Recurrent primary hyperparathyroidism (HPTP-R) is defined as elevated serum calcium and parathyroid hormone (PTH) levels after parathyroidectomy, with normalization of these parameters for at least 6 months. It differs from persistent primary hyperparathyroidism (HPTP-P), in that in the latter, postoperative hypercalcemia is not resolved in this period.1 Despite advances in preoperative imaging tests and surgical management, persistence/recurrence of this disease still occurs in 2.5%–5.5% of sporadic HPTP.2,3
The main causes of HPTP-P are the absence of identification of the adenoma and undiagnosed or insufficiently treated multiglandular disease.4 The causes of HPTP-R include recurrence of a parathyroid carcinoma, recurrence of the remnant, or metachronous hyperplasia in the context of familial hyperparathyroidism, or supernumerary glands.5
There are few publications in the literature about local recurrence of parathyroid adenomas, so we believe it is interesting to analyze our experience with this type of reoperations.
We conducted a retrospective study of reoperations for HPTP-P or HPTP-R from 1997 to 2019 in a reference Endocrine Surgery Unit. We defined HPTP-R as elevated serum calcium and PTH levels 6 months after a successful initial parathyroidectomy.
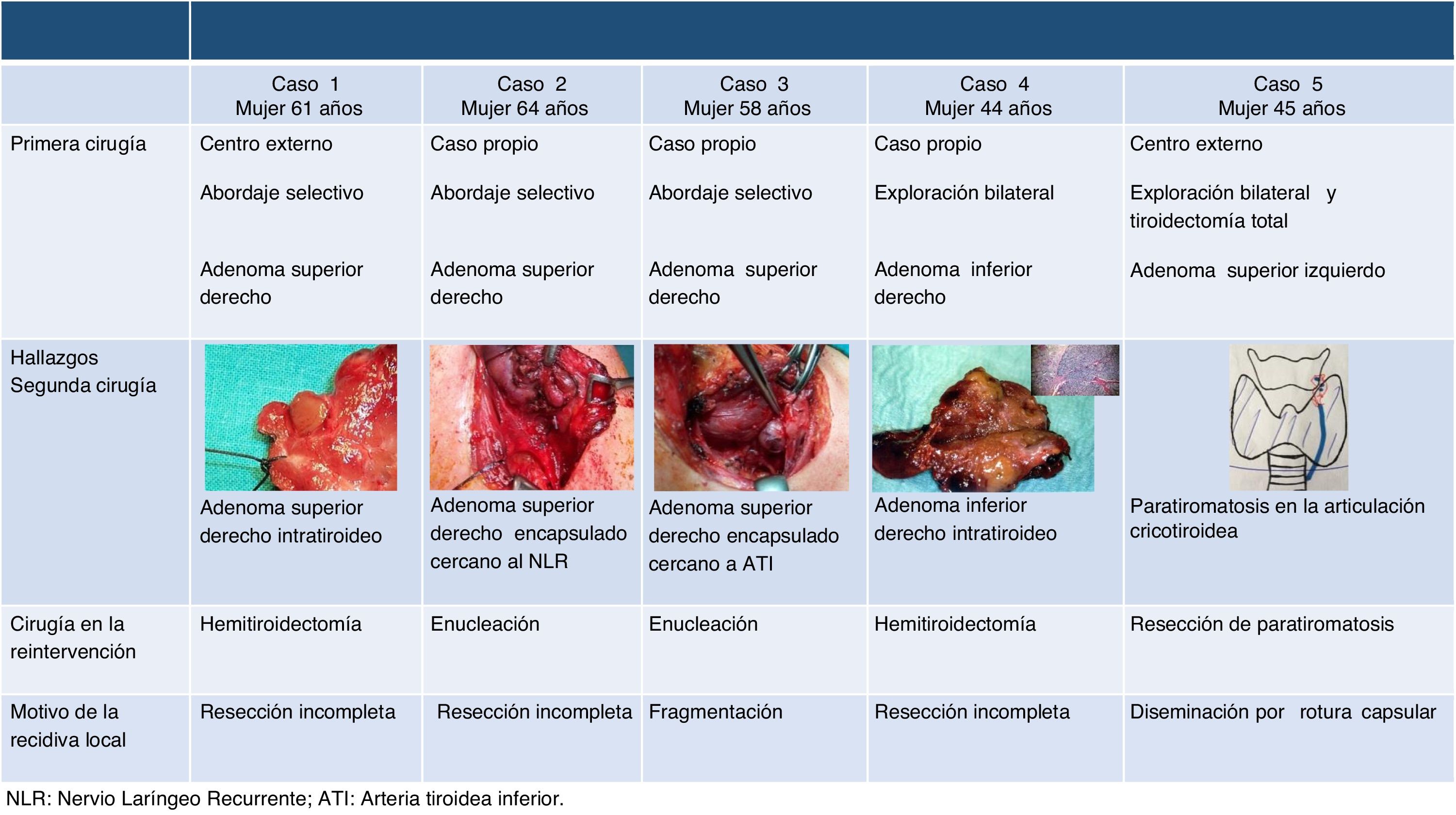
Patients with recurrence in the same location as the previously removed adenoma were identified, and those with hereditary hyperparathyroidism and carcinomas were excluded. We conducted a descriptive analysis of demographic variables, imaging tests prior to initial surgery and reoperation, the surgical technique used for both procedures, the time interval between them, and postoperative complications.
