The results of parastomal hernia (PH) repair based on data from registries are scarce. The objective of this work is to analyze the data collected on PH in the National Registry of Incisional Hernia (EVEREG) and thus evaluate current practices and results in PH repair.
MethodsData from the PH cohort recorded in the period from July 2012 to June 2018 are analyzed. Complications, recurrences and associated factors of the entire PH cohort are analyzed, regardless of the type of stoma they are associated with. Subsequently, the same PH group analysis was performed in relation to a colostomy (larger group).
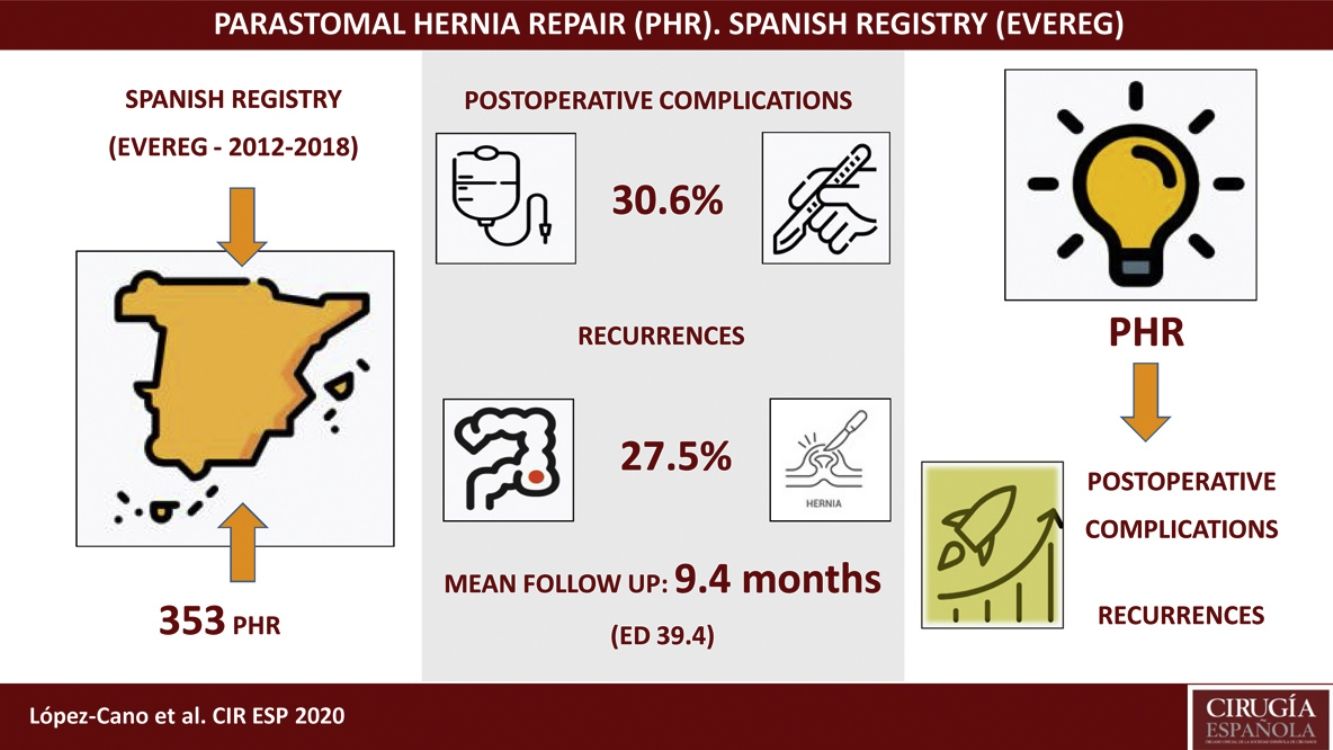
Results353 PH were studied. Of these, 259 (73%) were PH in the context of a terminal colostomy, 74 (21%) in the context of a terminal ileostomy, and 20 (6%) in the context of a ureteroileostomy (Bricker). The global mean age was 68.7 ± 11.1 years and 135 (38%) patients were female. The open approach and elective surgery were predominant (78% and 92% respectively); 99% were repaired with a non-absorbable synthetic mesh. Global postoperative complications were high (30.6%). As well as, the global recurrence (27.5%) after a mean follow-up of 9.4 months.
ConclusionsPH repair is infrequent. PH surgery seems to be associated with a high percentage of postoperative complications and recurrence.
Los resultados de la reparación de la hernia paraestomal (HP) basados en datos provenientes de registros son escasos. El objetivo del presente trabajo es analizar los datos recogidos sobre la HP en el Registro Nacional de Hernia Incisional (EVEREG) y así evaluar las prácticas actuales y resultados en la reparación de una HP.
MétodosSe analizan los datos de la cohorte de HP registradas en el período desde julio de 2012 hasta junio de 2018. Se analizan las complicaciones, recidivas y factores asociados a ellas de la cohorte completa de HP, independientemente del tipo de estoma al que se asocian. Posteriormente, se realiza el mismo análisis del grupo de HP con relación a una colostomía (grupo más numeroso).
ResultadosSe estudiaron 353 HP. De estas, 259 (73%) fueron HP en el contexto de una colostomía terminal, 74 (21%) en el de una ileostomía terminal y 20 (6%) en el de una ureteroileostomía (Bricker). La edad media global fue de 68,7 ± 11,1 años y 135 (38%) pacientes fueron del sexo femenino. El abordaje abierto y la cirugía electiva fueron predominantes (78% y 92%, respectivamente). El 99% se reparó con una malla sintética no absorbible. Las complicaciones postoperatorias globales fueron altas (30,6%), así como la recurrencia global (27,5%) tras un seguimiento medio de 9,4 meses.
ConclusionesLa reparación de la HP es poco frecuente comparada con el conjunto de reparaciones de la hernia incisional. La cirugía de la HP parece relacionarse con un porcentaje elevado de complicaciones postoperatorias y recidiva.
