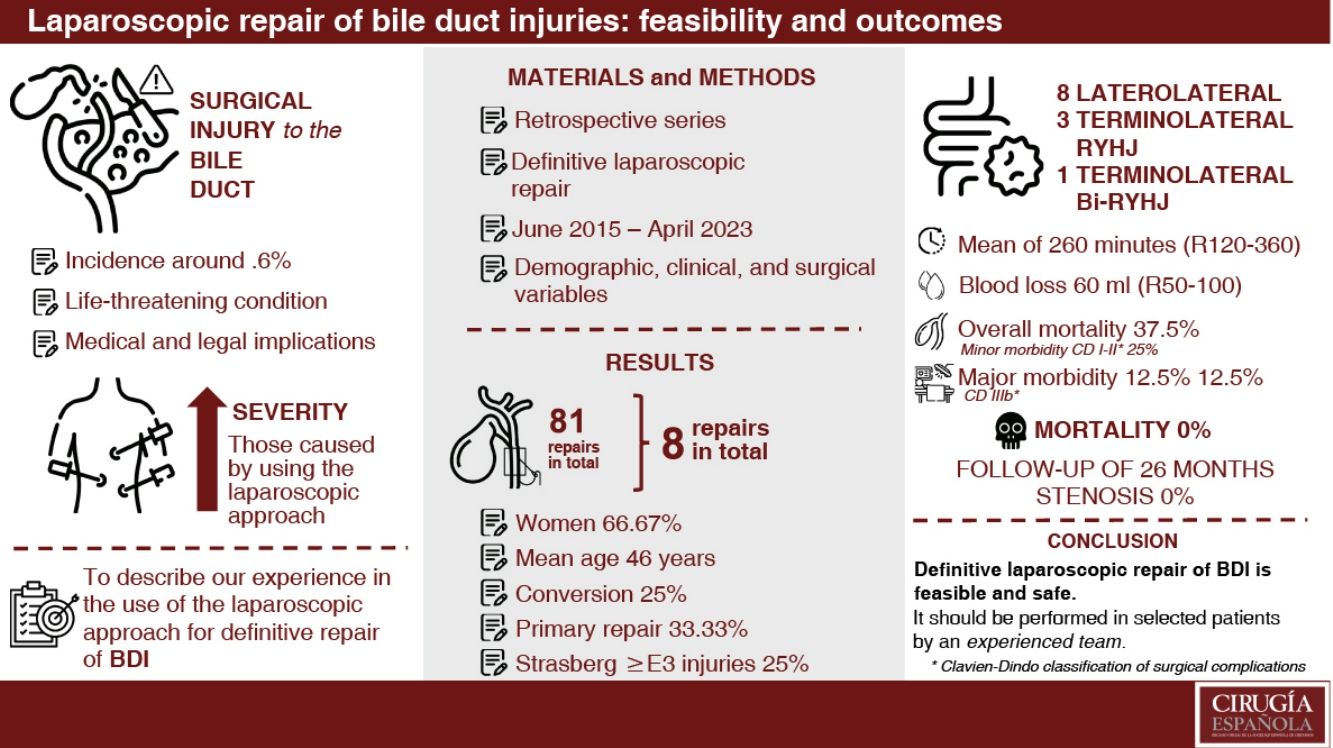
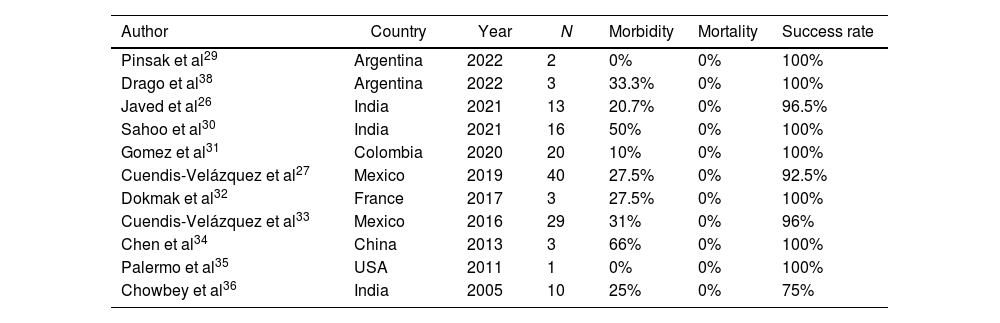
Bile duct injuries (BDI) following laparoscopic cholecystectomy occurs in approximately 0.6% of the cases, often being more severe and complex. Roux-en-Y hepaticojejunostomy (RYHJ) is considered the optimal therapeutic option, with success rates ranging from 75% to 98%. Several series have demonstrated the advancements of the laparoscopic approach for resolving this condition. The objective of this study is to describe our experience in the laparoscopic repair of BDI.
