Incidence of gallbladder polyps is 0,3–12%. It is important to differentiate pseudopolyps (cholesterol polyps, adenomyomatosis, inflammatory polyps), which do not have the capacity to become malignant, from true polyps (adenomas and adenocarcinomas). The main risk factors for malignancy are >6−10 mm, growth, sessile morphology, Indian ethnicity and primary sclerosing cholangitis. Ultrasound is the gold standard for diagnosis. Most polyps diagnosed by ultrasound are pseudopolyps. The main objective of this study is to analyse whether ultrasound is accurate for diagnosing true polyps in patients undergoing surgery for this reason.
MethodsRetrospective observational study with prospective data entry of patients undergoing elective cholecystectomy for gallbladder polyps from 2007 to 2021. Surgery was indicated in symptomatic patients and in those with risk factors. The study has been approved by the Clinical Research Ethics Committee of our hospital.
ResultsWe included 124 patients in our study. An elective laparoscopic cholecystectomy was performed in all of them. The mean age was 55,4 years and 61% were women. Of all patients, 65% were symptomatic at diagnosis. Only 3 patients had true polyps (2,4%). All of them were tubular adenomas. The rest of patients were false positives (97,6%). The adenoma size was 11, 6 and 5 mm, respectively. The surgical indication was due to polyp size or due to associated biliary symptoms.
ConclusionUltrasonography is not accurate for the diagnosis of gallbladder polyps. Validation of other complementary tests for the diagnosis of gallbladder polyps in asymptomatic patients could be relevant to avoid unnecessary surgeries.
La incidencia de pólipos vesiculares es del 0,3–12%. Es importante diferenciar los pseudopólipos (pólipos de colesterol, adenomiomatosis o pólipos inflamatorios) de los pólipos verdaderos (adenomas y adenocarcinomas). Los principales factores de riesgo de malignización son el tamaño superior a 6−10 mm, crecimiento rápido del mismo, morfología sésil, etnia india y colangitis esclerosante primaria. La ecografía es el gold standard para su diagnóstico. Sin embargo, la mayoría de los pólipos diagnosticados por ecografía son pseudopólipos. El objetivo del estudio es analizar si la ecografía es precisa para diagnosticar los pólipos verdaderos en los pacientes cuya indicación quirúrgica ha sido este diagnóstico ecográfico.
Material y métodosEstudio observacional retrospectivo de los pacientes intervenidos en nuestro centro, desde el año 2007 al 2019, de colecistectomía electiva por presentar pólipos vesiculares. La cirugía se indicó en pacientes sintomáticos y/o con factores de riesgo.
ResultadosSe han incluido 124 pacientes. En todos ellos se ha realizado colecistectomía laparoscópica. La edad media fue de 55,4 años y el 61% eran mujeres. El 65% tenían síntomas biliares. En nuestro estudio, 3 pacientes presentaron pólipos verdaderos (2,4%). Todos ellos, fueron adenomas tubulares. El resto de los pacientes resultaron falsos positivos (97,6%). El tamaño de los adenomas fue de 11, 6 y 5 mm. La cirugía se indicó por tamaño o por clínica asociada.
ConclusionesLa ecografía no es precisa para el diagnóstico de pólipos vesiculares verdaderos. La validación de otras pruebas complementarias para el diagnóstico de pólipos en pacientes asintomáticos podría ser relevante para evitar cirugías innecesarias.
On ultrasound, gallbladder polyps are defined as elevations of the gallbladder wall that protrude into the lumen.1–3 They are immobile, have no posterior acoustic shadowing, and are detected incidentally in 0.3%–12% of the population studied by ultrasound.2,4–7 In recent years, the increased use of ultrasound as a diagnostic tool has led to more diagnoses of gallbladder polyps.5
It is important to differentiate pseudopolyps (cholesterol polyps, foci of adenomyomatosis, inflammatory polyps, hyperplastic polyps) from true polyps (adenomas, adenocarcinomas).8,9 The vast majority of polyps detected by ultrasound are cholesterol polyps or adenomyomatosis, with no risk of malignancy.4 However, 1%–12% of cholecystectomy specimens contain true polyps,3,10 and only 3%–8% of these will present malignant disease in the histological analysis.4
The differential diagnosis of the main gallbladder lesions is shown in Table 1.7,9–12
Differential diagnosis of main gallbladder lesions.
