Gastroesophageal reflux disease (GERD) is a frequent esophageal disease, with an annual incidence of 0.5% and a prevalence of 10%–20% in developed countries.1 GERD is initially treated with antisecretory drugs, but it has been established that 17%–32% of patients have continued GERD symptoms despite medical treatment.2 The surgical treatment of choice for GERD is fundoplication.3
Obesity and GERD are associated and, therefore, bariatric surgery should be considered in obese patients with refractory GERD.4 According to the criteria of the American Society of Bariatric and Metabolic Surgery (ASMBS), patients with a body mass index (BMI) greater than 30kg/m2 who present a hiatal hernia are also candidates to undergo a bariatric procedure.5 The Roux-en-Y gastric bypass is considered the best option to control GERD-related symptoms in obese patients.6
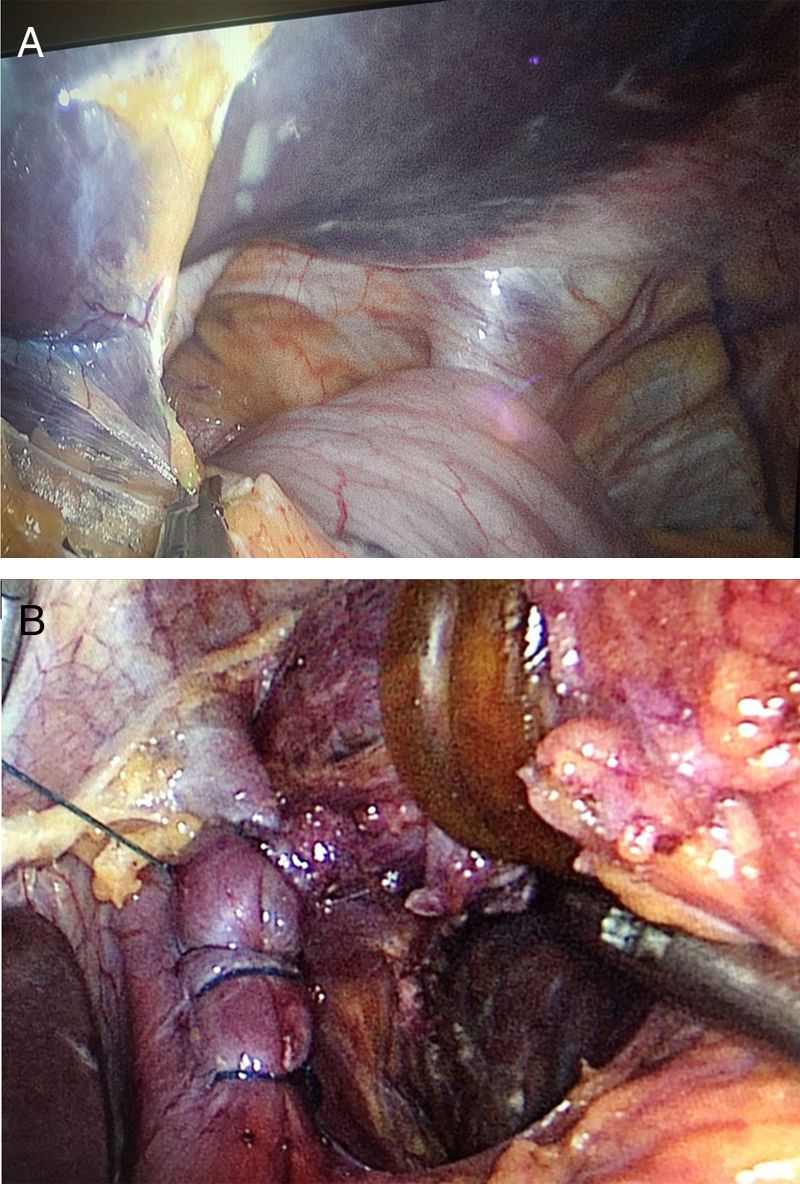
We present the case of a 60-year-old woman with a history of type 2 diabetes mellitus, dyslipidemia, and symptoms of pyrosis and regurgitation. Despite taking pantoprazole at 40mg/day, her symptom control was poor. She came to our consultation with a weight of 76kg, a height of 1.59m and a BMI of 30kg/m2. Seven years earlier, she had undergone endoscopic sleeve gastroplasty, after which no significant weight loss was achieved, but the GERD symptoms had worsened progressively. An upper gastrointestinal series revealed a type II hiatal hernia and altered gastric morphology secondary to the POSE procedure (Fig. 1). An upper gastrointestinal endoscopy showed grade C esophagitis according to the Los Angeles classification; biopsies were taken, which had an appearance of chronic esophagitis and no signs of metaplasia. The esophageal manometry presented a hypotensive lower esophageal sphincter (resting pressure 2mmHg), while pH-metry showed a DeMeester score of 21.5 and a pH<4 7% of the time.
