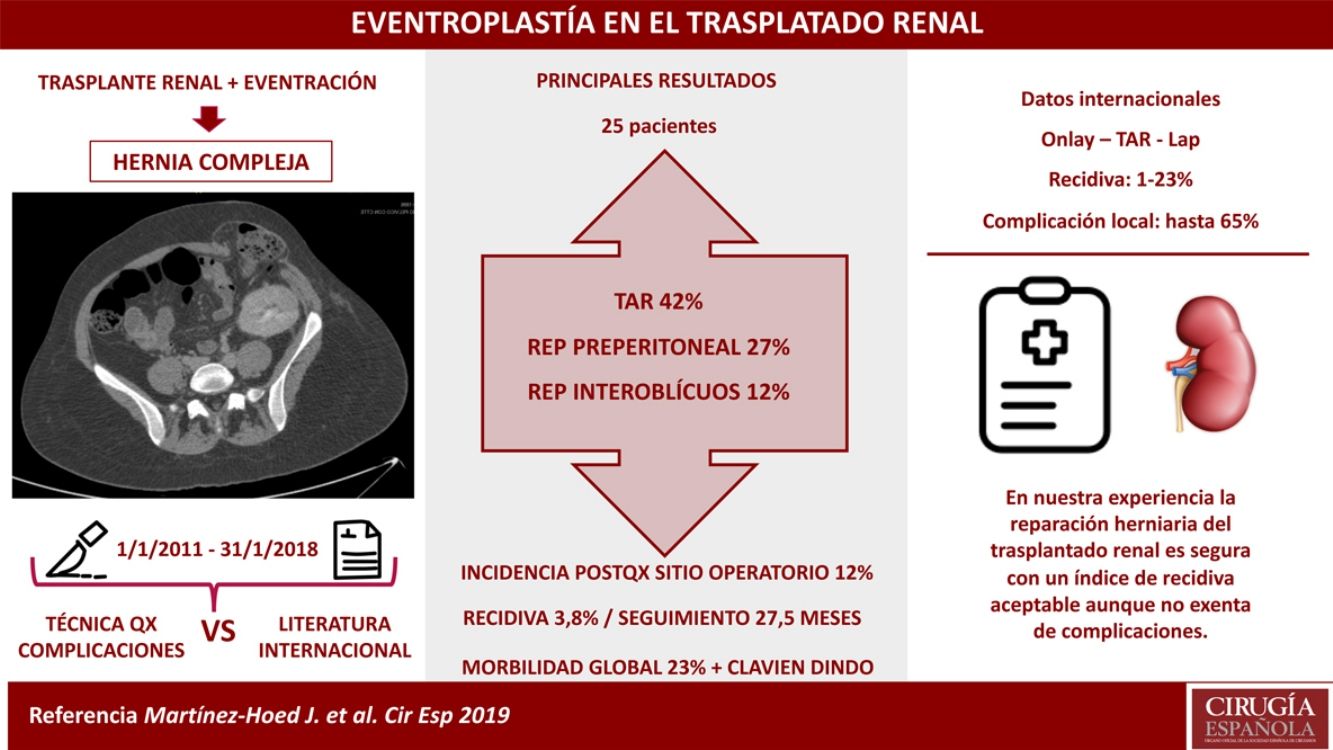
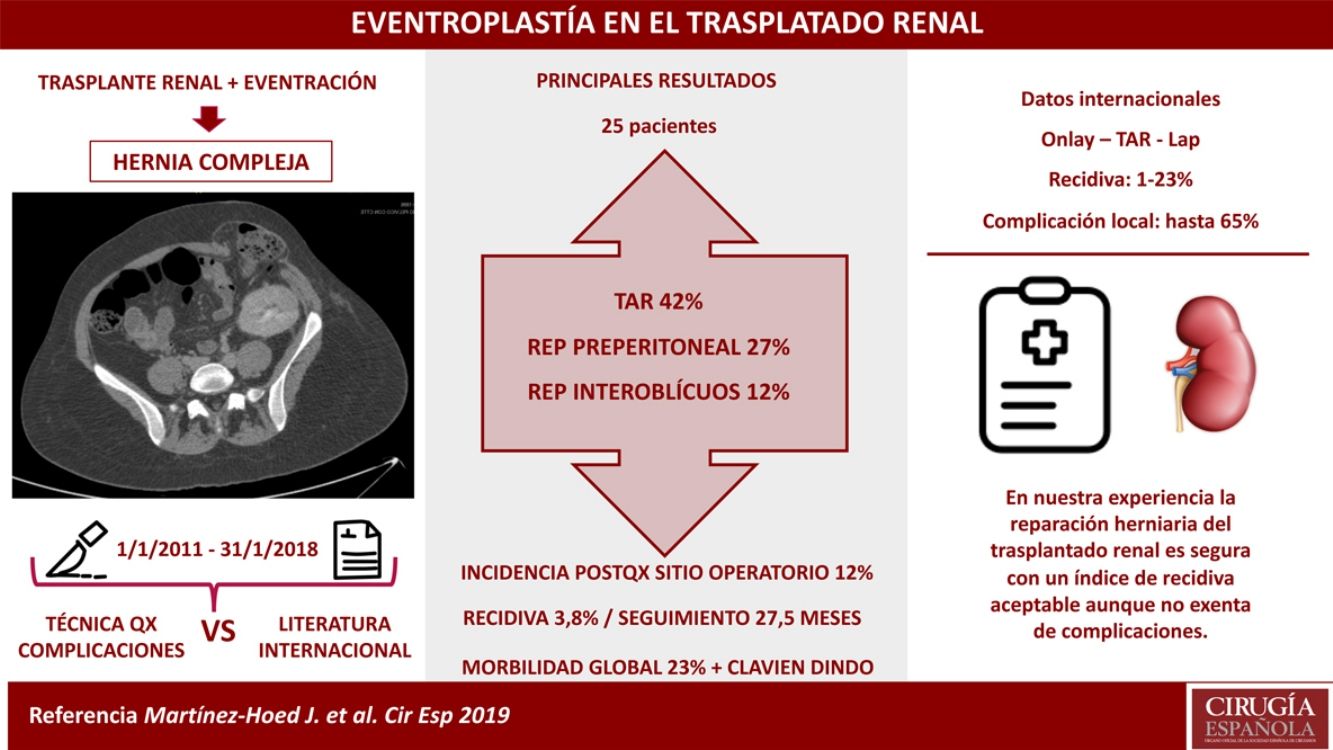
Incisional hernias secondary to renal transplantation (IHRT) are considered complex hernias because they are lateral to the sheath of the rectus abdominis muscle. The presence of the graft in the iliac fossa and the proximity to the inguinal area, costal margin and iliac bones, as zones with difficult fixation for prostheses, increases repair complexity. In addition, these patients have specific characteristics, such as treatment with immunosuppressive medication, that could alter postoperative evolution. The objective of this study was to analyze the results obtained in IHRT repair at a tertiary hospital, and to compare these data with the international literature.
MethodsRetrospective observational study of patients treated surgically for IHRT in our unit from January 1, 2011 to January 31, 2018. Preoperative conditions, intraoperative factors and postoperative complications during follow-up were analyzed.
ResultsTwenty-five patients underwent hernia repair, finding a 4% hernia recurrence rate during a median follow-up of 27.5 months (20–39). The most frequently used technique was the posterior transversus abdominis release component separation technique in 42%, followed by preperitoneal repair in 27% and interoblique repair in 12%. The overall postoperative morbidity was 23%, which was frequently related to the surgical site (12%).
ConclusionsIHRT repair is a safe procedure at our medical center, with an acceptable rate of hernia recurrence, but it is not without complications.
Las hernias incisionales secundarias al trasplante renal (HITR) se consideran hernias complejas debido a su localización lateral a la vaina del músculo recto abdominal. También influyen la presencia del injerto en la fosa iliaca y la proximidad del área inguinal, el margen costal y los huesos iliacos como rebordes de difícil fijación de la prótesis. Además, estos pacientes presentan connotaciones específicas, como el tratamiento con inmunosupresores, que podrían alterar la evolución postoperatoria. El objetivo del estudio fue analizar los resultados obtenidos en la reparación de las HITR en un hospital terciario, comparando estos datos con la literatura internacional.