| Histology | Ultrasound | |
|---|---|---|
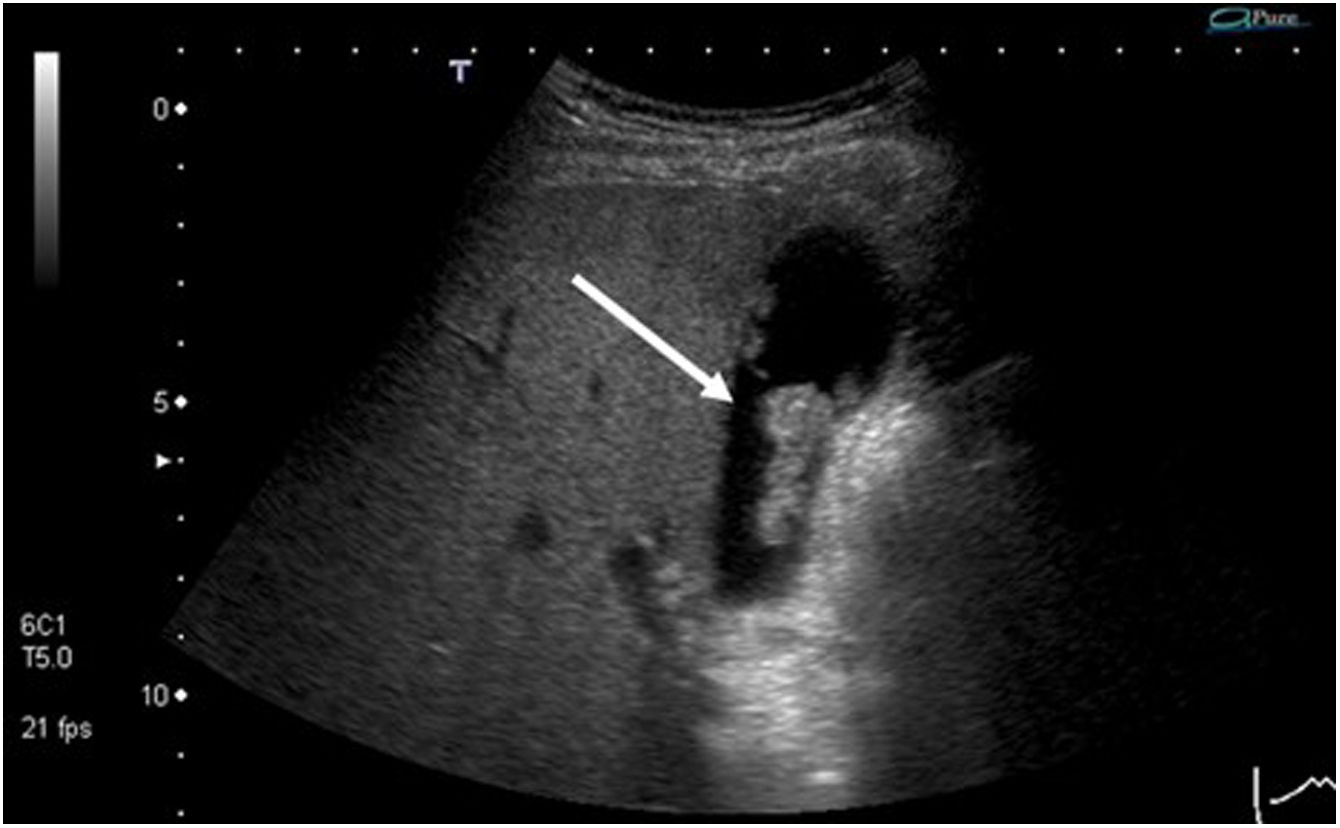
| Cholesterol polyp | Cholesterol deposits in the interior of the macrophages in the lamina propia of the gallbladder wall | Hyperechoic structure, no posterior acoustic shadow, and does not vary position with patient movement (Fig. 1) |
| Inflammatory polyp | Process of granulation and fibrosis of the tissue, consequence of chronic vesicular inflammation | Very variable ultrasound presentation |
| Adenomyomatosis | Proliferation of epithelium with hypertrophy of the muscular layer with invaginations of hypertrophic mucosa through the thickened muscular layer (Rokitansky-Aschoff sinusoids); may be diffuse, segmental or focal. | Wall thickening with cystic spaces and comet-tail artifact (hyperechoic focus with posterior acoustic reverberation in the shape of an inverted triangle, with gradual decrease in echogenicity [Fig. 2]) |
| Adenoma | Risk of malignant degeneration; may be sessile or pedunculated.Most frequent histologies: tubular, papillary or tubulopapillary | Homogenous on ultrasound, with echogenicity similar to the liver (Fig. 3). |
| Adenocarcinoma | Malignant lesionPossible invasion of adjacent structures | Hyperechogenic, heterogeneous masses with vascularization visible by eco-Doppler and irregular margins |
Due to the poor prognosis of gallbladder adenocarcinoma, early identification of cases with the greatest potential for malignant degeneration is of vital importance.
