Internal hernia is responsible of less than 1% of intestinal obstruction. Hernia through the broad ligament is a rare condition reported as less than 7% of all internal hernias.1 During Covid-19 pandemia patients are scared about going to the hospital with an high risk of getting infected and they tend to underestimate the severity of their symptoms. Consequently they arrive to the hospital with a late-stage acute pathology. This state of fact is illustrated by this case report.
The endpoint of the case report is to illustrate a case of a complicated bowel obstruction in which the intestinal resection could have been avoided or minimized if the patient had gone earlier to the emergency.
In the context of the SARS-Cov-2 pandemic, we have detected in emergency services more complicated cases of acute pathologies. We have especially detected cases of periappendicular abscesses and cases of Hinchey 3 and 4 diverticulitis that in our center we usually find in an earlier stade.
The case concerns a 43 years old female with medical history of laparoscopic resection of uterine cyst 15 years ago (no information about the exact position). The patient came to the hospital 24 hours after symptoms starting. She had abdominal pain, nausea and vomiting since the day before. Beacause of the fear of getting the SARS-CoV-2 infection she decided not to come to the hospital despite the symptoms waiting 24 hours.
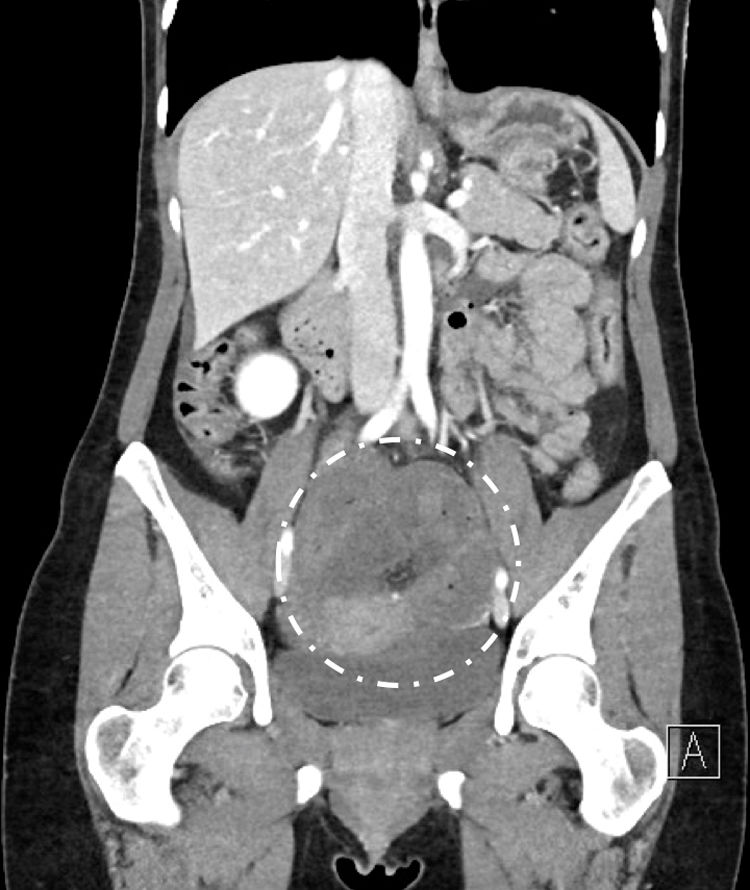
At the emergency admission the patient presented abdominal distension and guarding at low abdominal quadrants. Nausea and vomiting were still present. Blood test showed an inflammatory syndrome with leukocytosis (12460 G/l of white cells), normal C-reactive protein, LDH at 232 U/l and light anemia (10,9 g/dl of haemoglobin). The CT-Scan showed a mechanic intestinal obstruction with dilatation of upstream bowel and signs of intestinal necrosis (Fig.1). The radiological suspicion was an internal strangulated hernia with the transition zone localized in the pelvis. A nasopharyngeal swab and low-dose CT-Scan have been done, in order to follow the Covid-19 screening protocol, and they were negatives.