Seventy reoperations were performed, 33 of which had initially unidentified adenomas (47.1%), 18 multiglandular disease correctly/incorrectly treated in the first surgery (25.7%), 14 double adenomas (20%) and 5 local recurrence (7.1%).
The 5 local recurrences were women with a mean age of 53 ± 8 years who underwent resective surgery for a histologically confirmed sporadic adenoma and had maintained postoperative normocalcemia. The mean interval between both interventions was 10.6 ± 7 years. Previously, a bilateral cervical exploration had been performed in two patients, while a selective approach was used in three. Reoperations consisted of two hemithyroidectomies for intrathyroid adenomas, two enucleations, and one atypical resection for paratiromatosis/parathyroid disease; in all cases, parathyroid tissue with no malignancy criteria was confirmed in the histology study. Incomplete resection (4 cases) and local seeding due to probable capsular rupture were identified as the causes of local recurrence (Fig. 1).
Intraoperative PTH (PTHio) was determined in the three most recent reoperations, meeting the Miami criteria. One patient presented transient recurrent paralysis after a loss of segmental signal during neuromonitoring due to adhesion of the adenoma to the RLN/NLR. None of the cases presented postoperative hypocalcemia. After reoperation, all the patients remained asymptomatic and had normocalcemia during follow-up.
Local recurrence of a parathyroid adenoma after successful parathyroidectomy is rare. The classic study by Fraker et al.6 reported 11 benign local recurrences among 108 reoperated patients, 4 for HPTP-P and 7 for HPTP-R. In our study, the prevalence was similar, with only 7.1% of reoperations due to a locally recurrent adenoma, all of them due to HPTP-R. Other authors report a higher prevalence, such as the 17.4% of the pioneering publication by Rattner et al.7
Causal mechanisms for local recurrence that have been described include parathyromatosis/Parathyroid disease due to violation of the parathyroid capsule, or incomplete excision leaving a portion in situ, as in partially intrathyroid adenomas, secondary to cell implantation after capsular disruption or hyperplasia of residual tissue hyperplasia.6,7 In this sense, and given our findings, a hemithyroidectomy could be considered. On the other hand, local recurrence is a hallmark of parathyroid carcinoma, so a high index of suspicion must be maintained intraoperatively and local invasion or metastatic nodes must be ruled out histologically.
