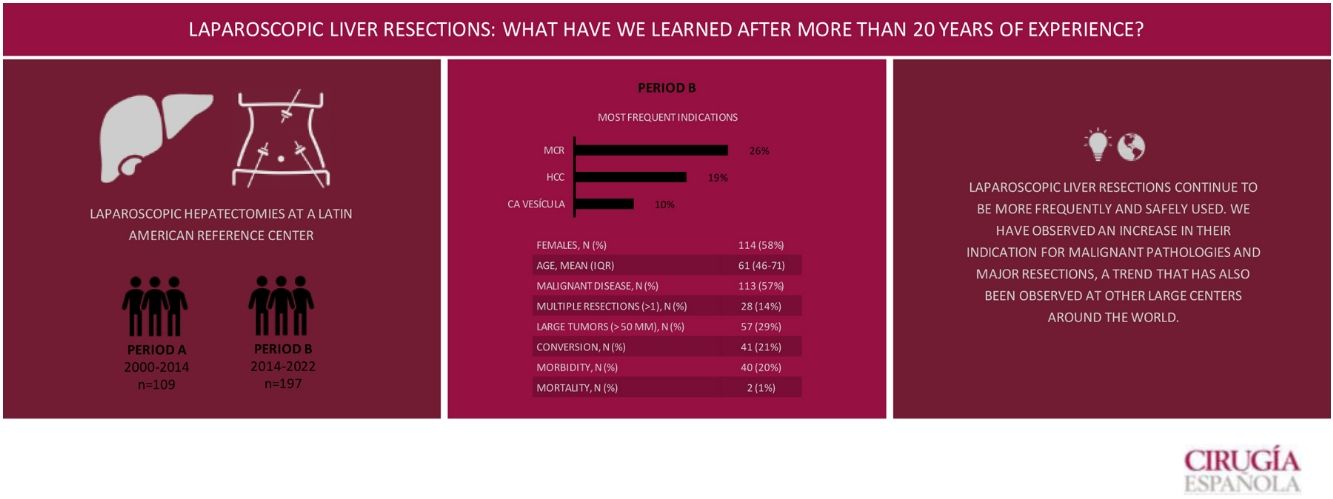
The aim of this study is to describe our experience in the last 8 years of laparoscopic liver resections (LLR) for benign and malignant tumors, to evaluate indications and results, and to compare the results with our previous experience and with other reference centers worldwide.
MethodsBased on a prospective database of the Hepatopancreatobiliary Surgery and Liver Transplantation Unit of the Hospital Italiano de Buenos Aires, patients who underwent LLR between September 2014 and June 2022 were retrospectively analyzed (period B) and where compared to our own experience from 2000 to 2014 previously published (period A).
ResultsColorectal liver metastasis was the main indication for surgery (26.4%). Major hepatectomies accounted for 15.7% of resections and the most frequently performed procedure was typical and atypical hepatectomies (58.4%) followed by left lateral hepatectomy (20.3%). The total postoperative major complications rate was 10.1% and the 90-day postoperative mortality was 1%. The median postoperative stay was four (IQR: 3–6) days. The overall survival rate estimated at 1, 3 and 5 years was 94%, 84% and 70%, respectively, with a median follow-up of 22.9 months.
ConclusionsLLRs in the hands of trained surgeons continue to grow safely, and we have seen an increase in the indication of LLR for malignant pathologies and major resections, a trend that follows the rest of the major centers in the world and has become the method of choice for surgical treatment of most liver tumors.
El objetivo de este estudio es describir nuestra experiencia en los últimos 8 años de resecciones hepáticas laparoscópicas (RHL) por tumores benignos y malignos, para evaluar indicaciones y resultados, y comparar los resultados con nuestra experiencia previa y con otros centros de referencia a nivel mundial.
MétodosA partir de una base de datos prospectiva de la Unidad de Cirugía Hepatopancreatobiliar y Trasplante Hepático del Hospital Italiano de Buenos Aires se analizaron de forma retrospectiva los pacientes que fueron sometidos a RHL entre septiembre de 2014 y junio de 2022 (período B) y se compararon los resultados con nuestra propia experiencia de RHL realizadas entre los años 2000 y 2014, publicada previamente (período A).