MétodosEstudio observacional retrospectivo, desde el 1 de enero de 2011 al 31 de enero de 2018, de los pacientes operados de HITR en nuestra unidad. Análisis de factores preoperatorios, intraoperatorios y de complicaciones postoperatorias observados durante el seguimiento.
ResultadosSe operaron 25 pacientes, encontrando un índice de recidiva herniaria del 4% tras un seguimiento mediano de 27,5 meses (20-39). La técnica más utilizada fue la separación posterior de componentes con liberación del transverso en un 42%, seguida de la reparación preperitoneal en un 27% y la reparación interoblicuos en un 12%. La morbilidad postoperatoria global fue del 23%, siendo las más frecuentes las relacionadas con el sitio quirúrgico (12%).
ConclusionesLa reparación de las HITR es un procedimiento seguro en nuestro centro, con un índice de recidiva herniaria aceptable, aunque no exento de complicaciones.
Renal transplantation can be carried out through a variety of approaches, using incisions such as the pararectal, oblique, paramedial or the so-called ‘hockey stick’, depending on the choice of the surgeon and the hospital. All these incisions have in common that they may later give rise to a lateral hernia of the abdominal wall.1
Incisional hernias after renal transplantation (IHRT) are defined as complex due to the laterality of the hernia defect and the proximity of the semilunar line, inguinal area, costal margin and iliac bones, which are an added difficulty because of their problematic ridges for prosthetic mesh fixation.2–4
Furthermore, these patients present associated comorbidities and the use of immunosuppressive medication, which are factors that can increase postoperative morbidity rates related to hernia repair.1 Likewise, the location of the renal graft also adds complexity to the surgery due to its close proximity to the defect to be repaired.
The incidence of IHRT reported in the literature is 3.2% (range 1.1% to 7%). This rate is not as high as the frequency of incisional hernias related to liver transplantation, which can reach 30%.1,5 There is great heterogeneity in the surgical technique due to a lack of standardization for the repair, and even the recurrence rates are highly variable in the literature, ranging between 0 and 20%.6,7
The objective of this study was to retrospectively analyze the results of IHRT repair in an Abdominal Wall Surgery Unit and, in turn, to compare the results obtained with what has been published to date in the international literature.
MethodsWe conducted a retrospective review of all patients who underwent surgical IHRT repair from January 1, 2011 to January 31, 2018 at our hospital. Exclusion criteria were: children under the age of 18, non-functioning renal grafts, incisional hernias not associated with kidney transplantation incision, and urgent hernia repairs performed in these patients.
All patients were studied preoperatively by means of a computed tomography (CT) scan in order to classify the type of incisional hernia according to the European Hernia Society (EHS) classification and to plan preoperative treatment as well as surgery.2 Data provided by the CT scan in terms of diameters of the defect and hernia sac, as well as hernia and abdominal cavity volumes, were used for preoperative preparation of the patients. In addition, we assessed the suitability and possible use of preoperative progressive pneumoperitoneum (PPP) or botulinum toxin (BTX). In cases of hernia orifices with transverse diameters greater than 12cm, preoperative BTX was indicated. In patients who presented hernias with loss of domain or a Tanaka index greater than 20%, the combination of BTX and PPP was indicated.8,9
All surgical cases were included in the Spanish National Incisional Hernia Registry, (EVEREG).10 This study received the approval of the hospital's Ethics Committee and was conducted in accordance with data protection regulations, with informed patient consent.
Before surgery, all IHRT cases were assessed by the Nephrology Service, who adjusted the immunosuppressive treatment preoperatively and optimized the patient's metabolic condition. All patients received thromboembolic prophylaxis using enoxaparin the day before surgery, compression stockings, and antibiotic prophylaxis with amoxicillin and clavulanic acid 30min before the skin incision. Ciprofloxacin was used in individuals allergic to amoxicillin. All patients had urinary catheterization to control diuresis and intra-abdominal pressure, thereby minimizing bladder injuries during surgical dissection.
The 5 surgeons of the unit participated in the IHRT repairs, performing the technique according to the type of hernia, location and size of the hernia defect, and using various repair types to complete the reconstruction of the abdominal wall. In all cases, Redon drains were placed to minimize the development of postoperative seroma.