MethodsA retrospective, descriptive study was conducted, including patients who underwent laparoscopic repair after BDI. Demographic, clinical, surgical, and postoperative variables were analysed using descriptive statistical analyses.
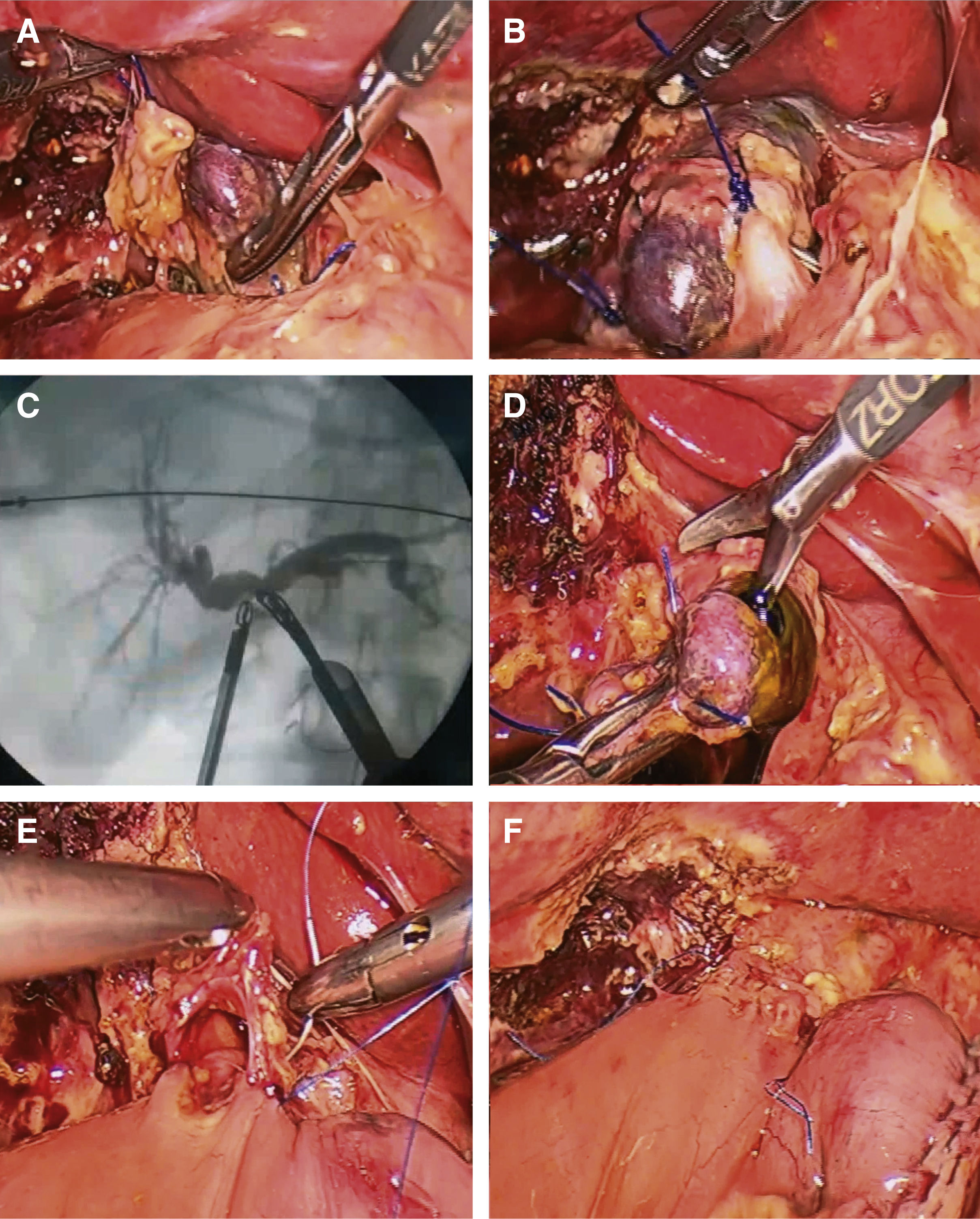
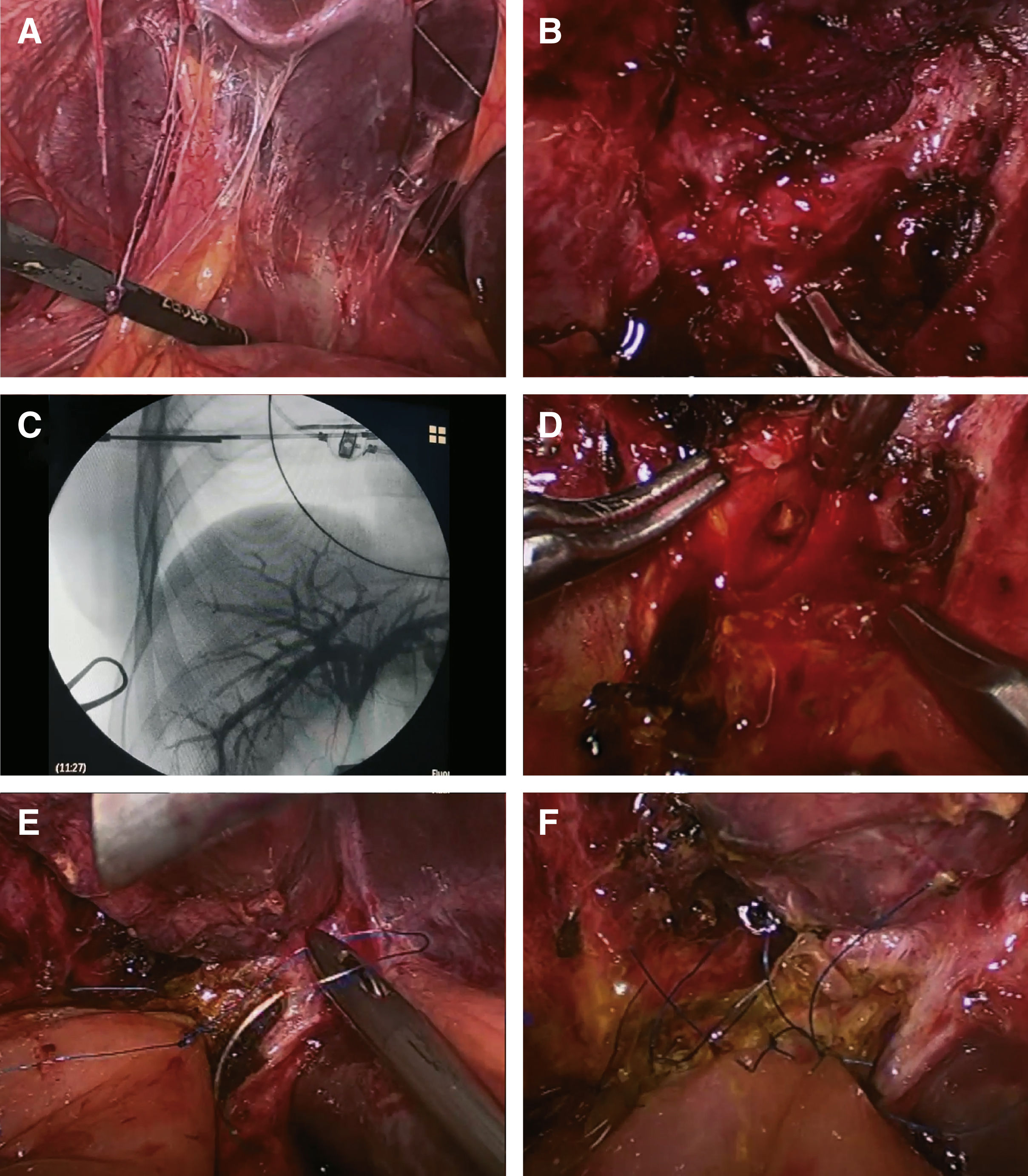
ResultsEight patients with BDI underwent laparoscopic repair (out of 81 surgically repaired patients). Women comprised 75% of the sample. A complete laparoscopic repair was achieved in 75% (6) of cases. The mean age was 40.8 ± 16.61 years (range 19−65). Injuries at or above the confluence (Strasberg-Bismuth ≥ E3) occurred in 25% of cases (2). Primary repair was performed in two cases. Half of the cases underwent a Hepp-Couinaud laterolateral RYHJ, while three patients received a terminolateral RYHJ, and one underwent a bi-terminolateral RYH. The mean operative time was 260 min (range 120−360). Overall morbidity was 37.5% (3 cases): two minor complications (bile leak grade A and drainage-related bleeding) and one major complication (bile leak grade C). No mortality was recorded. The maximum follow-up period reached 26 months (range 6–26).