ResultadosLa indicación quirúrgica más frecuente fue por metástasis de cáncer colorrectal (26,4%). El 15,7% de las resecciones fueron hepatectomías mayores y el procedimiento más frecuentemente realizado fueron hepatectomías típicas y atípicas (58,4%), seguido por la hepatectomía lateral izquierda (20,3%). La tasa de complicaciones mayores fue del 10,1%. La mortalidad en los primeros 90 días postoperatorios fue del 1%. La mediana de estancia postoperatoria fue de 4 (IQR: 3−6) días. La sobrevida global al año, a los 3 y a los 5 años fue del 94%, del 84% y del 70%, respectivamente, con una media de seguimiento de 22,9 meses.
ConclusionesLas resecciones hepáticas por vía laparoscópica en manos de cirujanos entrenados continúan creciendo de manera segura, y hemos visto un aumento en la indicación de RHL para patologías malignas y resecciones mayores, tendencia que acompaña al resto de los grandes centros del mundo y se ha convertido en el método de elección para el tratamiento quirúrgico de la mayoría de los tumores hepáticos.
Over the last 30 years, laparoscopic surgery has evolved to become the approach of choice for multiple abdominal procedures, which has significantly changed surgical practice.
In the early 1990s, the first laparoscopic liver resections (LLR) were reported1,2. Since then, minimally invasive liver surgery (MILS) has evolved, and today both simple and complex procedures are equally safe and feasible to perform, including major hepatectomies and liver ablations from living donors3–5.
To date, consensus conferences have taken place, and international guidelines for MILS have been developed. At these conferences, leading experts have determined the optimal conditions and indications for performing LLR and provided recommendations to perform and implement these procedures6–8.
Today, the field of LLR has become a reality that continues to evolve and requires periodic reassessment. In 2007, we presented our initial experience with laparoscopic liver resections9. In 2015, we re-analyzed our results after 14 years of experience in MILS10. Thus, the objective of this study is to describe our experience over the last 8 years with LLR due to benign and malignant tumors, evaluate the indications and results, and compare the results with our previous experience as well as other reference centers around the world.
MethodsFrom a prospective database of the Hepatopancreatobiliary Surgery and Liver Transplantation Unit of the Hospital Italiano de Buenos Aires, we retrospectively analyzed patients who underwent LLR between September 2014 and June 2022 (Period B) and then compared the results with our own experience of LLR carried out between 2000 and 2014 (previously published10) (Period A). The study criteria excluded patients who underwent liver biopsies, unroofing of liver cysts, and radiofrequency ablations.
Statistical analysisWe evaluated patient age, sex and demographic variables, reason for consultation, indication for resection, pre- and postoperative diagnosis, number of lesions as well as their size and location, procedure performed, pedicle clamping, operative time, associated procedures, conversion rate, hospitalization time, morbidity and mortality, and results of distant disease in malignant pathology. Postoperative complications were recorded according to the Dindo–Clavien classification11. Operative mortality was defined as death occurring during hospital stay or within 90 days of surgery.
ResultsA total of 197 patients were included in period B, in whom laparoscopy was applicable in 49.5%. The sex of the population was predominantly female (57.9%), with a median age of 61 years (IQR 46−71). Resections had been conducted by specialist surgeons from the Hepatobiliopancreatic Surgery service in 99.1% of the cases. The most frequent reasons for consultation were oncological follow-up or incidental findings on imaging studies (32.5% and 30.9%, respectively). The remaining demographic and clinical characteristics are presented in Table 1.
Demographic and clinical characteristics.
| Female sex, n (%) | 114 (58%) |
| Age, mean (IQR) | 61 (46−71) |
| Weight in kg, mean (IQR) | 74 (60−85) |
| Height in meters, mean (IQR) | 1.65 (1.58−1.63) |
| BMI, mean (IQR) | 26.1 (22.9−29.7) |
| ASA, mean (IQR) | 2 (2−3) |
| Malignant disease, n (%) | 113 (57%) |
| Multiple resections (>1), n (%) | 28 (14%) |
| Simultaneous resections, n (%) | 41 (21%) |
| Large tumors (>50 mm), n | 57 (29%) |
| Hospital stay in days, mean (IQR) | 4 (3−6) |
The most frequent indication was colorectal tumor metastasis (CRM) in 26.4% of cases, followed by hepatocellular carcinoma (HCC) in 19.3% and gallbladder cancer (GC) in 10.1% (Fig. 1). In 28 patients (14.2%), the resections were multiple (2–6); in the remaining 169 (85.8%) patients, the resections were solitary. In total, 15.7% of the resections were major hepatectomies (3 or more continuous segments), and the most frequently performed procedures were typical and atypical hepatectomies in 115 patients (58.4%), followed by left lateral hepatectomy in 40 cases (20.3%). The rest of the procedures are analyzed in Table 2.