The patients were followed up with postoperative visits to the outpatient consultations 15, 30 and 90 days after surgery, then after 6 months, one year, and annual visits until completing a follow-up period of 3 years, which we tried to complete in most of the patients. Hernia recurrence was defined clinically by examination of the patient during the office visit, and, when there was suspicion, CT scan was performed for confirmation.
The following epidemiological data were collected: age, gender, associated diseases, smoking, obesity (body mass index), immunosuppressive medication, anticoagulant medication, and ASA classification. Factors related to surgical repair were also analyzed: defect size and location according to the EHS classification, Tanaka index, type of repair conducted, mesh used, possibility of primary closure of the defect, and duration of the surgery. Intraoperative complications and associated procedures were also recorded. Postoperative complications were classified according to Clavien-Dindo,11 and we also registered postoperative hospital stay, follow-up time, and the need for hospital readmission.
We performed a basic descriptive statistical analysis using frequencies and percentages for categorical variables, and based on means, medians, ranges and standard deviations for quantitative variables, supported by the SPSS version 20.0 program. Lastly, a review of the literature was carried out from January 1, 1998 to February 1, 2019, searching PubMed and SciELO with the keywords“incisional hernia”, “kidney transplantation”, “hernia incisional y trasplante renal”. Out of the 23 scientific articles found, 10 were excluded because they did not contain the main parameters of the analysis.
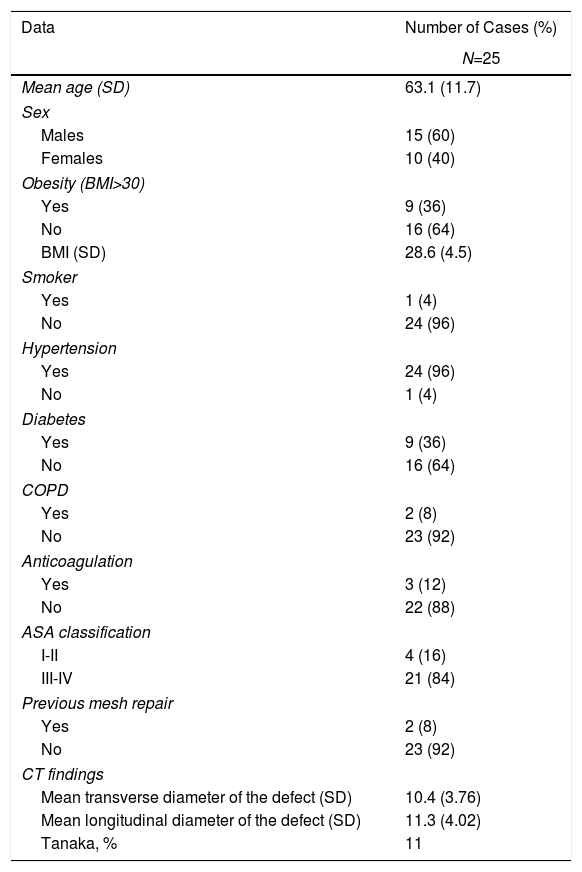
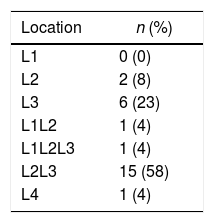
ResultsFrom January 1, 2011 to January 31, 2018, we operated on 25 patients with IHRT. Table 1 shows the main demographic data of the series and CT scan results. The classification of IHRT in accordance with EHS criteria is shown in Table 2. All the cases had a history of having undergone surgery on the iliac fossa for pararectal and oblique incisions for transplantation.
