Colonic diverticulosis is a common entity that causes an acute inflammatory process in approximately 20% of patients.1 About 20% of patients who undergo elective surgery for complications of diverticulosis present fistula of the colon with another organ; colovesical fistulae are the most frequent, and colouterine fistulae are among the most unusual.2 Currently, the minimally invasive treatment of diverticular disease includes the use of video-assisted laparoscopic surgery3 and the application of perioperative optimization programs or Enhanced Recovery After Surgery protocols (ERAS).4
We present the case of a 65-year-old woman with a colouterine fistula secondary to complicated diverticular disease, treated by laparoscopic resection of the sigmoid colon and preservation of the uterus within the framework of an ERAS program.5
The patient’s history included laparoscopic surgery for endometriosis 30 years earlier, a recent colonoscopy that only showed diverticula in the sigmoid colon, smoking and obesity (BMI 32 kg/m2). The patient consulted for purulent vaginal discharge, with no other clinical manifestations, two months after receiving medical treatment for the first episode of acute diverticulitis. During colposcopy, pus was observed coming out of the cervix, which was mildly painful upon mobilization.
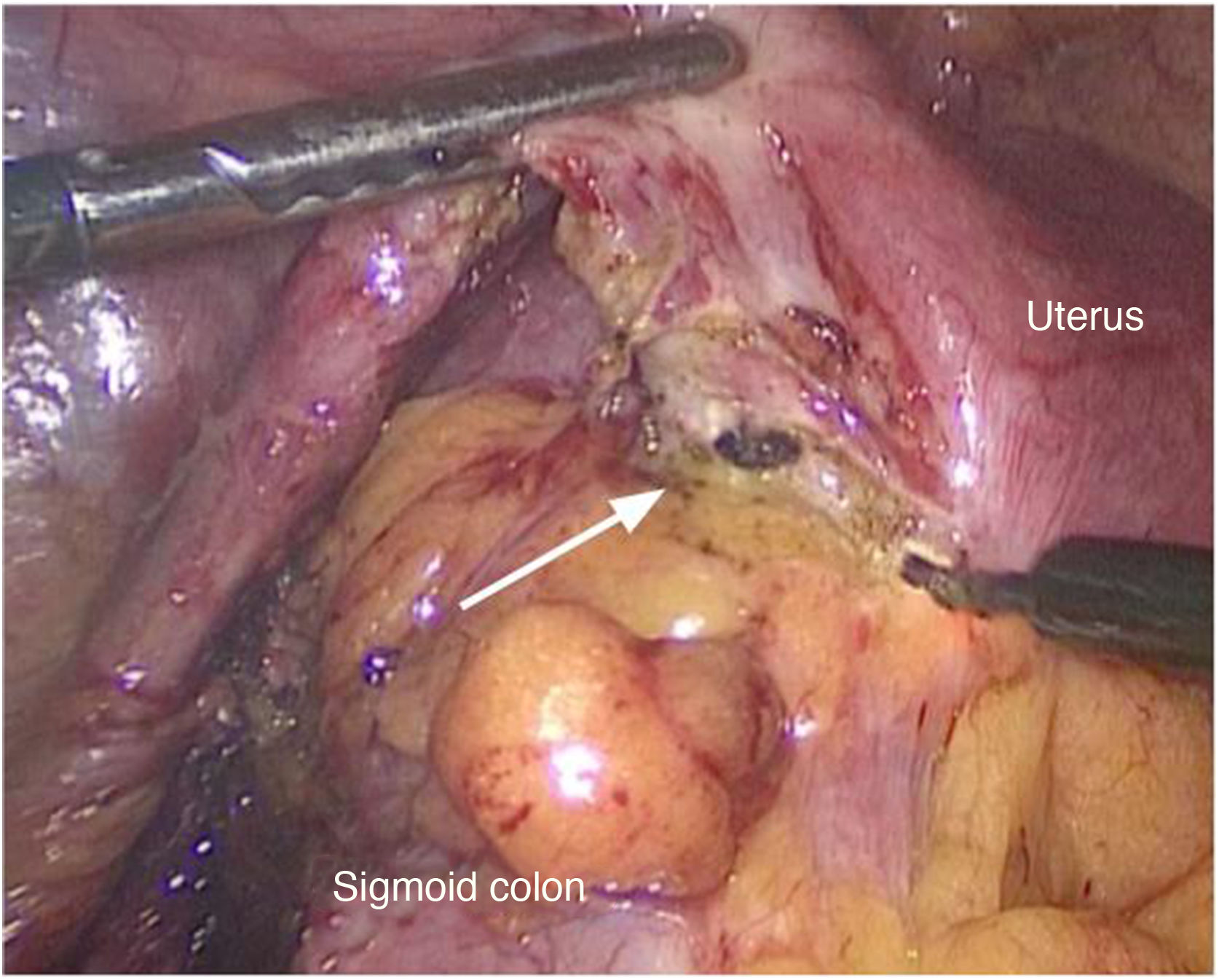
A double contrast barium enema was performed, which showed diverticular formations but no signs of complications. An MRI scan, however, identified a fistula between the sigmoid colon and the uterus with inflammatory characteristics (Fig. 1).