Types of resections.
| Resection | Type | n = 197 |
|---|---|---|
| Major | Right hepatectomy | 12 (6%) |
| Left hepatectomy | 16 (8%) | |
| Right trisectionectomy | 3 (2%) | |
| Minor | Typical and atypical segmentectomy | 105 (53%) |
| Bisegmentectomy IVb-V | 10 (5%) | |
| Left medial hepatectomy | 1 (1%) | |
| Left lateral hepatectomy | 40 (20%) | |
| Right anterior hepatectomy | 2 (1%) | |
| Right posterior hepatectomy | 8 (4%) |
Mean operative time was 198 min (IQR 140–292). The total postoperative complication rate was 20.3%, and the major complication rate (Dindo–Clavien > IIIb) was 10.1%. Table 3 compares the characteristics of patients who presented major complications versus those who did not. A total of 41 (20.8%) patients underwent conversion to laparotomy, and in 15 cases (7.6%) the procedure was hand-assisted. The mortality rate in the first 90 postoperative days was 1%.
Characteristics of patients with major complications.
| With a major complication (n = 20) | No major complication (n = 177) | OR (95%CI) | P | |
|---|---|---|---|---|
| Age, mean (IQR) | 64.5 (45.5−69.0) | 60.0 (46.0−71.0) | 1.00 (0.97−1,03) | 0.794 |
| BMI, mean (IQR) | 25.7 (23.0−29.0) | 26.1 (22.9−29.8) | 1.01 (0.93−1.10) | 0.703 |
| Female sex, n (%) | 10.0 (50.0) | 104.0 (58.7) | 0.55 (0.27−1.10) | 0.095 |