Demographic Data of Patients Treated Surgically for Incisional Hernia Secondary to Renal Transplantation Between January 1, 2011 and January 31, 2018.
| Data | Number of Cases (%) |
|---|---|
| N=25 | |
| Mean age (SD) | 63.1 (11.7) |
| Sex | |
| Males | 15 (60) |
| Females | 10 (40) |
| Obesity (BMI>30) | |
| Yes | 9 (36) |
| No | 16 (64) |
| BMI (SD) | 28.6 (4.5) |
| Smoker | |
| Yes | 1 (4) |
| No | 24 (96) |
| Hypertension | |
| Yes | 24 (96) |
| No | 1 (4) |
| Diabetes | |
| Yes | 9 (36) |
| No | 16 (64) |
| COPD | |
| Yes | 2 (8) |
| No | 23 (92) |
| Anticoagulation | |
| Yes | 3 (12) |
| No | 22 (88) |
| ASA classification | |
| I-II | 4 (16) |
| III-IV | 21 (84) |
| Previous mesh repair | |
| Yes | 2 (8) |
| No | 23 (92) |
| CT findings | |
| Mean transverse diameter of the defect (SD) | 10.4 (3.76) |
| Mean longitudinal diameter of the defect (SD) | 11.3 (4.02) |
| Tanaka, % | 11 |
In 3 patients, we observed associated midline defects, especially M3 hernias, which required joint repair with the IHRT procedure. Among these cases, 2 had a history of urgent midline laparotomy (supra and infraumbilical), and another patient had a recurrent umbilical hernia. The combination of preoperative PPP and BTX was used in 5 patients due to the size of the defects, and only in one case was BTX exclusively used in order to perform a repair with less tension due to a transverse defect diameter greater than 12cm.
The skin incisions used were the same as those for renal transplantation in 75% (pararectal and oblique incision), and midline infraumbilical incision was used in 25%. At the beginning of the series (year 2011), bridge prosthesis techniques were used, without closing the hernia defect in 4 patients. Subsequently, the most widely used techniques were the separation of components with transverse abdominis release (TAR) in 42% (11 cases), followed by preperitoneal repair in 27% (7 patients) and interoblique repair in 12% (3 cases).
Regarding prosthetic implants, double mesh was used in 62% (16 patients) of the surgeries, and in 85% of cases the prosthetic material used allowed contact with the intestines. Overall, the most commonly used prosthetic material was polyvinylidene fluoride (PVDF) in 50% of cases, followed by polypropylene in 40%. The position, number, fixation method and combination of prosthetic mesh used was determined by the surgeon's own criteria.
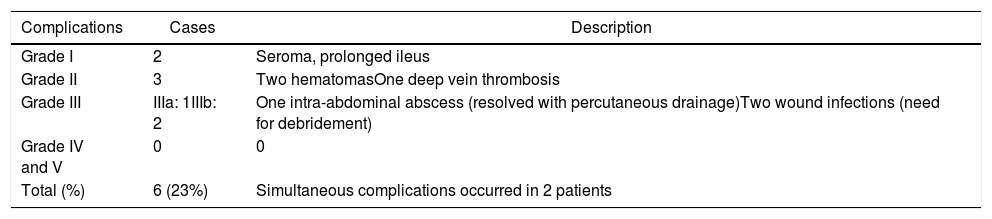
The overall postoperative morbidity was 23%. Table 3 shows the distribution of postoperative complications according to the Clavien-Dindo classification. There were no postoperative deaths associated with the hernia repair. Two patients required reoperation due to surgical site infection, as surgical debridement was needed for its resolution. There was no case of prosthetic infection. The average hospital stay was 8.4 days (3–20).
Classification of the Postoperative Complications of Patients Treated Surgically for Incisional Hernia Secondary to Renal Transplantation According to Clavien-Dindo.
| Complications | Cases | Description |
|---|---|---|
| Grade I | 2 | Seroma, prolonged ileus |
| Grade II | 3 | Two hematomasOne deep vein thrombosis |
| Grade III | IIIa: 1IIIb: 2 | One intra-abdominal abscess (resolved with percutaneous drainage)Two wound infections (need for debridement) |
| Grade IV and V | 0 | 0 |
| Total (%) | 6 (23%) | Simultaneous complications occurred in 2 patients |
After a mean postoperative follow-up of 27.5 months (range 20–39), we found a hernia recurrence rate of 4% (one case), with a completed follow-up of 24 months in 70% of patients. One patient died one year after the procedure due to pulmonary causes not related to the hernia surgery.
In the case of recurrence, the first surgery consisted of a L3W3 IHRT repair using a ‘bridge prosthesis’ for the defect. After four years of follow-up, a recurrence was discovered, and TAR was performed to resolve it. After this last surgery, 3 years of follow-up have been completed, and no new recurrence has been detected in a series of studies.
