The COVID-19 pandemic led to the cancellation of non-essential surgical procedures in March 2020. With the resumption of surgical activity, patients undergoing surgery were one of the first population groups to be systematically tested for PCR. The aim of this study was to determine the prevalence of asymptomatic SARS-CoV-2 carriers after the resumption of non-essential surgical activity.
MethodsRetrospective multicenter observational study of patients scheduled for surgery or undergoing emergency surgery in Catalonia between 20 April and 31 May 2020. The microbiological results of preoperative PCR tests and clinical records were reviewed, and an epidemiological survey was conducted on patients with positive PCR for SARS-CoV-2.
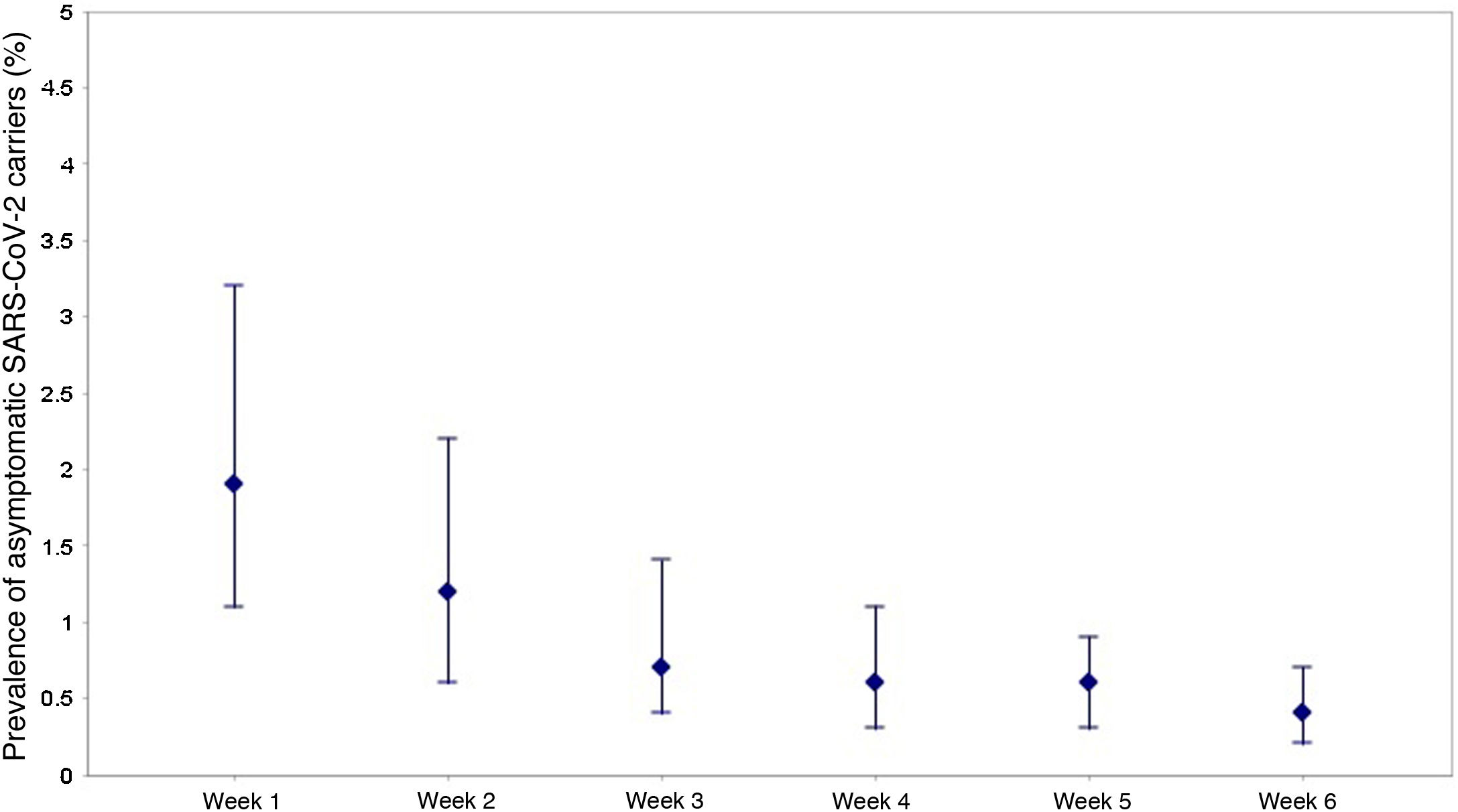
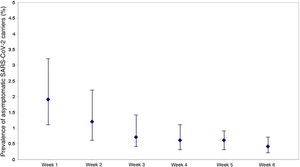
ResultsA total of 10,838 patients scheduled for surgery or who underwent emergency surgery were screened for COVID-19. One hundred and eighteen patients (1.09%) were positive for SARS-CoV-2 in the 72 h prior to surgery. The prevalence of asymptomatic carriers was 0.7% (IC95%: 0.6%–0.9%). The first week of the study presented the highest prevalence of asymptomatic carriers [1.9% (CI95%:1.1%–3.2%)].
