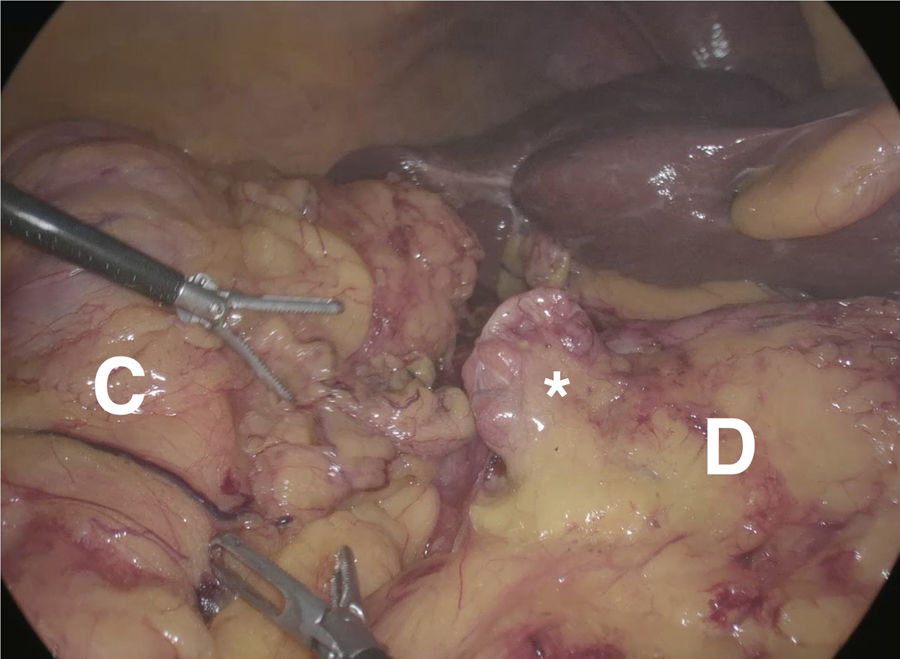
We describe the case of an 80-year-old male, a cardiopath, who underwent a laparoscopic right colectomy for colic cancer. During the surgery, a 2×2cm diverticulum was identified on the anterior face of the second portion of duodenum. It had a good looking, then its manipulation was avoided and finally respected without incident (Fig. 1).
During immediate postoperative the patient restarted oral diet on the first postoperative day (POD). On the fourth POD he presented a sudden desaturation at 88% despite the extra oxygen, confusion and abdominal distension. The blood count showed no leukocytosis but a significant increase of PCR. A thoraco-abdominal CT ruled out pulmonary embolism and it showed pneumo-peritoneum and suspected perforation of the second duodenal portion.
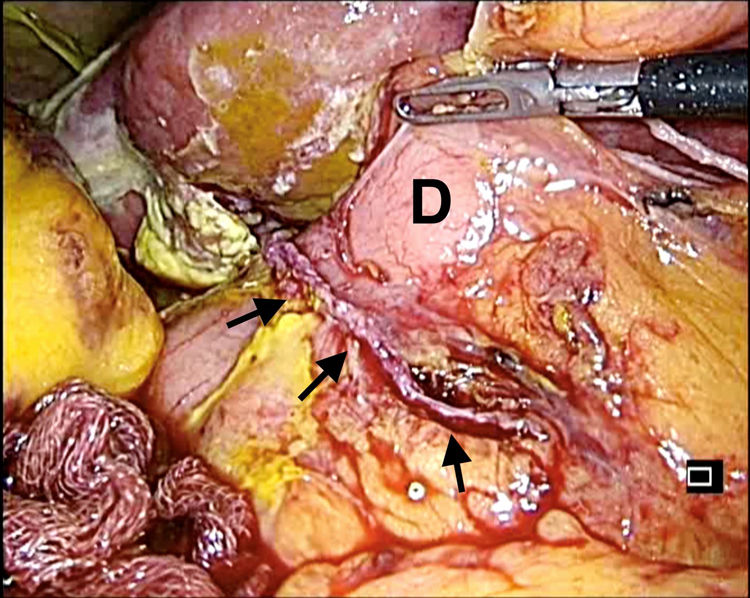
We have performed a laparoscopic exploration after starting empirical antibiotic therapy with Piperacillin-Tazobactam. During surgery, biliary peritonitis was observed close to duodenum with a small bowel plastron. The perforation site was identified corresponding to the free end of the duodenal diverticulum, the integrity of its base had been checked. Resection of the diverticulum was performed by cutting it parallel through the base with an endostapler and the absence of leaks was verified in a 4.5cm stapler line by placing methylene blue (Fig. 2).