Parastomal hernia (PH) is a very common pathology that is observed in 78%–93% of radiology follow-up studies.1,2 To a greater or lesser degree, and regardless of the type of ostomy, PH will alter the patient’s quality of life, and elective surgical repair may be considered a treatment option.3 However, these repairs encompass a heterogeneous group of approaches (open and/or minimally invasive) that are associated with high rates of recurrence, and systematic reviews of the subject can only conclude that “…it is not possible to draw conclusions about which technique is preferred…”4 since “…the quality of the evidence for the various surgical techniques is low and does not lead to firm conclusions.”4 On the other hand, PH can present complications (i.e., intestinal obstruction, strangulation) and require urgent treatment. Here too, the information present in the literature offers very limited data.5,6
Observational studies based on surgical activity registries provide information on routine practice in non-selected patients and can answer questions that are more difficult to answer with other study designs (i.e., randomized studies), provide data on the efficacy of interventions in the general population, and offer a platform for the evaluation, follow-up and long-term use of surgical ‘instruments’ and/or the analysis of surgical innovation.7–9 In this context, in Spain there is a registry for incisional hernia (EVEREG), started in Catalonia in 2012 and promoted since 2013 by the Spanish Association of Surgeons (AEC) through the Abdominal Wall Division.10 EVEREG is one of the few registries of these characteristics present in Europe and the world,11 and in it PH surgeries are also registered and tracked.
The objective of this study is to analyze the data collected in EVEREG from its inception in July 2012 until June 2018, to describe patients who undergo PH surgery, and to analyze current practices and results for its repair among surgeons who participate in the EVEREG registry, both in elective and urgent surgery.
MethodsThe EVEREG database was designed with the OpenClinica computerized data entry platform, which is accessible online (http://www.evereg.es/) and allows for all cases of PH treated at participating hospitals (178 centers) to be registered anonymously. The database is permanently open to all centers that wish to participate. The practice of analyzing data from the registry, approval by committees, and data collection systematics have been described previously.10 Briefly, it is an online, prospective database maintained by surgeons from each hospital study center that collects data for patient parameters, hernia type, operations, complications, and clinical follow-up, as well as telephone follow-up, at one month, 6 months, one year and 2 years after surgery for each of the PH treated surgically. The registry is for hernias and not for patients, so patients with more than one hernia, or those who have been operated on several times for recurrences, may be repeatedly registered.
The independent variables analyzed in this study included patient demographic characteristics (age, sex, body mass index [BMI], diabetes mellitus [DM], chronic obstructive pulmonary disease [COPD], smoking), history of cancer, type of PH (colostomy, ileostomy or ureteroileostomy [Bricker]), the presence of an ASA (American Society of Anesthesiologists) greater than III and the ability to reduce PH (reducible or chronic incarceration). The outcome variables described in this study were: whether there was a previous mesh or not; whether a mesh repair was done, and whether it was placed in the prefascial (onlay), retromuscular (sublay) or intra-abdominal position; whether the hernia defect was closed; the type of surgical approach (open or laparoscopic); the presence of global complications, surgical site occurrence (SSO),12 surgical site infections (SSI),12 complications not related to the surgical site (respiratory, cardiac, etc.), postoperative complications according to the Clavien–Dindo classification,13 and lastly, whether the surgery was elective or urgent.
We analyzed the potential factors associated with complications and recurrence of the entire group. However, and given that the majority of PH corresponded with the colostomy group, this group was only used for the analysis of SSO, SSI, complications not related to the surgical site, and recurrence. The small number of patients included for ileostomy and ureteroileostomy (Bricker) did not allow for more than a descriptive statistical analysis of these groups.
Statistical analysisThe quantitative variables are expressed as mean ± standard deviation (SD) and the qualitative variables as proportions with their confidence interval. To analyze the association between qualitative variables, the chi-square test or Fisher’s test was used when necessary, as well as the Student’s t test or the Mann–Whitney test for quantitative variables. The normal distribution of the quantitative variables was verified using the Kolmogorov–Smirnov test. A P-value < .05 was considered statistically significant. The description of the variables and the statistical analysis were carried out using the SPSS® program (IBM, Armonk, New York, USA), version 21.