Several studies have attempted to establish the risk factors for malignancy of gallbladder polyps. The most commonly accepted are:2,4,5,7,10
- -
Size greater than 6 mm (greater than 10 mm in certain studies).2,7,12
- -
Growth of the polyp during the follow-up period (especially if the growth is pronounced and rapid10).
- -
Sessile morphology.
- -
Indian ethnicity.
- -
Single polyps.
- -
Primary sclerosing cholangitis.
Other possible risk factors have been suggested (age >50–60, concomitant cholelithiasis, biliary colic symptoms, etc), but the results have not been conclusive.2,4–6
Cholecystectomy is indicated in patients with lesions compatible with polyps that meet the risk criteria mentioned above.
Ultrasound has been considered the gold standard for diagnosis, since it is a non-invasive, cheap and easily accessible test. However, it is operator-dependent and limited by several factors, such as Body Mass Index (BMI), interposition of intestinal gas or intrathoracic gallbladder.
In recent years, the question has been raised whether the decision for surgical management should be based exclusively on ultrasound findings, as a poor correlation has been observed between ultrasound and pathological findings.1,12
The sensitivity of transabdominal ultrasound is not very high for the diagnosis of true polyps (<70%); in contrast, its specificity is high (96%).2,13 Its positive predictive value is less than 15%, and its negative predictive value is close to 99%.1,13 These results can lead to numerous unnecessary surgeries, especially considering that most diagnosed polyps will not be real polyps.
Given these data, and even though the morbidity and mortality of laparoscopic cholecystectomy are low, the objective of our study is to analyze whether ultrasound is accurate to diagnose true polyps in patients whose surgical indication was based on ultrasound diagnosis.
MethodsWe have designed a retrospective, observational study with prospective data entry into the database of our General Surgery department. The study included patients who had undergone elective cholecystectomy at our medical center between 2007 and 2021 due to gallbladder polyps observed on ultrasound.
At our hospital, elective cholecystectomy surgery is indicated in patients with biliary symptoms and asymptomatic patients who present risk factors for malignancy, such as a polyp size greater than 10 mm, significant polyp growth observed on 2 consecutive imaging tests, and/or or concomitant cholelithiasis.1,7,8,10 The management algorithm for gallbladder polyps at our hospital is shown in Fig. 4.
In patients who do not meet the criteria for surgery, follow-up is carried out with ultrasound scans every 6 months during the first year, annually from the first to fifth years, and biannually thereafter, following the recommendations of most authors.1,7,10
This study has been approved by the Clinical Research Ethics Committee (2022/5058) of our hospital, and the principles for ethical human research have been followed in accordance with the Declaration of Helsinki.14 The STROBE15 guidelines for observational studies have been followed.
The study collected the following variables:
- -
Sex.
- -
Age.
- -
Symptoms of biliary origin.
- -
Polyp diagnosis method.
- -
Polyp size on ultrasound.
- -
Concomitant cholelithiasis.
- -
Histological result of the specimen (including size of the lesion).
The statistical analysis was conducted using the SPSS version 25. Continuous variables are presented as means ± standard deviation. Categorical variables have been expressed as percentages.
ResultsDuring the period of time studied, 124 patients with an ultrasound diagnosis of gallbladder polyp who met surgical criteria were included in the study. All patients were treated with elective laparoscopic cholecystectomy.
Mean patient age was 55.4 years (42.6–68.2), and a higher prevalence was observed in women (76 patients; 61%). At the time of diagnosis, 65% of patients had symptoms compatible with biliary colic.
Among the 124 patients included, only 3 patients had true polyps confirmed by the histopathological analysis (2.4%), and the remaining 121 were false positives (97.6% of patients). In all 3 cases, the histopathological result was tubular adenoma.
The adenomas were 11, 6 and 5 mm in size. In the first case, the surgical indication was due to polyp size, and the other 2 were due to associated biliary symptoms.
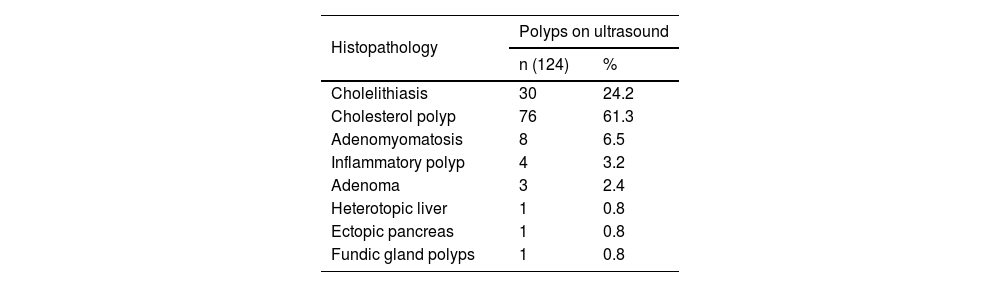
The remaining histopathological results are shown in Table 2.