ConclusionsOur study demonstrates the feasibility of laparoscopic RYHJ in a selected group of patients, offering the benefits of a minimally invasive approach.
Las lesiones quirúrgicas de la vía biliar (LQVB) posteriores a la colecistectomía videolaparoscópica tienen una incidencia del 0,6% aproximadamente, siendo generalmente más graves y complejas. La hepaticoyeyunoanastomosis en Y de Roux (HYA) es la mejor opción terapéutica (tasas de éxito entre 75–98%). Algunas series demostraron factible el abordaje laparoscópico en la resolución de esta patología. El objetivo es describir nuestra experiencia en la reparación laparoscópica de las LQVB.
MétodosEstudio retrospectivo, descriptivo. Se incluyeron pacientes sometidos a reparación laparoscópica posterior a LQVB. Se analizaron variables demográficas, clínicas, quirúrgicas y postoperatorias. Se aplicaron análisis estadísticos descriptivos.
ResultadosSe evaluaron 92 pacientes con LQVB; 81 se sometieron a reparación quirúrgica, ocho fueron candidatos a HYA laparoscópica (aplicabilidad 9,88%). En el 75% (6) se logró una reparación laparoscópica completa. La mayoría eran mujeres (75%). Edad promedio de 40,8 ± 16,61 años (rango 19−65). Las lesiones Strasberg-Bismuth ≥ E3 afectaron al 25% (2). En la mitad se realizó una HYA laterolateral según la técnica de Hepp-Couinaud; tres pacientes recibieron una HYA terminolateral y otro una bi-HYA terminolateral en Y de Roux. Tiempo operatorio promedio de 260 minutos (rango 120−360). La morbilidad global fue del 37,5% (3 casos): dos complicaciones menores (bilirragia grado A y hemorragia por drenajes) y una mayor (bilirragia grado C). No se registró mortalidad. El seguimiento máximo fue de 26 meses (rango 6–26).
ConclusionesNuestro estudio muestra que en un grupo seleccionado de pacientes, la HYA laparoscópica es factible, con los beneficios de un abordaje miniinvasivo.