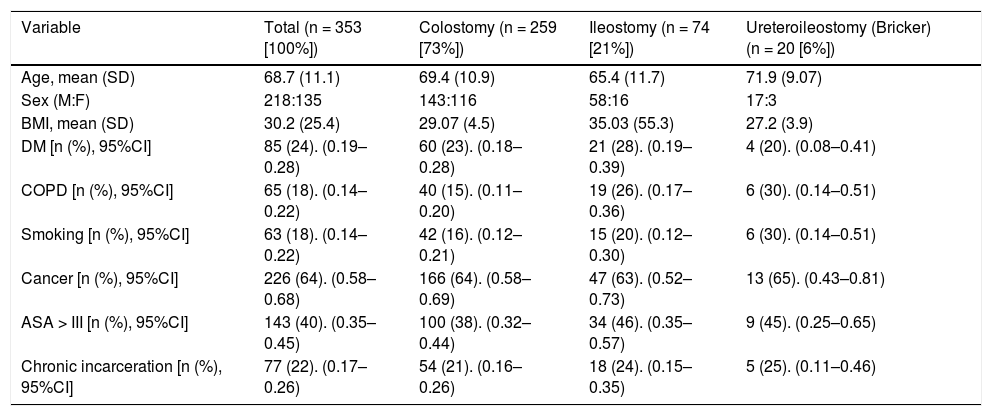
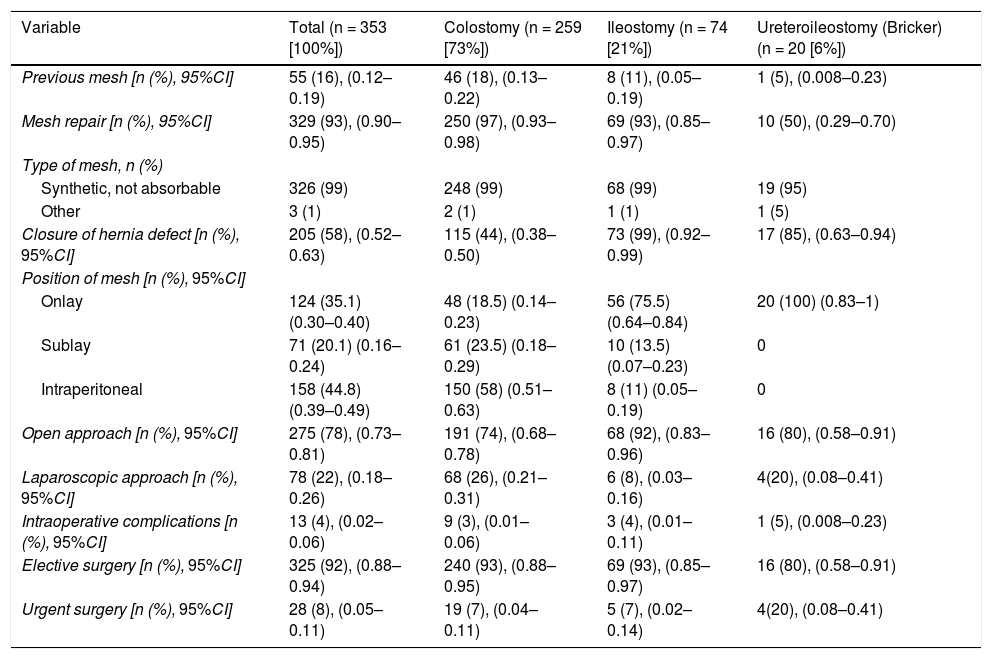
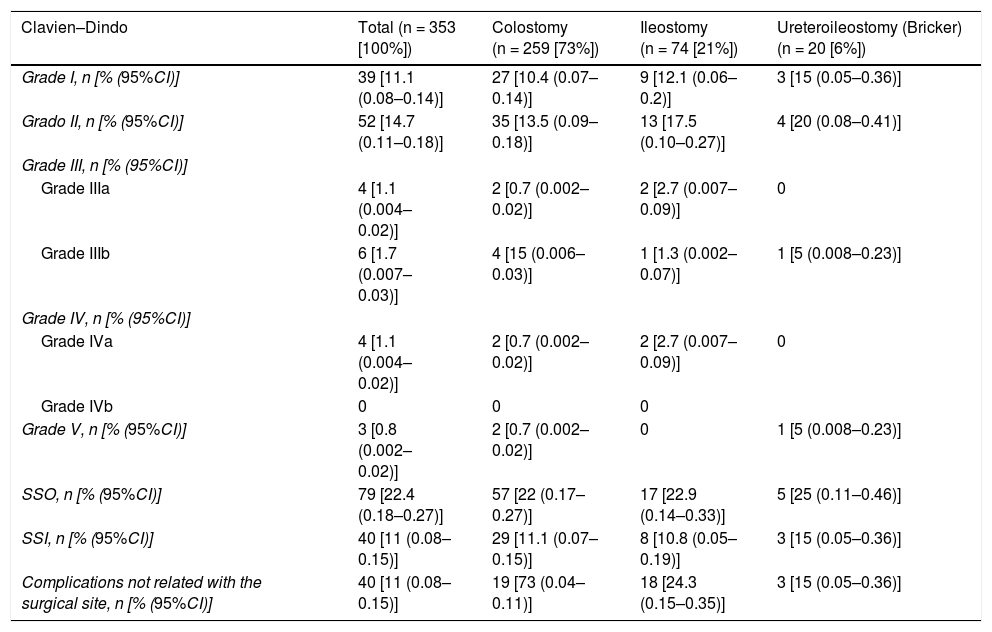
ResultsBetween July 2012 and June 2018, 8675 incisional hernia procedures were added to the registry, 353 (4%) of which were PH; 259 (73%) of these were PH in the context of an end colostomy, 74 (21%) in the context of an end ileostomy, and 20 (6%) in the context of ureteroileostomy (Bricker). Mean age was 68.7 ± 11.1 years, and 135 (38%) of the 353 patients were female. Table 1 shows the general demographic characteristics, broken down by the different types of PH. In the repair of PH in the global group, 55 (16%) of 353 patients had had a previous mesh. The open approach and elective surgery were predominant, with 275 (78%) and 325 (92%) of the 353 patients, respectively. The majority (326 [99%] of 353 patients) underwent repair with non-absorbable synthetic mesh, which was placed in an intraperitoneal position in 158 (44.8%) patients. The number of intraoperative complications was low, appearing in 13 (4%) patients of the total group. The characteristics of the surgical procedure of the total group, and broken down according to the type of PH, are presented in Table 2. Postoperative complications occurred in 108 (30.6%) patients of the total group. These complications are shown in Table 3 according to the Clavien–Dindo classification, together with the categorization as SSO, SSI and those not related to the surgical site.