DiscussionThe prevalence of true polyps detected in our study is similar to reports in the literature (<8%).3 A possible limitation of our study is selection bias, as only patients who had undergone surgery could be analyzed.
Ultrasound has a high rate of false positives in the diagnosis of gallbladder polyps, even when performed by expert radiologists.3 This raises the need to study alternatives to improve diagnostic accuracy, including the use of computed tomography (CT), magnetic resonance imaging (MRI), contrast-enhanced ultrasound, or endoscopic ultrasound.2,3
CT scans involve irradiating the patient and do not offer benefits over ultrasound in the diagnosis of these lesions, which is why its use is reserved for staging lesions suspected of malignancy.2,8,11
MRI can be useful in cases of uncertain diagnosis, although it is an expensive and lengthy test. It provides high-resolution images and allows for the assessment of the gallbladder and bile duct anatomy and function.16 The diffusion coefficient of true polyps is lower than that of pseudopolyps, although a greater number of studies would be required to standardize the use of MRI in the diagnosis of gallbladder polyps.2,8,12
Doppler ultrasound provides visualization of blood flow in the tissue to determine its characteristics. However, in most cases, it can only be used to evaluate larger vessels.17,18 The use of contrast material (Contrast Enhanced UltraSound, CEUS) facilitates dynamic, continuous, real-time study of the blood flow of the lesion, thus increasing the sensitivity of the technique and the diagnostic accuracy of malignant lesions.2,12,18,19 Due to the great variability described among studies, there is no clear consensus on what the signs of malignancy are, although the most widely accepted include: sessile morphology; heterogeneous, rapid contrast enhancement in the arterial phase with rapid washout in the venous phase; branched, dilated and irregular vessels; and invasion of the liver parenchyma.12,17–20 However, more studies are still required to standardize the use of CEUS in the diagnosis of these lesions.
Lastly, endoscopic ultrasound has been proposed as a useful tool to reduce the number of unnecessary cholecystectomies. This is an expensive and invasive test that is not available at all medical centers, but which allows a biopsy to be taken when necessary.2,18,21 Some studies have attributed the technique with greater sensitivity and specificity to differentiate between polyp types versus ultrasound. It allows the layers of the gallbladder wall to be correctly differentiated, as the loss of this pattern is one of the main signs of malignancy. However, a meta-analysis had statistically compared the results of both techniques, and no significant differences were observed between them.18 No studies have been carried out on the diagnostic accuracy of the preoperative combination of both tests.9
The latest recommendations from the Society of Radiologists in Ultrasound (SRU) establish that, if an intravesicular lesion of >10 mm is observed on ultrasound with no clear signs of malignancy (absence of liver invasion or altered gallbladder structure), the ultrasound should be repeated in 1–2 months using Doppler ultrasound and an optimized gray scale; or CEUS or MRI should be performed for better characterization of the lesion.12
Another topic of discussion in the management of these patients is the frequency of follow-up in patients eligible for conservative management, and until when it should be carried out, since the rate and time at which adenomas can evolve into adenocarcinomas is not clear. In the vast majority of studies, ultrasound follow-up is performed every 6 months during the first 1–2 years and annually thereafter until 5 years of follow-up is completed. Nevertheless, there are studies that conclude that the transformation from adenoma to adenocarcinoma can take up to 10 years, thus supporting longer follow-up in these patients. On the other hand, the review by Wennmacker et al. suggests that ultrasound follow-up of these lesions, especially those of small size, may not be clinically profitable or cost-effective due to the low risk of malignancy reported in the studies included in the analysis. However, the evidence available to date comes from low-quality studies, so more research is required to establish the clinical and economic effectiveness of the ultrasound follow-up of these lesions.9 Thus, the decision to end the follow-up of these patients will depend on the clinical judgment of the doctor responsible.2,5,9
In conclusion, and based on the results of our study, we can affirm that ultrasound is useful for the initial diagnosis of gallbladder polyps. However, it is not very precise, and many diagnosed lesions are not true polyps.
In the future, studies would be necessary to validate and compare the usefulness and precision of CEUS and MRI in the differential diagnosis of gallbladder polypoid lesions in order to avoid unnecessary surgeries, as well as their possible complications.
Conflict of interestsNone.
FundingThis research study has received no specific funding from public, commercial or non-profit entities.
The authors would like to thank the staff of the General Surgery and GI Surgery, Radiology, and Pathology Departments of our hospital.