The mean interval between initial surgery and reoperation was greater than 10 years, which is consistent with previous publications7 with a range between 8 and 23 years. Therefore, in a late recurrence after initial successful surgery, we must consider a benign local recurrence.
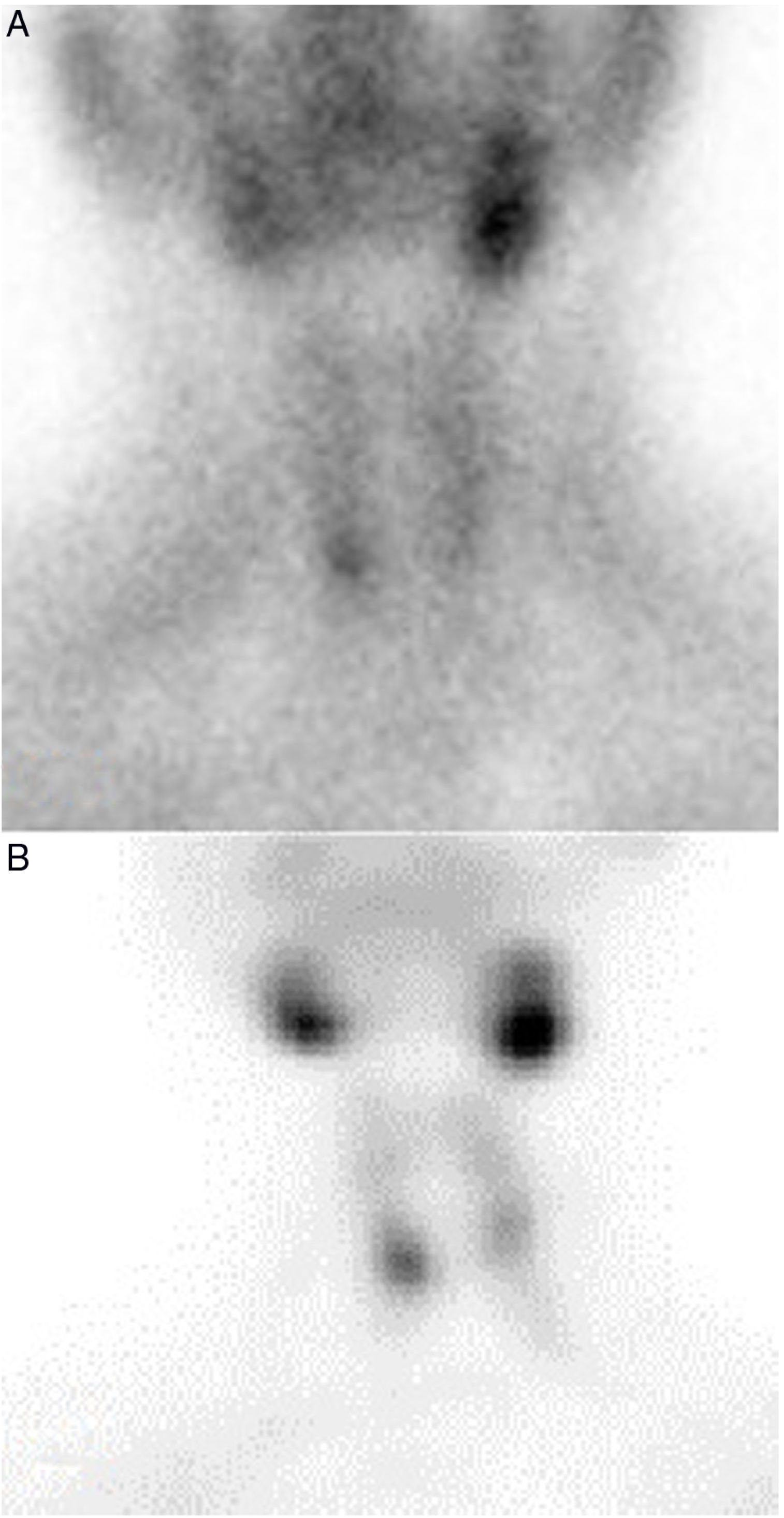
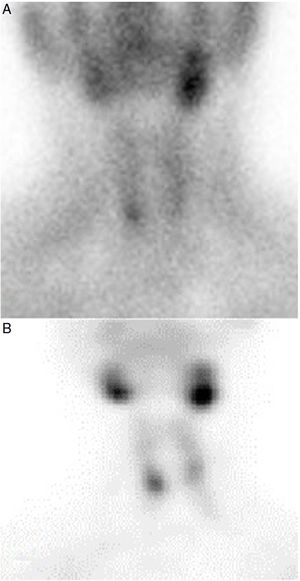
In the present study, the preoperative scintigraphies showed identical images between the initial surgery and the reoperation (Fig. 2).
This coincidence, not previously described, would allow us to suspect local recurrence and could have implications for planning and surgical approach. In our hospital, the lateral approach was chosen, which makes it possible to perform a hemithyroidectomy for partially/totally intrathyroid adenomas in which enucleation may not be effective. In the publication by Ros et al8 of 16 intrathyroid parathyroid adenomas, two local recurrences were found in the three patients treated with enucleation.
The determination of PTHio could be especially important in reoperations.1,9 Irvin et al10 compared patients with and without PTHio monitoring, observing an increase in the success rate of reintervention from 76% to 94%, respectively.
Although the morbidity derived from parathyroid reexaminations has decreased in recent decades,9 there is an increased risk of postoperative recurrent paralysis and hypocalcemia.1 Intraoperative neuromonitoring is especially useful in relapses of the upper gland, closely related to the terminal segment of the NLR/RLN, where it tends to branch and is more vulnerable.
As conclusions, local recurrence after parathyroidectomy due to benign non-familial primary hyperparathyroidism is a rare cause of recurrence and it should be suspected if the recurrence is late, the preoperative imaging tests in both surgeries coincide and a capsular rupture or partially intrathyroid adenoma is described in the first surgery. Hemithyroidectomy should be considered for partially/totally intrathyroid adenomas in the initial surgery and at reoperation. Reoperation for primary hyperparathyroidism is challenging and should be carried out by experienced surgeons at high-volume hospitals.
Please cite this article as: Martínez Sanz N, Lorente Poch L, Torselli Valladares ED, Sancho Insenser JJ, Sitges Serra A. Recidiva local de adenomas de paratiroides como causa infrecuente de hiperparatiroidismo primario recurrente. Cir Esp. 2021;99:161–164.