Patient characteristics.
| Variable | Total (n = 353 [100%]) | Colostomy (n = 259 [73%]) | Ileostomy (n = 74 [21%]) | Ureteroileostomy (Bricker) (n = 20 [6%]) |
|---|---|---|---|---|
| Age, mean (SD) | 68.7 (11.1) | 69.4 (10.9) | 65.4 (11.7) | 71.9 (9.07) |
| Sex (M:F) | 218:135 | 143:116 | 58:16 | 17:3 |
| BMI, mean (SD) | 30.2 (25.4) | 29.07 (4.5) | 35.03 (55.3) | 27.2 (3.9) |
| DM [n (%), 95%CI] | 85 (24). (0.19–0.28) | 60 (23). (0.18–0.28) | 21 (28). (0.19–0.39) | 4 (20). (0.08–0.41) |
| COPD [n (%), 95%CI] | 65 (18). (0.14–0.22) | 40 (15). (0.11–0.20) | 19 (26). (0.17–0.36) | 6 (30). (0.14–0.51) |
| Smoking [n (%), 95%CI] | 63 (18). (0.14–0.22) | 42 (16). (0.12–0.21) | 15 (20). (0.12–0.30) | 6 (30). (0.14–0.51) |
| Cancer [n (%), 95%CI] | 226 (64). (0.58–0.68) | 166 (64). (0.58–0.69) | 47 (63). (0.52–0.73) | 13 (65). (0.43–0.81) |
| ASA > III [n (%), 95%CI] | 143 (40). (0.35–0.45) | 100 (38). (0.32–0.44) | 34 (46). (0.35–0.57) | 9 (45). (0.25–0.65) |
| Chronic incarceration [n (%), 95%CI] | 77 (22). (0.17–0.26) | 54 (21). (0.16–0.26) | 18 (24). (0.15–0.35) | 5 (25). (0.11–0.46) |
ASA: American Society of Anesthesiologists; SD: standard deviation; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; F: female; 95%CI: 95% confidence interval; BMI: body mass index; M: male.
Characteristics of the procedure.
| Variable | Total (n = 353 [100%]) | Colostomy (n = 259 [73%]) | Ileostomy (n = 74 [21%]) | Ureteroileostomy (Bricker) (n = 20 [6%]) |
|---|---|---|---|---|
| Previous mesh [n (%), 95%CI] | 55 (16), (0.12–0.19) | 46 (18), (0.13–0.22) | 8 (11), (0.05–0.19) | 1 (5), (0.008–0.23) |
| Mesh repair [n (%), 95%CI] | 329 (93), (0.90–0.95) | 250 (97), (0.93–0.98) | 69 (93), (0.85–0.97) | 10 (50), (0.29–0.70) |
| Type of mesh, n (%) | ||||
| Synthetic, not absorbable | 326 (99) | 248 (99) | 68 (99) | 19 (95) |
| Other | 3 (1) | 2 (1) | 1 (1) | 1 (5) |
| Closure of hernia defect [n (%), 95%CI] | 205 (58), (0.52–0.63) | 115 (44), (0.38–0.50) | 73 (99), (0.92–0.99) | 17 (85), (0.63–0.94) |
| Position of mesh [n (%), 95%CI] | ||||
| Onlay | 124 (35.1) (0.30–0.40) | 48 (18.5) (0.14–0.23) | 56 (75.5) (0.64–0.84) | 20 (100) (0.83–1) |
| Sublay | 71 (20.1) (0.16–0.24) | 61 (23.5) (0.18–0.29) | 10 (13.5) (0.07–0.23) | 0 |
| Intraperitoneal | 158 (44.8) (0.39–0.49) | 150 (58) (0.51–0.63) | 8 (11) (0.05–0.19) | 0 |
| Open approach [n (%), 95%CI] | 275 (78), (0.73–0.81) | 191 (74), (0.68–0.78) | 68 (92), (0.83–0.96) | 16 (80), (0.58–0.91) |
| Laparoscopic approach [n (%), 95%CI] | 78 (22), (0.18–0.26) | 68 (26), (0.21–0.31) | 6 (8), (0.03–0.16) | 4(20), (0.08–0.41) |
| Intraoperative complications [n (%), 95%CI] | 13 (4), (0.02–0.06) | 9 (3), (0.01–0.06) | 3 (4), (0.01–0.11) | 1 (5), (0.008–0.23) |
| Elective surgery [n (%), 95%CI] | 325 (92), (0.88–0.94) | 240 (93), (0.88–0.95) | 69 (93), (0.85–0.97) | 16 (80), (0.58–0.91) |
| Urgent surgery [n (%), 95%CI] | 28 (8), (0.05–0.11) | 19 (7), (0.04–0.11) | 5 (7), (0.02–0.14) | 4(20), (0.08–0.41) |
95%CI: 95% confidence interval.
Postoperative complications.
| Clavien–Dindo | Total (n = 353 [100%]) | Colostomy (n = 259 [73%]) | Ileostomy (n = 74 [21%]) | Ureteroileostomy (Bricker) (n = 20 [6%]) |
|---|---|---|---|---|
| Grade I, n [% (95%CI)] | 39 [11.1 (0.08–0.14)] | 27 [10.4 (0.07–0.14)] | 9 [12.1 (0.06–0.2)] | 3 [15 (0.05–0.36)] |
| Grado II, n [% (95%CI)] | 52 [14.7 (0.11–0.18)] | 35 [13.5 (0.09–0.18)] | 13 [17.5 (0.10–0.27)] | 4 [20 (0.08–0.41)] |
| Grade III, n [% (95%CI)] | ||||
| Grade IIIa | 4 [1.1 (0.004–0.02)] | 2 [0.7 (0.002–0.02)] | 2 [2.7 (0.007–0.09)] | 0 |
| Grade IIIb | 6 [1.7 (0.007–0.03)] | 4 [15 (0.006–0.03)] | 1 [1.3 (0.002–0.07)] | 1 [5 (0.008–0.23)] |
| Grade IV, n [% (95%CI)] | ||||
| Grade IVa | 4 [1.1 (0.004–0.02)] | 2 [0.7 (0.002–0.02)] | 2 [2.7 (0.007–0.09)] | 0 |
| Grade IVb | 0 | 0 | 0 | |
| Grade V, n [% (95%CI)] | 3 [0.8 (0.002–0.02)] | 2 [0.7 (0.002–0.02)] | 0 | 1 [5 (0.008–0.23)] |
| SSO, n [% (95%CI)] | 79 [22.4 (0.18–0.27)] | 57 [22 (0.17–0.27)] | 17 [22.9 (0.14–0.33)] | 5 [25 (0.11–0.46)] |
| SSI, n [% (95%CI)] | 40 [11 (0.08–0.15)] | 29 [11.1 (0.07–0.15)] | 8 [10.8 (0.05–0.19)] | 3 [15 (0.05–0.36)] |
| Complications not related with the surgical site, n [% (95%CI)] | 40 [11 (0.08–0.15)] | 19 [73 (0.04–0.11)] | 18 [24.3 (0.15–0.35)] | 3 [15 (0.05–0.36)] |
95%CI: 95% confidence interval; SSI: surgical site infections; SSO: surgical site complications.