The patient was included in an ERAS program. An enema was used for preoperative bowel preparation, and antibiotic prophylaxis was administered during anesthetic induction. We performed elective exploratory laparoscopy and observed an inflammatory process between the sigmoid colon and the uterus. The colouterine fistula was undone with electrocautery (Fig. 2). Laparoscopic sigmoidectomy was completed, with descent of the splenic angle and primary colorectal anastomosis created with double mechanical suture, following a previously described technique.6 The patient evolved without complications and was discharged from the hospital on the second postoperative day. The histopathological study confirmed diverticular disease of the colon. In the outpatient follow-up visit on the seventh postoperative day, the patient presented no vaginal discharge. After 18 months of follow-up, the patient has had no complications related to the pathology treated.
Colouterine fistula secondary to diverticulitis is a rare entity with few cases reported in the international literature.2 Perhaps this is because the thickness of the myometrium offers great resistance to the subacute inflammatory process that ends up communicating the lumen of the colon with the endometrium. Clinically, it manifests as purulent vaginal discharge due to the presence of fecal matter in the uterus, although it can also manifest as sepsis if there is an accumulation of pus in the uterine cavity. While not recent, the patient’s history of surgery for endometriosis is still important as it could have caused adhesions between the sigmoid colon and the myometrium, favoring the progression of the inflammatory process that began later.
The barium enema did not demonstrate the communication between the two organs, which usually happens.7 Although computed tomography is very sensitive and specific for the diagnosis of acute complications of diverticulosis, identification of a fistulous tract and the diagnostic exclusion of a neoplasm are more difficult. For this reason, we used magnetic resonance imaging, which has greater precision for the diagnosis of a fistula, in addition to allowing us to determine its inflammatory characteristics.8
Surgery is the definitive treatment, and en bloc resection of both organs is the most frequently reported strategy.9 However, there are no clear guidelines on the need for hysterectomy in cases in which there is no pyometra or manifestations of sepsis. Thus, considering that the patient did not present signs of systemic inflammation (fever, leukocytosis, etc.), we opted for a conservative strategy, performing only sigmoidectomy with primary anastomosis. Laparoscopic resection has advantages over open surgery, including less pain, shorter hospital stay and quick recovery.10 Compliance with 83% of the ERAS protocol measures in this particular case contributed to the short hospital stay and low morbidity.
Prophylactic antibiotic treatment was administered during anesthetic induction, similar to what is used for the treatment of colovesical fistulae. It was not continued during the postoperative period due to the optimal clinical condition of the patient, showing no signs of systemic inflammation before or after the procedure, and the lack of evidence for another indication.
This rare entity can be treated appropriately with a minimally invasive approach and without the need for hysterectomy under the clinical conditions presented here, with early hospital discharge.
Please cite this article as: Mentz RE, González Salazar EA, Campana JP, Vaccaro CA, Rossi GL. Tratamiento miniinvasivo de la fístula colouterina de origen diverticular. Cir Esp. 2021;99:549–551.