| History of abdominal surgery, n (%) | 11.0 (55.0) | 115.0 (65.3) | 0.64 (0.25−1.65) | 0.363 |
| Surgical time, min (IQR) | 235.0 (150.0−306.0) | 198.0 (140.0−228.0) | 1.00 (0.99−1.00) | 0.218 |
| Major resection, n (%) | 5.0 (25.0) | 32.0 (18.0) | 1.51 (0.511−4.45) | 0.455 |
| Tumor diameter, cm (IQR) | 5.0 (1.1−6.5) | 3.2 (1.7−5.0) | 1.05 (0.89−1.24) | 0.511 |
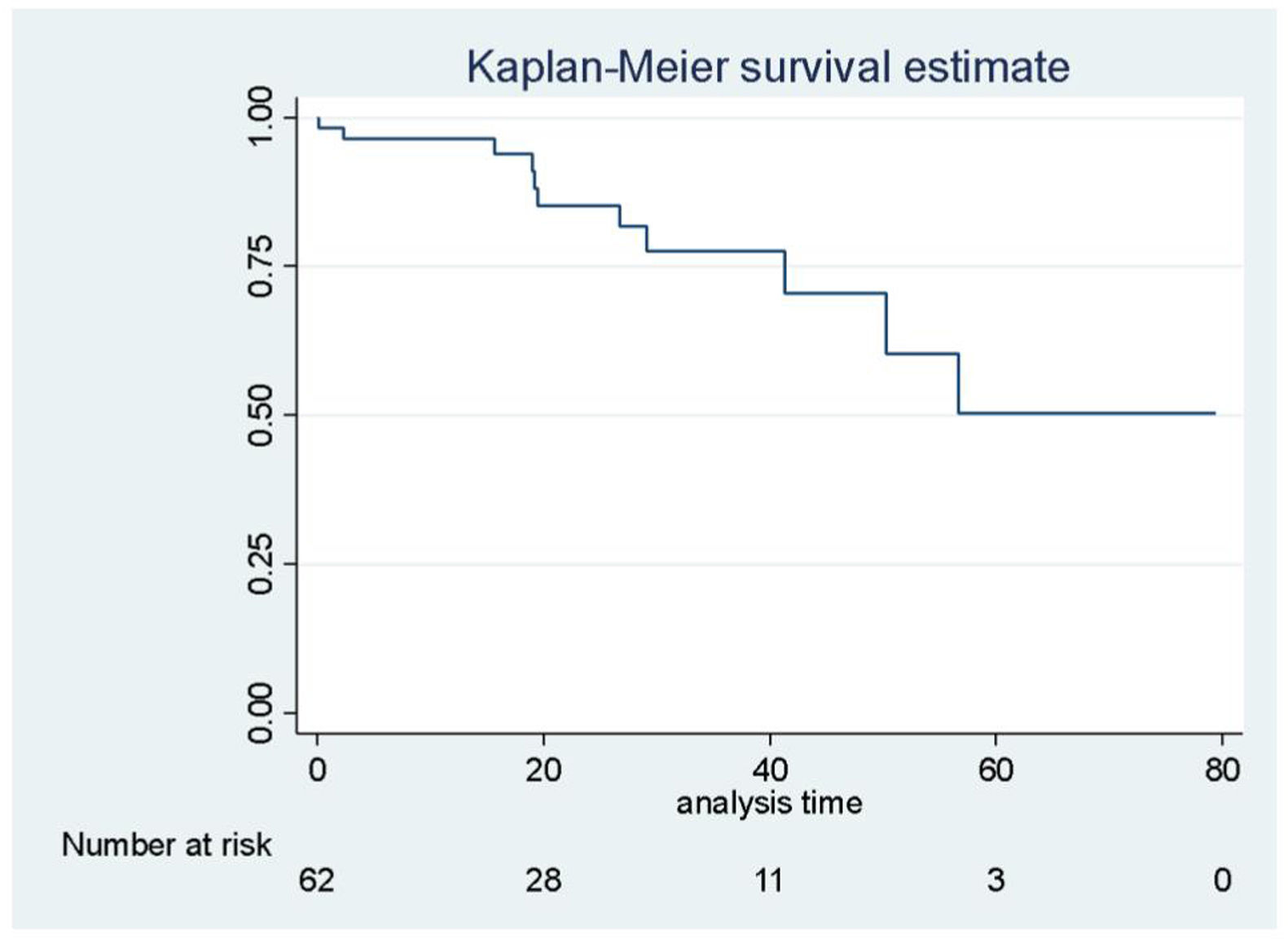
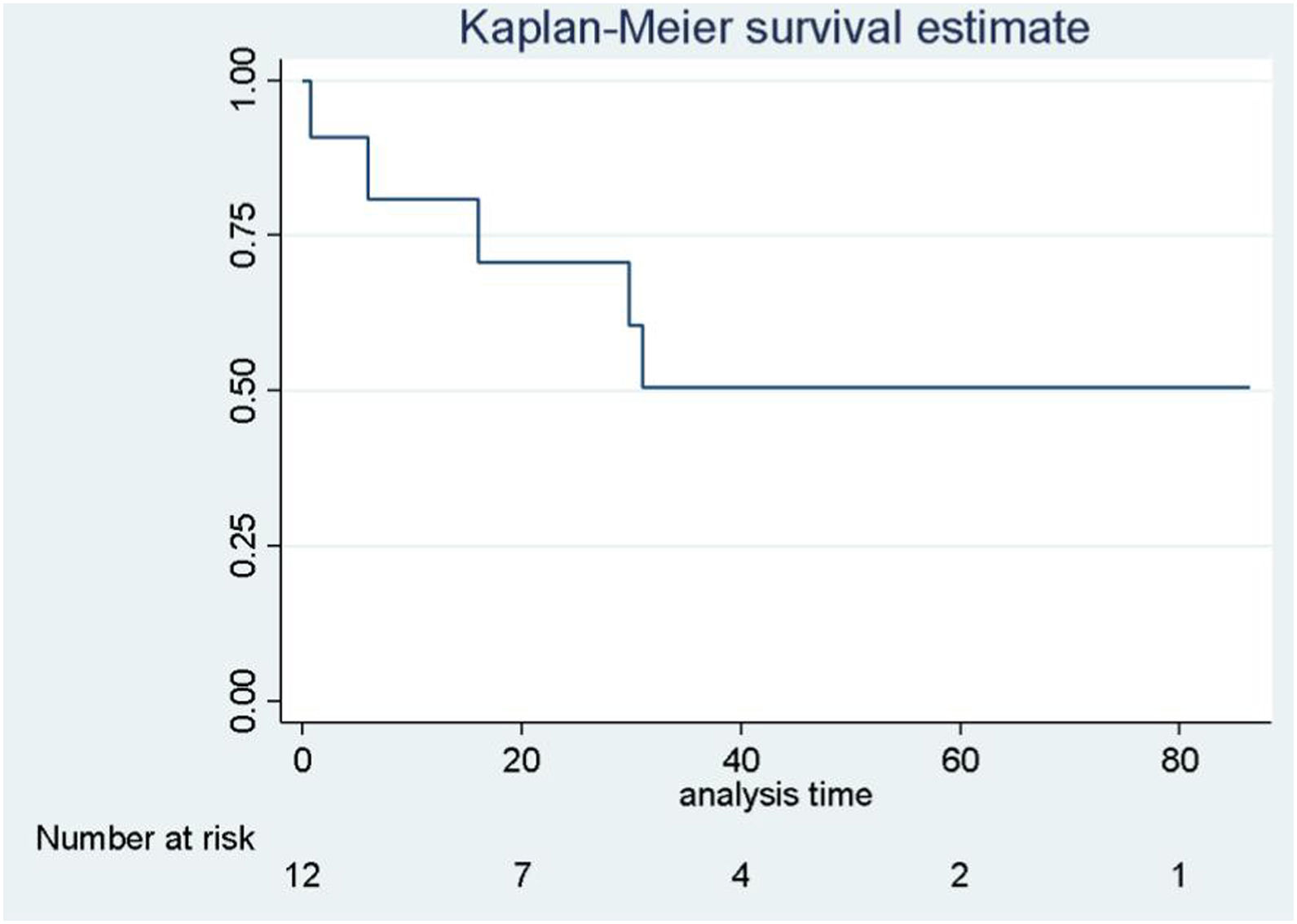
The median postoperative hospital stay was 4 (IQR 3−6) days. The overall survival rates for malignant pathology after one, 3 and 5 years were 98%, 98% and 90% (CI: 0.89−0.99; CI: 0.89−0.99; and CI: 0.60−0.98), respectively, with a mean follow-up of 22.9 months (Fig. 2). Regarding the most frequent pathology, the overall survival rates for metastasectomies after one, 3 and 5 years was 96%, 77% and 50% (CI: 0.86−0.99; CI: 0.58−0.88; CI: 0.22−0.73) (Fig. 3); survival rates after hepatocellular carcinoma also after one, 3 and 5 years was 88%, 73% and 73% (CI: 0.66–0.95; CI: 0.34–0.91; CI: 0.34–0.919 (Fig. 4).
In recent years, LLR have experienced exponential growth in Argentina and the rest of the world since the controversy about the oncological and perioperative safety of minimally invasive surgery has been resolved, widely demonstrated and published12. In addition, the expert consensus has expanded the indications from minor resections in anterior segments to major hepatectomies as well as complex lesions in the posterior segments, or with vascular reconstructions and even ALPPS (associating liver partition and portal vein ligation for staged hepatectomy) via laparoscopic surgery and hepatectomies for living-donor liver transplantation (first case in our hospital in 2019)8,13,14. The contraindications are the same as for laparoscopic surgery and are usually associated with the risks related to anesthesia, such as severe cardiopulmonary pathology, hypertension ascites and relative contraindications, such as multiple previous surgeries, pregnancy and intestinal occlusion15. The development of the team’s technical skills has meant that contraindications are relative. Currently, and given our level of experience, a close relationship between the tumor and the venous axes of the suprahepatic cava axis means that the conventional approach is preferred in such cases.
In fact, few hospitals have extensive experience in LLR16. A survey of 27 international expert hepatobiliary surgery centers from around the world showed different numbers depending on the region: the LLR rates were 34.6% in Asia-Pacific, 35.6% in Europe and 27.4% in North/South America17,18. Table 4 shows the results obtained in our study periods and compares them with international reference series19–21.