Follow-up was not possible for the entire series and included 149 (42.2%) of the 353 patients for a minimum period of 6 months. The reason for excluding the remaining registries was the absence of follow-up data. For the colostomy group was also not complete for the same reason, with data available for 108 (42%) of 259 patients. The mean follow-up was 9.4 months (SD 39.4; 95%CI 5.3–13.5) for the total group and 9.2 months (SD 32.6; 95%CI 5.2–13.1) for the colostomy group. During this follow-up period, a total of 41 (27.5%) out of 149 patients with PH recurrence were registered, and 34 (31.5%) out of 108 patients belonged to the colostomy group. Mortality during the follow-up period was 9/149 patients (6%); all deaths were unrelated to the PH intervention.
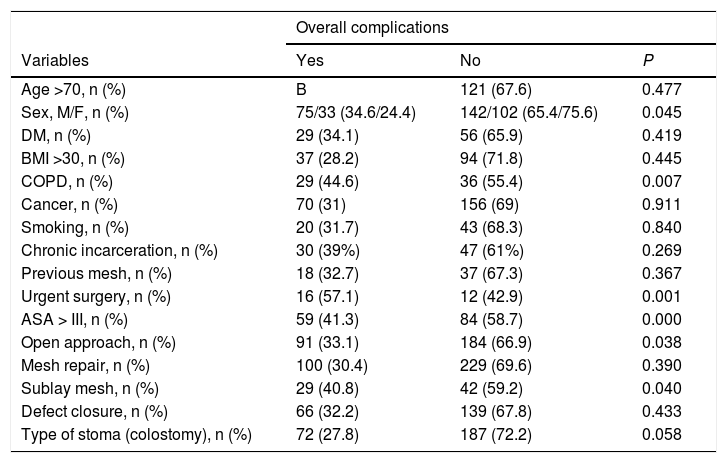
The analysis of the factors associated with the global complications of the complete series showed that the demographic variables of sex (P = .045), COPD (P = .007) and ASA greater than III (P = .000) were significantly associated with a higher incidence of complications. Furthermore, in this same series, the open surgical approach and the mesh in a sublay position were associated with more complications, showing significant P values of .038 and .040, respectively (Table 4).
Complications of the total series.
| Overall complications | |||
|---|---|---|---|
| Variables | Yes | No | P |
| Age >70, n (%) | B | 121 (67.6) | 0.477 |
| Sex, M/F, n (%) | 75/33 (34.6/24.4) | 142/102 (65.4/75.6) | 0.045 |
| DM, n (%) | 29 (34.1) | 56 (65.9) | 0.419 |
| BMI >30, n (%) | 37 (28.2) | 94 (71.8) | 0.445 |
| COPD, n (%) | 29 (44.6) | 36 (55.4) | 0.007 |
| Cancer, n (%) | 70 (31) | 156 (69) | 0.911 |
| Smoking, n (%) | 20 (31.7) | 43 (68.3) | 0.840 |
| Chronic incarceration, n (%) | 30 (39%) | 47 (61%) | 0.269 |
| Previous mesh, n (%) | 18 (32.7) | 37 (67.3) | 0.367 |
| Urgent surgery, n (%) | 16 (57.1) | 12 (42.9) | 0.001 |
| ASA > III, n (%) | 59 (41.3) | 84 (58.7) | 0.000 |
| Open approach, n (%) | 91 (33.1) | 184 (66.9) | 0.038 |
| Mesh repair, n (%) | 100 (30.4) | 229 (69.6) | 0.390 |
| Sublay mesh, n (%) | 29 (40.8) | 42 (59.2) | 0.040 |
| Defect closure, n (%) | 66 (32.2) | 139 (67.8) | 0.433 |
| Type of stoma (colostomy), n (%) | 72 (27.8) | 187 (72.2) | 0.058 |
ASA: American Society of Anesthesiologists; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; BMI: body mass index.