During postoperative the patient restarted oral diet on the second POD with good tolerance and he evolved correctly until his discharge.
Duodenal localization of diverticulum is not rare, it's the second most frequent site of presentation after the colon.4 Most of them are accidentally5 and only about 5% become symptomatic or complicated.1 These complications have been described as bleeding, biliary obstruction and perforation. The last one being the most rare and severe. Surgical treatment will be needed in 1–2% of patients diagnosed with a duodenal diverticulum.5
Pre-operative diagnosis is difficult and the intraoperative diagnosis also requires a high preoperative suspicion.5 Ting-Chia et al. reported 16% of mortality related to perforated duodenal diverticulum in 186 cases between 1907 and 2016. Noting a remarkable decrease until 6% from 1989, which is partially explained by the improvement in diagnostic techniques and the development of broad-spectrum antibiotics.2
In case of perforation of a duodenal diverticulum, the treatment of choice is the resection of the diverticulum. Duodenostomy and other surgical options are also available, such as a local Whipple-type excision depending on the size and the degree of the infection.6–10 Laparoscopy has also been described as part of a minimally invasive approach achieving good results with early recovery.7
Ting-Chia et al. made a Medline search about the laparoscopic approach to a complicated duodenal diverticulum between 1994 and 2016, finding 15 cases described, where diverticulectomy was performed in 80% of patients, Distal gastrectomy and gastrojejunostomy in 13% and diverticular inversion in 7%. Mortality was 0%, lower hospital stay and better post-operative recovery was reported.2
Within the treatment options there are series in which the choice of a non-surgical conservative treatment is reported in approximately 2% of patients.5 Chad et al. suggests conservative treatment as a safe treatment alternative in selected patients. In series between 1989 and 2016, up to 22% of patients were described having a conservative management. Concluding that this treatment, based on restriction of intake and broad spectrum antibiotic-therapy, can be a valid option when applied in patients clinically stables with no evidence of sepsis and/or elderly patients with comorbidities and high surgical risk.8
In our case, a laparoscopic approach was performed. No technical difficulty was found thanks to the anterior localization of the diverticulum on second duodenal portion already found in the dissection during the previous oncological surgery. The minimally invasive treatment mini-invasive treatment results in an advantage in postoperative outcomes considering the patient's age and comorbidities.
Haboubi et al. from UK reported a case of perforation of duodenal diverticulum detected at 2nd POD of an elective left colectomy for diverticular disease. The perforation was surgically repaired on the second POD by laparotomy with diverticulectomy. An entero-cutaneous fistula occurred and resolved spontaneously at 2 weeks.9
Despite what is published in literature on duodenal diverticula, the debate on what to do about an incidental finding of duodenal diverticulum during any kind of surgery is still open. Perhaps the best option is not to treat it with an approach “wait and see”. All the published cases correspond to complications of duodenal diverticulum, it is not reported how many of them are found incidentally and ignored without any further clinical relevance.
Duodenal diverticular perforation is a rare entity that poses a diagnostic challenge due to the lack of specific clinical signs and symptoms. The treatment may vary between conservative management and surgical treatment. About surgery the minimally invasive approach provides an advantage in terms of postoperative recovery and hospital stay.
We appreciate the help of the General Surgery Medical Service and Visceral of the Luxembourg Hospital as well as the great work performed by the nursing team.
Please cite this article as: Sánchez-Haro E, Pascotto B, Makkai-Popa ST, Azagra Soria JS. Divertículo duodenal perforado; complicación rara de la colectomía derecha laparoscópica. Puesta al día. Cir Esp. 2021;99:234–236.