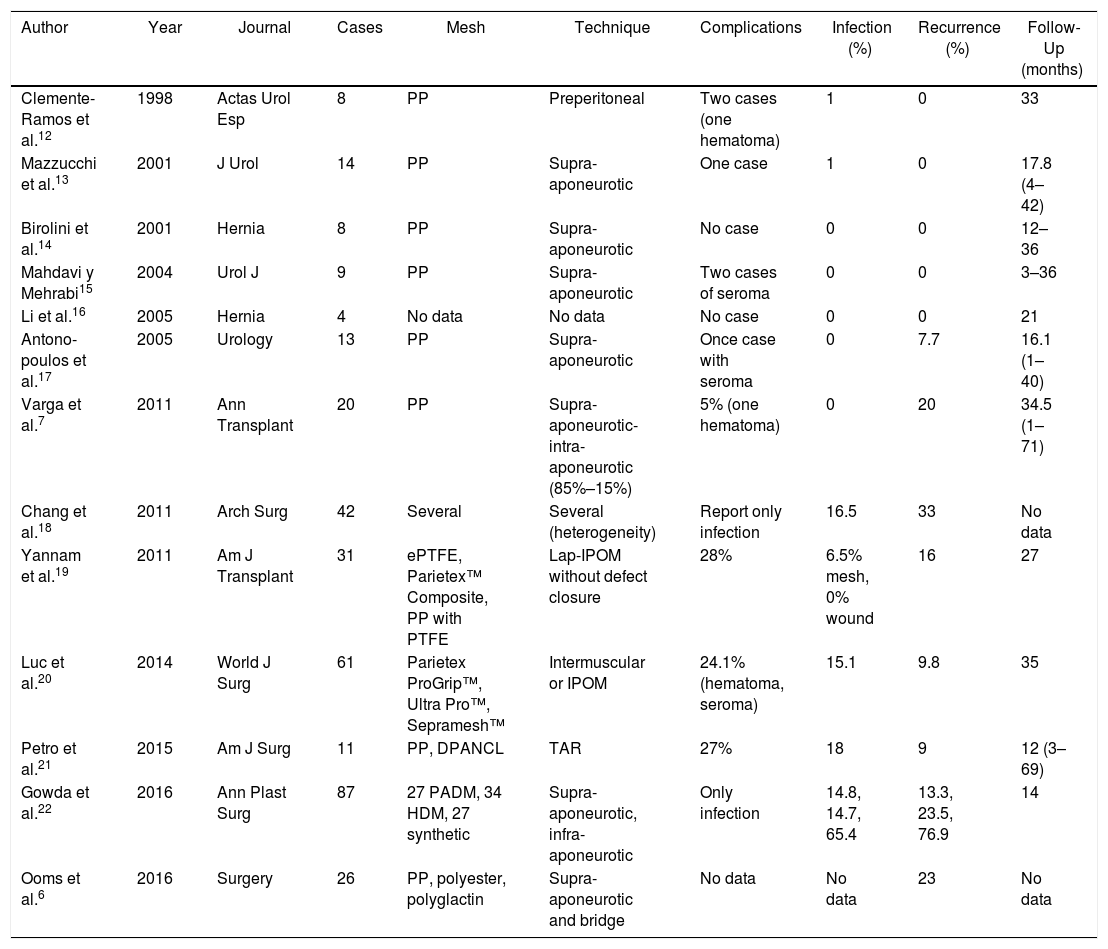
Table 4 summarizes the series published in the international literature in the period from January 1, 1998 to February 1, 2019.6,7,12–22
Series Published in the International Literature About Incisional Hernia Secondary to Renal Transplantation Between 1998 and 2018.