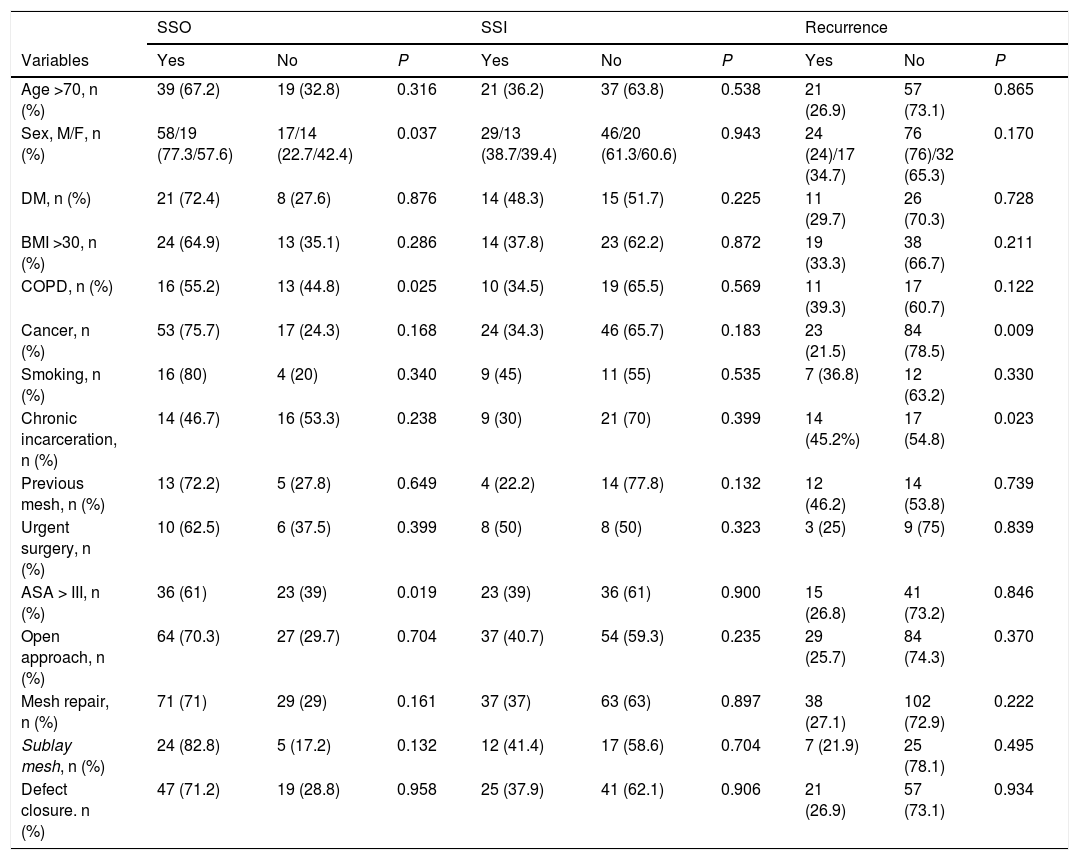
The analysis of the specific colostomy group showed that complications unrelated to the surgical site were more frequent in patients over 70 years of age (P = .015) and in patients with an ASA greater than III (P = .008). In this same colostomy group, SSO appeared more frequently among females (P = .037), patients with COPD (P = .025) and those with an ASA greater than III (P = .019). No variable was found to be significantly associated with a higher incidence of SSI. However, recurrence in patients with colostomy was significantly higher in patients with a history of cancer surgery (P = .009) and in those who presented PH with chronic incarceration (P = .023). The analysis of the factors associated with SSO, SSI, and recurrence in the colostomy group are presented in Table 5.
Factors associated with SSO, SSI and recurrence in the colostomy group.
| SSO | SSI | Recurrence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Yes | No | P | Yes | No | P | Yes | No | P |
| Age >70, n (%) | 39 (67.2) | 19 (32.8) | 0.316 | 21 (36.2) | 37 (63.8) | 0.538 | 21 (26.9) | 57 (73.1) | 0.865 |
| Sex, M/F, n (%) | 58/19 (77.3/57.6) | 17/14 (22.7/42.4) | 0.037 | 29/13 (38.7/39.4) | 46/20 (61.3/60.6) | 0.943 | 24 (24)/17 (34.7) | 76 (76)/32 (65.3) | 0.170 |
| DM, n (%) | 21 (72.4) | 8 (27.6) | 0.876 | 14 (48.3) | 15 (51.7) | 0.225 | 11 (29.7) | 26 (70.3) | 0.728 |
| BMI >30, n (%) | 24 (64.9) | 13 (35.1) | 0.286 | 14 (37.8) | 23 (62.2) | 0.872 | 19 (33.3) | 38 (66.7) | 0.211 |
| COPD, n (%) | 16 (55.2) | 13 (44.8) | 0.025 | 10 (34.5) | 19 (65.5) | 0.569 | 11 (39.3) | 17 (60.7) | 0.122 |
| Cancer, n (%) | 53 (75.7) | 17 (24.3) | 0.168 | 24 (34.3) | 46 (65.7) | 0.183 | 23 (21.5) | 84 (78.5) | 0.009 |
| Smoking, n (%) | 16 (80) | 4 (20) | 0.340 | 9 (45) | 11 (55) | 0.535 | 7 (36.8) | 12 (63.2) | 0.330 |
| Chronic incarceration, n (%) | 14 (46.7) | 16 (53.3) | 0.238 | 9 (30) | 21 (70) | 0.399 | 14 (45.2%) | 17 (54.8) | 0.023 |
| Previous mesh, n (%) | 13 (72.2) | 5 (27.8) | 0.649 | 4 (22.2) | 14 (77.8) | 0.132 | 12 (46.2) | 14 (53.8) | 0.739 |
| Urgent surgery, n (%) | 10 (62.5) | 6 (37.5) | 0.399 | 8 (50) | 8 (50) | 0.323 | 3 (25) | 9 (75) | 0.839 |
| ASA > III, n (%) | 36 (61) | 23 (39) | 0.019 | 23 (39) | 36 (61) | 0.900 | 15 (26.8) | 41 (73.2) | 0.846 |
| Open approach, n (%) | 64 (70.3) | 27 (29.7) | 0.704 | 37 (40.7) | 54 (59.3) | 0.235 | 29 (25.7) | 84 (74.3) | 0.370 |
| Mesh repair, n (%) | 71 (71) | 29 (29) | 0.161 | 37 (37) | 63 (63) | 0.897 | 38 (27.1) | 102 (72.9) | 0.222 |
| Sublay mesh, n (%) | 24 (82.8) | 5 (17.2) | 0.132 | 12 (41.4) | 17 (58.6) | 0.704 | 7 (21.9) | 25 (78.1) | 0.495 |
| Defect closure. n (%) | 47 (71.2) | 19 (28.8) | 0.958 | 25 (37.9) | 41 (62.1) | 0.906 | 21 (26.9) | 57 (73.1) | 0.934 |
ASA: American Society of Anesthesiologists; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; BMI: body mass index; SSI: surgical site infections; SSO: surgical site complications.
The availability of a registry like EVEREG has allowed us to conduct this prospective observational study of 353 repaired PH. To date, only a few studies from the limited registries worldwide, such as the Americas Hernia Society Quality Collaborative (AHSQG)14 or the Danish hernia registry,15 offer similar numbers to ours.