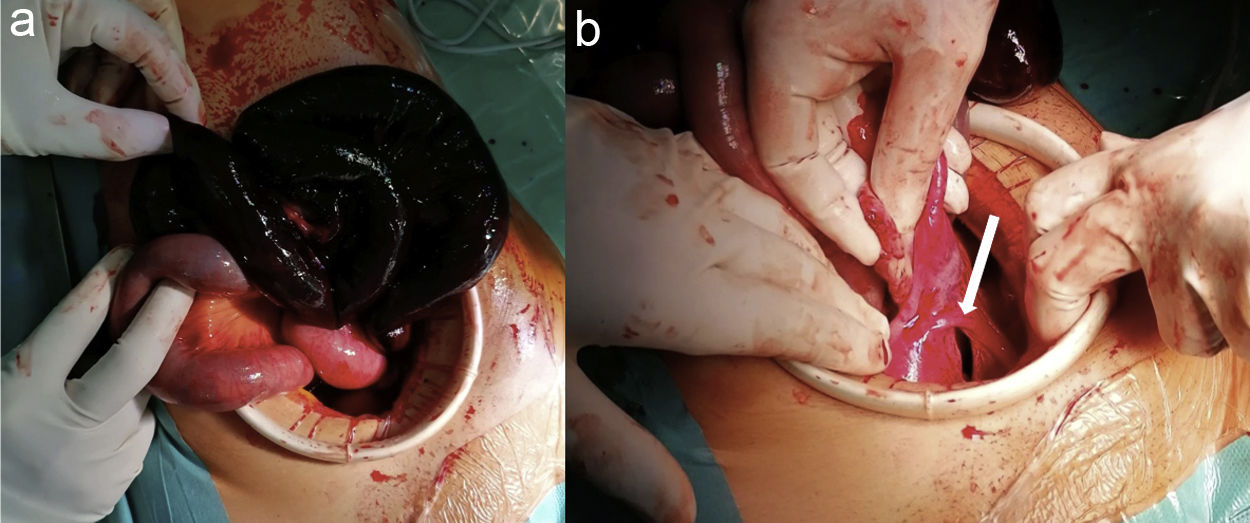
We performed an exploratory laparoscopy founding a 70 cm necrotic ileal loop due to an internal hernia (Fig. 2a). Laparoscopically we localized the defect on the left broad ligament (“fenestra type” according to Hunt classification Fig. 2b).2 The dilatation of upstream bowel and most of all the necrosis of the ileal loop made impossible a laparoscopic manipulation without perforating and contaminating the abdominal cavity. So we decided to convert in laparotomy with a 10 cm sub-umbilical incision. After liberation of the hernia we had to resect the necrotic bowel performing a latero-lateral mechanic anastomosis about 30 cm to Bauhin valve. The 3 cm broad ligament defect (“type 3” according to Cilley classification Fig. 2b)3 has been closed by a 3-0 non-absorbable running barbed suture.
The postoperative course was excellent with no complications and the patient has been discharged at 3rd postoperative day. The follow up at 1 month was normal and the patient asymptomatic.
Quain first described the broad ligament internal hernia in 1861 as autopsy finding.4 73 years later, in 1934, Hunt proposed a classification for this kind of internal hernia. The “fenestra type” with a complete fenestration through a defect in the broad ligament (2 peritoneal layers); and the “pouch type” which involves hernia into the pouch from the anterior or posterior defect (1 peritoneal layer).2
In 1986 Cilley described the broad ligament defects depending on the anatomic localization. Type 1 defects occur caudal to the round ligament of the uterus. Type 2 defects occur above the round ligament. Type 3 defects occur between the round ligament and the remainder of the broad ligament, through the meso-ligamentum teres.3
The diagnosis of broad ligament internal hernia is intra-operative. It should be suspected in female patients with obstructive syndrome and without any prior history of laparotomy. CT-Scan has an important role in the diagnosis of mechanic obstruction.5
The causes of broad ligament defect are most of time acquired. Trauma from pregnancy, delivery, pelvic inflammatory disease, endometriosis or surgery are examples. A congenital cause should be suspected in nulliparous patients without any prior gynaecological event.1,6
Treatment is surgery and it consists in incarcerated hernia reduction, resection, if necessary, of necrotic bowel and defect closure. Traditional laparoscopy and SILS (Single-Incision-Laparoscopy) have been described as safe and with comparable morbidity and earlier recovery.6–9 It should be considered in diagnosis and treatment of internal hernia.
In our daily practice we prefer laparoscopic approach even for emergency surgery as internal hernia. Unfortunately the necrotic condition and its extension forced us to convert into laparotomy in order to prevent an abdominal contamination.
Broad ligament defect hernia is a surgical emergency which should be suspected and added to the list of differential diagnosis for female patients with obstructive syndrome or supra-pubic pain and without any prior laparotomy. Early diagnosis and surgical repair reduce morbidity and mortality for strangulation.
The current worldwide status10 cause of Covid-19 pandemia has created a fear system due to which patients hesitate to go to the hospital despite severe symptoms. The results is a more severe condition of the acute pathologies with serious impacts on morbidity and mortality.
We appreciate the help of the general surgery medical service and visceral hospital of Luxembourg, as well as the great work performed by the nursing team.
Please cite this article as: Pascotto B, Poulain V, Ghistelinck B, Azagra JS. Urgencias quirúrgicas no relacionadas con la pandemia COVID-19. Caso clínico: hernia interna yeyunal complicada con necrosis intestinal en el ligamento ancho útero-ovárico. Cir Esp. 2020. https://doi.org/10.1016/j.ciresp.2020.06.015