| Author | Year | Journal | Cases | Mesh | Technique | Complications | Infection (%) | Recurrence (%) | Follow-Up (months) |
|---|---|---|---|---|---|---|---|---|---|
| Clemente-Ramos et al.12 | 1998 | Actas Urol Esp | 8 | PP | Preperitoneal | Two cases (one hematoma) | 1 | 0 | 33 |
| Mazzucchi et al.13 | 2001 | J Urol | 14 | PP | Supra-aponeurotic | One case | 1 | 0 | 17.8 (4–42) |
| Birolini et al.14 | 2001 | Hernia | 8 | PP | Supra-aponeurotic | No case | 0 | 0 | 12–36 |
| Mahdavi y Mehrabi15 | 2004 | Urol J | 9 | PP | Supra-aponeurotic | Two cases of seroma | 0 | 0 | 3–36 |
| Li et al.16 | 2005 | Hernia | 4 | No data | No data | No case | 0 | 0 | 21 |
| Antono-poulos et al.17 | 2005 | Urology | 13 | PP | Supra-aponeurotic | Once case with seroma | 0 | 7.7 | 16.1 (1–40) |
| Varga et al.7 | 2011 | Ann Transplant | 20 | PP | Supra-aponeurotic-intra-aponeurotic (85%–15%) | 5% (one hematoma) | 0 | 20 | 34.5 (1–71) |
| Chang et al.18 | 2011 | Arch Surg | 42 | Several | Several (heterogeneity) | Report only infection | 16.5 | 33 | No data |
| Yannam et al.19 | 2011 | Am J Transplant | 31 | ePTFE, Parietex™ Composite, PP with PTFE | Lap-IPOM without defect closure | 28% | 6.5% mesh, 0% wound | 16 | 27 |
| Luc et al.20 | 2014 | World J Surg | 61 | Parietex ProGrip™, Ultra Pro™, Sepramesh™ | Intermuscular or IPOM | 24.1% (hematoma, seroma) | 15.1 | 9.8 | 35 |
| Petro et al.21 | 2015 | Am J Surg | 11 | PP, DPANCL | TAR | 27% | 18 | 9 | 12 (3–69) |
| Gowda et al.22 | 2016 | Ann Plast Surg | 87 | 27 PADM, 34 HDM, 27 synthetic | Supra-aponeurotic, infra-aponeurotic | Only infection | 14.8, 14.7, 65.4 | 13.3, 23.5, 76.9 | 14 |
| Ooms et al.6 | 2016 | Surgery | 26 | PP, polyester, polyglactin | Supra-aponeurotic and bridge | No data | No data | 23 | No data |
NCLAPD: non-cross-linked acellular porcine dermis; ePTFE: expanded polytetrafluoroethylene; HDM: human dermal matrix; IPOM: intraperitoneal onlay mesh; Lap-IPOM: laparoscopic intraperitoneal mesh; TAR: transversus abdominis muscle release; PADM: porcine acellular dermal matrix; PP: polypropylene; PTFE: polytetrafluoroethylene.
There are few published studies that analyze the results of IHRT repairs. In our hospital, and over a period of 7 years, we have only operated on 25 patients with these characteristics. We feel that this is a low number, as our unit is a specialized surgery unit where these complex cases are referred from other medical centers, and also taking into account that approximately 665 kidney transplantations were performed at our hospital during the study period.
This could be explained by several factors: lack of diagnosis by the nephrologist as it is a hernia with peculiar characteristics; patient reluctance to report the issue due to a negative, prolonged experience with chronic kidney disease; and, lastly, the actual incidence of this type of complex hernias is not very high due to the pararectal or lateral incision, considered to be below 7%.1,12
The size of the hernia defect also adds special complexity to this type of hernia. In our experience, the transverse hernia diameter was greater than 10cm (W3) in 50% of cases. For the preoperative study, we relied on CT scan and the EHS classification in order to unify the wide heterogeneity of IHRT that we found.2 It is important to note that, after reviewing the literature, no authors mention this classification, at least as a study objective. Nor did we find any references in the literature describing the need for techniques like BTX or PPP in the management of IHRT, despite being, in many cases, very bulky defects. Our experience in preconditioning and the use of these preoperative measures allowed us to facilitate and successfully resolve the repair in 5 patients.9
Regarding the type of reconstruction to be performed, for the “onlay” or supra-aponeurotic technique, highly variable recurrence rates have been reported. Thus, Birolini et al. suggest that this repair type should always be performed because the preperitoneal situation is very difficult to achieve due to the presence of the transplanted kidney.14 Other less frequent reconstruction techniques could have a role in certain situations, such as in major hernia defects, very bulky hernias, or with the involvement of the external oblique muscle in the hernia sac. Thus, intermuscular repair is advocated, dissecting the space between the oblique muscles, similar to hemilateral anterior component separation. Veyrie et al.23 performed this approach in 61 cases of lateral hernias, although not secondary to kidney transplantation, indicating that it allows for less tissue dissection, with a recurrence rate of 4.9%.23 Other authors have proposed the use of intraperitoneal prosthetic mesh, using them as bridges in very large defects.4,19 At the beginning of our series, we used this approach in 3 patients, where we were unable to perform complete fascial closure. One of them was the only patient with IHRT who presented recurrence 4 years after repair, which we successfully resolved with a preperitoneal repair.20,21