PH is an incisional hernia related to the presence of a stoma in the abdominal wall16; however, in our registry, only 4% of repaired incisional hernias are PH. This could be in line with the belief that surgeons in general are reluctant to repair PH due to the unsatisfactory results of such surgery in terms of morbidity and recurrence.14,15 The mean age of the patients who underwent PH repair in our registry was 68 years, which is similar to the results of other registries that place it at 66.14,15 The distribution by sex is variable in the aforementioned registries; in ours, a predominance of males was observed. It is not surprising that the repair of a PH secondary to a colostomy is most frequently registered (73%), since this type of PH is also described as the most frequent.17 The surgical approach (open vs laparoscopic) of PH is a controversial issue, and one systematic review does not ‘clarify’ which should be the approach of choice given the low level of evidence in the literature.4 However, other reviews indicate that the laparoscopic approach (modified Sugarbaker) may provide the best results.18 Our study shows that the open surgical approach was most frequently used in 78% of the total. To explain this, it is tempting to resort to the argument that laparoscopic abdominal wall surgery (i.e., incisional hernia) in our country is below international standards.19 However, it is interesting to observe how registries from other countries that theoretically would be expected to have high percentages of laparoscopic PH surgery report open surgery rates of up to 80%.14 In our registry, 92% of the patients were treated electively and mostly with non-absorbable synthetic mesh. This is along the same line as other registries14 and in accordance with the recommendations for the use of mesh by the recent guidelines of the European Hernia Society (EHS) on the prevention and treatment of PH.20 Furthermore, it is interesting to note that intraoperative complications were low (4%), but postoperative complications of PH surgery (globally and for the colostomy group) presented high percentages. In our opinion, the data of other registries on this matter are discordant: some describe complication rates between 9% and 15%,14 while others conclude that it is a surgery with high morbidity.15
Our data are in line with those of other European registries15 and we can affirm that PH surgery considered as a whole, and specifically for hernias associated with colostomy, is a surgery with high postoperative morbidity rates. Male sex, COPD, and patients with ASA class III or higher were shown to significantly increase complications globally, and specifically for colostomy. Other variables also significantly increased global complications, some perhaps logically (such as urgent surgery) and others (such as the open approach) perhaps due to greater exposure and manipulation of the stoma. Furthermore, it is interesting to observe how the sublay mesh placement technique also significantly increased complications. In any case and as mentioned above, in our context this surgery is associated with a high percentage of complications, most of which belong to Clavien–Dindo grade I or II.13 Likewise, it seems that laparoscopic surgery is significantly associated with fewer complications, although the open approach was the most frequently used.
Regarding the limited number of urgent cases registered (28%), we do not dare generalize the idea that few PH are repaired in the context of emergencies. The very nature of the registries and their data collection context can result in the tendency to collect mostly elective cases. The small number of urgent cases in the registry does not allow for an adequate analysis of this type of surgery in the context of PH.
Recurrence was high in both the total group (27.5%) and the colostomy group (31.5%), especially considering the short follow-up period. These high percentages are also observed in other registries14,15 and again demonstrate the difficulty of surgical treatment of PH in terms of recurrence, while trying to solve the conundrum of ‘closing’ a hernial orifice without actually closing it. In our registry, only the history of cancer and preoperative chronic incarceration in the colostomy group were shown to be variables significantly associated with recurrence.
This study has limitations, mainly derived from an incomplete observational analysis of all the registry data. Unfortunately, the incomplete recording of data, such as mesh fixation methods or the number of previous repairs, does not allow us to establish a more complete view of PH surgery. In addition to the incomplete registry, another important limitation is the impossibility to follow up all the registered patients, although these problems have also been mentioned as limitations of other registries.15 This could determine that the data shown here, especially data referring to recurrence, could even potentially be lower than those that would have been found if all patients had been followed. Furthermore, the data presented here do not pretend to represent the whole of PH surgery throughout the country, and, although the sample is large, it only presents the experience of the centers included in EVEREG, potentially producing biases related to the type of patients and the hospitals that treat them. On the other hand, the analyses of the entire series and then of the colostomy group alone limit the generalization of the data to PH associated with other types of stomata. The fact that it is essentially an analysis of PH in an elective context also limits the extension of the results to urgent surgery. The strengths of our study are the high number of PH analyzed, probably the second largest series of elective surgery analyzed to date and present in the literature. Furthermore, the data are multi-institutional and not limited to the experience of a single center, thus offering a ‘real world’ view of the data included prospectively in a registry.
In summary, PH repair is rare compared to incisional hernia repairs as a whole, and those that are most frequently repaired are related to end colostomies. PH surgery in our registry seems to be associated with a high percentage of complications. The open mesh approach is the most widely used, and laparoscopic surgery is associated with fewer complications. The recurrence of PH treated in the context of elective surgery is very high.
FundingNone.
Conflict of interestsThe authors have no conflicts of interest related with the study presented.
The authors would like to thank: Silvia Martínez and Xavier Masramón; SAIL (Servicio de Asesoría a la Investigación y Logística).