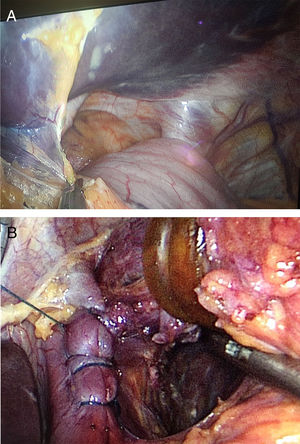
Given the modified anatomy of the stomach and the presence of diabetes mellitus and dyslipidemia, we decided to perform a one-anastomosis gastric bypass (OAGB) for metabolic purposes. Intraoperatively, a large hiatal hernia was observed that involved the gastric fundus and body (Fig. 2A). The herniated stomach was reduced, the crura of the diaphragm were dissected and the hernia defect was closed with continuous barbed suture (V-Loc® 2/0, Medtronic, USA) (Fig. 2B).
Afterwards, a gastric pouch measuring 20cm in length was constructed together with a mechanical side-to-side gastro-jejunal anastomosis (I-Drive®, Medtronic, USA) measuring 2.5cm in diameter using Tri-staple® cartridges (Medtronic, USA). The orifices were also sutured with continuous V-Loc® 2/0 barbed sutures. The length of the biliopancreatic loop was 250cm and the length of the common loop was 350cm. During the creation of the gastric pouch, some sutures of the previous endoscopic gastroplasty were cut, although this did not hinder correct stapling of the tissue.
The postoperative period was uneventful, and the patient was discharged 24h after surgery. One year after the procedure, the patient is asymptomatic, and the signs of esophagitis have disappeared in the upper GI endoscopy. The patient's diabetes mellitus was completely resolved (glycemia 102.9mg/dL and glycosylated hemoglobin 5.4%, with no medication) as was her dyslipidemia (total cholesterol 182mg/dL, triglycerides 141mg/dL and HDL 51mg/dL, also with no medication), and the patient had a BMI of 25kg/m2. In treatment with 2 tablets of multivitamin complex per day and one ampoule of vitamin D per week, the patient did not present protein, vitamin or mineral deficiencies on follow-up blood work.
Although fundoplication is the treatment of choice for non-pharmacologically controlled GERD, in patients with anatomical modifications of the stomach, this technique is difficult or even impossible to perform. The Roux-en-Y gastric bypass has been classically proposed as the alternative procedure in the surgical treatment of GERD in obese patients or those who are not candidates for fundoplication.6
In terms of weight loss and the resolution of comorbidities, results are excellent after OAGB, with high rates of remission of diabetes mellitus, hypertension and dyslipidemia, all of which are around 95% after 5 years.7 The main criticism of the technique (alkaline reflux and its effects) has been overcome with the modifications described by Carbajo et al.,7 including the creation of a long gastric reservoir measuring 18–20cm and a continuous side-to-side suture to affix the intestinal loop to the gastric pouch for 8–10cm. After 1200 interventions, the reflux rate described by Carbajo et al. was 2%. Mahawar8 has stated that the presence of bile in the gastric pouch of an asymptomatic patient has not proven to be harmful in the short term. The creation of a long reservoir reduces the possibility of gastroesophageal bile reflux, although eliminating it completely is not possible. Esophageal bile reflux, and even laryngeal reflux, have even been reported for intact stomachs and in the presence of the pylorus, although this is usually dysfunctional.9 Approximately 1% of patients undergoing a mini-gastric bypass have persistent GERD symptoms and require reoperation. The ideal length of the pouch to minimize reflux-related symptoms is even more controversial, although it is recommended that this should be as long as possible, while always preserving correct emptying of the bypassed segment. A narrow reservoir also implies lower acid secretion, thus minimizing the appearance of GERD and even marginal ulcers.10
Please cite this article as: Ruiz-Tovar J, Carbajo MA, Jimenez JM, Ortiz-de-Solorzano J, Castro MJ. Enfermedad por reflujo gastroesofágico en un paciente con un IMC 30kg/m2 y gastroplastia vertical endoscópica previa: indicación para un bypass gástrico de una anastomosis. Cir Esp. 2019;97:416–418.