It is this heterogeneity in the IHRT surgical technique that has undergone an important change with the advent of TAR in recent years. This, in our opinion, improves the management of these patients. In fact, it is the only repair that we have performed in the last 3 years of the study, with low rates of postoperative morbidity and no observed recurrence in the 11 patients treated. These findings are corroborated by Petro et al., who obtained a recurrence rate of 9%, with an average follow-up of 12 months. This shows that the use of the preperitoneal plane for IHRT repair is ideal, since the prosthesis remains in a space with less possibility of infection, thereby minimizing surgical site complications.12,21
Despite negative factors, such as the existence of immunosuppression or the comorbidity associated with these patients, we feel that the results of our series regarding recurrence rate and postoperative morbidity are good. This was undoubtedly influenced by the multidisciplinary preoperative patient optimization carried out by the Nephrology and Urology Departments in conjunction with our group. In certain patients, for example, the modification of the immunosuppressive treatment by Nephrology (substituting sirolimus with everolimus) provided the advantage of improved healing and reduced probability of infection, since this drug is related to 36% of surgical wound complications.24 On the other hand, during the postoperative period, such optimization would involve protecting the function of the transplanted kidney through the supply of fluids, adjusting the medication and avoiding nephrotoxic drugs during follow-up. For this reason, we feel that the specialization of the hospital in abdominal wall defects is important, as is the support of other specialized units involved in kidney transplantation, all of which contribute to good outcomes.
There is an evident variability in terms of IHRT recurrence, ranging from 1 to 23%.1,7,22 Our study achieved a rate of 4%, a result that we think is excellent if we consider that 50% were W3 hernias. In addition, when we compare this datum with EVEREG data, it is lower than the rates from 2018 (between 5.4 and 8%) if we analyze lateral hernias, so the management of this disease in specialized units may contribute to improved results in terms of recurrence. In terms of morbidity, most of these complications were minor and in range with the literature reviewed, and there were no cases of mortality related with the repair during follow-up.20 It is worth noting the 12% rate of surgical site complications, mostly superficial wound infection and hematomas, which is an adequate percentage given the complexity of these patients due to immunosuppression, anatomical difficulties and the presence of the renal graft.20,22,25
This study is not without limitations. On the one hand, the retrospective analysis of the series is limited by the information found in the unit's database as well as observer bias. At first glance, 25 cases may seem a limited case series to draw conclusions, but this number is higher than in the rest of the series analyzed. Furthermore, a longer postoperative follow-up in all patients would have contributed more information. Another factor that may bias the conclusions was the heterogeneity of the surgical techniques performed until the advent of TAR, something that also occurs in all the studies analyzed. For this reason, more prospective studies are necessary to compare different surgical techniques in order to reach a consensus on the best approach for IHRT.
In conclusion, although IHRT repair is not without complications, at our hospital it is a safe procedure with an acceptable hernia recurrence rate. Preoperative optimization, a multidisciplinary approach, the use of preoperative techniques such as BTX and PPP, and an accumulated experience in the TAR technique have played a part in these results.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Martínez-Hoed J, Bonafe Diana S, Torregrosa-Gallud A, García Pastor P, Abelló Audi D, Menéndez-Jiménez de Zavada y Lissón M, et al. Resultados de la reparación de la hernia incisional asociada al trasplante renal en un centro especializado. Análisis de nuestra experiencia de 7 años. Cir Esp. 2020;98:350–356.
This paper was partially presented as an oral communication on May 9, 2019 at the 15th National Conference on Abdominal Wall Surgery, Valencia, Spain.