Antonio Utrera González, Hospital Juan Ramón Jiménez, Huelva
José M, Capitán Vallvey, Complejo Hospitalario de Jaén, Jaén
Matías Pradas, Hospital Comarcal de Ronda, Ronda, Málaga
Daniel Pérez Gomar, Hospital Universitario Puerta del Mar, Cádiz
Manuel Bustos, Hospital Virgen del Rocío, Sevilla
Francisco Antonio Herrera Fernández, Hospital Comarcal Santa Ana, Motril
Juan A, Blanco, Hospital Civil de Málaga
Joaquim Robres Puig, Consorci Sanitari Integral de l’Hospitalet, Barcelona
Rafael Villalobos, Hospital Arnau de Vilanova, Lleida
Dolors Güell Puigcercós, Hospital de Terrassa, Terrassa
José María Puigcercós Fusté, Hospital Dos de Maig, Barcelona
Vicente Ayuso Osuna, Hospital Espíritu Santo, Santa Coloma Gramanet, Barcelona
Marta Piñol, Hospital Espíritu Santo, Santa Coloma Gramanet, Barcelona
Carles Olona Cases, Hospital Joan XXIII, Tarragona
Francisco Martínez Ródenas, Hospital Municipal de Badalona, Badalona
Jordi Comajuncosas, Hospital Parc Sanitari Sant Joan de Déu, Sant Boi
Enric Sebastián Valverde, Hospital Parc Sanitari Sant Joan de Déu, Sant Boi
Sara Amador, Hospital de Granollers
Jaume Gelonch, Hospital de Palamós
Helena Vallverdú, Hospital de Vic
Magda Abelló Sala, Hospital Pius, Valls
Antonio Veres Gómez, Hospital de la Cerdaña
Rosa Gamón, Hospital General de Castellón
Pedro García Peche, Hospital General Universitario Reina Sofía, Elche
Miguel González Valverde, Hospital General Universitario Reina Sofía, Elche
Miguel Angel Martín Blanco, Hospital de Vinaroz, Castellón
Ramón J Ferri, Hospital Lluís Alcanyís, Valencia
Elena Martí Ciñat, Hospital Malvarrosa, Valencia
Providencia García Pastor, Hospital Universitario La Fe, Valencia
Carlos Montero, Hospital Virgen de los Lirios, Alcoy
Miguel Ángel Lorenzo Liñán, Hospital General de Onteniente, Valencia
Vicente Barbero, Complejo Hospitalario Virgen de la Salud, Toledo
Miguel Ángel Morlan, Complejo Hospitalario Virgen de la Salud, Toledo
José María Jover, Hospital de Getafe, Madrid
Isabel Delgado Lillo, Hospital Clínico San Carlos, Madrid
María Mercedes Sanz Sánchez, Hospital General Universitario Gregorio Marañón, Madrid
Leire Zarain Obrador, Hospital General Universitario Gregorio Marañón, Madrid
Alejandro Lusilla, Hospital General Universitario Gregorio Marañón, Madrid
Juan Jesús Cabeza Gómez, Hospital Clínico San Carlos, Madrid
Teresa Butrón, Hospital Universitario 12 de Octubre, Madrid
Guillermo Supelano Eslait, Hospital Universitario 12 de Octubre, Madrid
José Luis Álvarez Conde, Complejo Hospitalario de Palencia
Baltasar Pérez Saborido, Hospital Río Ortega, Valladolid
Mario Rodríguez López, Hospital Río Ortega, Valladolid
Santiago Revuelta Álvarez, Hospital Universitario Marqués de Valdecilla, Santander
Pedro Trillo Parejo, Complexo Hospitalario Universitario, Orense
José Luis Rodicio, Hospital Universitario Central de Asturias, Oviedo
Antonio Blanco, Hospital Universitario Central de Asturias, Oviedo
Jacobo Trébol López, Complejo Asistencial Universitario de Salamanca
Ramón Castañera González, Complejo Hospitalario de Palencia
Gian Pier Protti, Hospital Arnau de Vilanova, Lleida
Damián Turiño Luque, Hospital Civil de Málaga
Juan José Espert, Hospital Clínic i Provincial de Barcelona
Carmen Zaragoza, Hospital de Alicante
Marta Hidalgo Pujol, Hospital de Bellvitge
Daniel Carmona Navarro, Hospital de Igualada, Barcelona
Álvaro Valdés de Anca, Hospital de La Princesa, Madrid
Laura Fresno de Prado, Hospital del Mar, Barcelona
Antonio Nieto Soler, Hospital de Mérida-Almendralejo
Francisca Vasco Rodríguez, Hospital de Palamós, Girona
Roberto Lozoya Trujillo, Hospital de Sagunto, Valencia
M, Pilar Anaya Reig, Hospital General de Onteniente, Valencia
M, Mercedes Sanz Sánchez, Hospital General Universitario Gregorio Marañón, Madrid
José Bueno Lledó, Hospital La Fe, Valencia
Salvador Pous Serrano, Hospital La Fe, Valencia
Elena Martí Cuñat, Hospital Malvarrosa, Valencia
Ernest Bombuy Giménez, Hospital Mataró, Barcelona
Esther Mans, Hospital Mataró, Barcelona
Aparicio García, Hospital Nuestra Sra, del Prado de Talavera de la Reina, Toledo
Elena Ortega Ortega, Hospital Nuestra Sra, del Prado de Talavera de la Reina, Toledo
Enric Sebastián, Hospital Parc Sanitari Sant Joan de Déu, Sant Boi, Barcelona
Carlos Hoyuela Alonso, Hospital Plató, Barcelona
Raquel Grajal Marino, Hospital Santos Reyes, Aranda de Duero, Burgos
Lofti Elmalaki Hossain, Hospital Universitario de Ceuta
Raul Medina, Hospital Universitario de Gran Canaria Doctor Negrín, Las Palmas de Gran Canaria
José Daniel Sánchez, Hospital Universitario Infanta Sofía, Madrid
Tomas Ratia Giménez, Hospital Universitario Príncipe de Asturias, Madrid
Antonio López, H. Univ. Guadalajara
Rosa Ana García Díaz, H. Univ. Marqués de Valdecilla, Santander
Itziar Larrañaga, Mutua de Terrassa, Barcelona
Please cite this article as: López-Cano M, Pereira JA, Rodrigues-Gonçalves V, Verdaguer-Tremolosa M, Hernández-Granados P, Bravo-Salvá A, et al. Reparación de la hernia paraestomal. Estudio observacional prospectivo basado en el Registro Español de Hernia Incisional (EVEREG). Cir Esp. 2021;99:527–534.