Comparison of time periods and other international series.
| Period A | Period B | Total series | USA | Europe | Asia | |
|---|---|---|---|---|---|---|
| Period | 2000–2014 | 2014–2022 | 2000–2022 | 2006–2020 | 1998−2018 | 2006−2020 |
| N of cases, n | 109 | 197 | 306 | 500 | 1232 | 382 |
| Female sex (%) | 67% | 58% | 61% | 53% | 47% | 36% |
| Age, mean | 55 | 61 | 57 | 59 | 66 | 71 |
| Most frequent indication | CRM | CRM | CRM | HCC | CRM | HCC |
| Benign pathology, n (%) | 57 (52%) | 84 (43%) | 141 (46%) | 180 (36%) | 122 (10%) | 16 (4%) |
| Malignant pathology, n (%) | 52 (48%) | 113 (57%) | 165 (54%) | 320 (64%) | 1110 (90%) | 366 (96%) |
| Resections <, n (%) | 96 (89%) | 160 (81%) | 256 (84%) | 367 (73%) | 699 (57%) | 330 (86%) |
| Resections >, n (%) | 13 (11%) | 37 (19%) | 50 (16%) | 133 (27%) | 533 (43%) | 52 (14%) |
| Conversion, n (%) | 9 (9%) | 41 (21%) | 50 (16%) | 71 (14%) | 39 (3%) | 26 (7%) |
| Morbidity, n (%) | 11 (11%) | 40 (20%) | 51 (17%) | 68 (14%) | 246 (20%) | 32 (8%) |
| Complications <, n (%) | 7 (7%) | 20 (10%) | 27 (9%) | 55 (11%) | 119 (10%) | 23 (6%) |
| Complications >, n (%) | 4 (4%) | 20 (10%) | 24 (8%) | 13 (3%) | 127 (10%) | 9 (2%) |
| Mortality, n (%) | 1 (1%) | 2 (1%) | 3 (1%) | 1 (0.2%) | 4 (0.3%) | 0 (0%) |
When we compared the results analyzed (Period B) with our own experience at the beginning of the program (2000–2014, Period A)9, we observed that the most frequent indication for LLR continued to be CRM, similar to reports by large European series21,22. Hepatocellular carcinoma and gallbladder cancer are in second and third place in Period B, showing an increase in the indication for laparoscopic resection; this trend has also been reported by study centers in North America and Asia, where they have surpassed CRM19,20. Also, although the sample size does not allow for in-depth analysis of the different pathologies, in the cases of gallbladder cancer this was carried out descriptively (Fig. 5) since the treatment and prognosis vary greatly depending on the stage. It is worth mentioning that in our cohort, which represents 10.1% (n = 20) of the indication for LLR, 70% of the cases were diagnosed due to incidental findings in post-cholecystectomy pathology. In 5 instances, the diagnosis was preoperative due to non-specific abdominal pain, and one patient was diagnosed with prostate cancer during follow-up oncological studies. Right trisegmentectomy was performed in only one case (T4N0Mx), and in the remaining 19 cases we enlarged the gallbladder bed, froze the cystic duct, and emptied the hepatic pedicle. The pathology study was compatible with the absence of atypia in most cases, which is consistent with the fact that we, like Chile, are in an area with a regional incidence of gallbladder cancer, where radical second-stage surgery is completed laparoscopically.
In our experience, the number of major LLR increased from 11% to 18.8% (Table 4), which resulted in an increase in overall morbidity but no increase in major complications (D–C > IIIB), reoperations (which remained low at 4.1%), or mortality (which continued to be less than 1%). The conversion rate of Period B reached 20%, a number that exceeds most reported series19,21,22. We believe this may be due to multiple factors that merit further study, such as patient comorbidity, larger resection size, greater complexity of the procedures, and unexpected intraoperative findings.
Over the last two decades, the indications for surgery, patient complexity and procedural complexity have expanded significantly. In the hands of trained surgeons, the use of laparoscopic liver resections continues to grow safely, and we have observed an increase in the indication of LLR for malignant pathologies and major resections. This trend has also been noted in other large medical centers around the world as LLR becomes the method of choice for surgical treatment of most liver tumors.
FundingThis research study has received no specific funding from public, commercial or non-profit entities.
Conflicts of interestsNone to declare.
The authors would like to thank Dr Sebastián Marciano for his guidance and contributions to the methodology.