ConclusionsThe low levels of asymptomatic carriers of COVID-19 infection obtained in the surgical population of hospitals in Catalonia after the resumption of surgical activity, shows that most patients were able to undergo surgical procedures without the risks of COVID-19 associated complications in the perioperative period.
La pandemia producida por COVID-19 ocasionó la cancelación de los procedimientos quirúrgicos no esenciales en marzo de 2020. Con el reinicio de la actividad quirúrgica, los pacientes que se sometían a una cirugía fueron uno de los primeros grupos poblacionales a los que se realizó test PCR de forma sistemática. El objetivo de este estudio fue determinar la prevalencia de portadores asintomáticos de SARS-CoV-2 tras el reinicio de la actividad quirúrgica no esencial.
MétodosEstudio observacional multicéntrico retrospectivo de los pacientes programados para cirugía o que se sometieron a cirugía urgente en Cataluña entre el 20 de abril y el 31 de mayo de 2020. Se revisaron los resultados microbiológicos de los test PCR preoperatorios, las historias clínicas y se realizó una encuesta epidemiológica a los pacientes con PCR positiva para SARS-CoV-2.
ResultadosUn total de 10.838 pacientes programados para una intervención quirúrgica o a los que se realizó a una cirugía urgente, fueron sometidos a cribaje para COVID-19. Ciento dieciocho pacientes (1,09%) fueron positivos para SARS-CoV-2 en las 72 h previas a la cirugía. La prevalencia de portadores asintomáticos fue del 0,7% (IC95%:0,6%–0,9%). La primera semana del estudio presentó la prevalencia más alta de portadores asintomáticos [1,9%(IC95%:1,1%–3,2%)].
ConclusionesLos bajos niveles de portadores asintomáticos de infección por COVID-19 obtenidos en la población quirúrgica de los hospitales de Cataluña tras el reinicio de la actividad quirúrgica, muestra que la mayoría de pacientes se pudieron someter a procedimientos quirúrgicos sin los riesgos de las complicaciones asociadas al COVID-19 en el periodo perioperatorio.
Coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared a global pandemic by the World Health Organization (WHO) on March 11, 20201. The clinical manifestations of SARS-CoV-2 infection are extremely variable and can range from severe life-threatening disease to paucisymptomatic or asymptomatic forms2. The incubation period ranges from 2 to 14 days after exposure to the virus, and the first symptoms appear within the first 5 days of exposure in 50% of cases3. Transmission from asymptomatic or presymptomatic subjects has been clearly documented, and the proportion of asymptomatic infections is between 0.13% and 41%, according to different studies4–9.
Spain has been one of the European countries most severely affected by the COVID-19 pandemic during the first wave10,11. The results of the Seroepidemiological Survey of SARS-CoV-2 Virus Infection in Spain (ENE-COVID) conducted between April 27 and May 11, 2020, showed a global seroprevalence in Spain of 5%. In Catalonia, the prevalence by province was 7% in Barcelona, 3.8% in Lleida, 2.6% in Girona and 1.4% in Tarragona12.
The exponential increase in cases caused restrictive policies to be initiated as part of the ‘state of alarm’ declared in Spain on March 14 to reduce the risk of transmission of SARS-CoV-213,14. Likewise, the COVID-19 pandemic posed a great challenge for the healthcare system in Spain. Due to the patient overload of hospitals in March 2020, non-essential surgical procedures were cancelled, and surgery units were converted into COVID-19 wards and intensive care units in order to treat the disease. Furthermore, the lack of availability of diagnostic tests at the beginning of the pandemic meant that there was no standardized screening of most of the population with clinical suspicion of infection in the absence of serious symptoms or requiring hospital admission. In this regard, real-time reverse transcription polymerase chain reaction (PCR) in nasopharyngeal samples is currently the gold standard for diagnosing patients with active SARS-CoV-2 infection7. As surgical activity gradually restarted, hospitals resumed scheduled surgical activity. In this phase, the authorities proposed PCR screening strategies in different groups, including patients who were going to undergo surgery. Following the recommendations established by the Ministry of Health, most hospitals added PCR testing with a nasopharyngeal sample to their preoperative protocols as screening for active SARS-CoV-2 infection in the 72 h prior to a scheduled surgery and in the immediate preoperative period in the case of urgent surgery15,16. This meant that patients who underwent surgery were one of the first population groups in whom PCR testing became universalized. The application of screening protocols using PCR was generalized in all hospitals in Catalonia. Given the limited information available on the number of asymptomatic carriers (AC), the data generated in the preoperative screening can provide important information on the epidemiological situation in Catalonia in the period immediately after the resumption of surgical activity. The main objective of this study was to determine the prevalence of asymptomatic SARS-CoV-2 carriers in the surgical population in Catalonia after the restart of scheduled activity during the first wave of the pandemic.
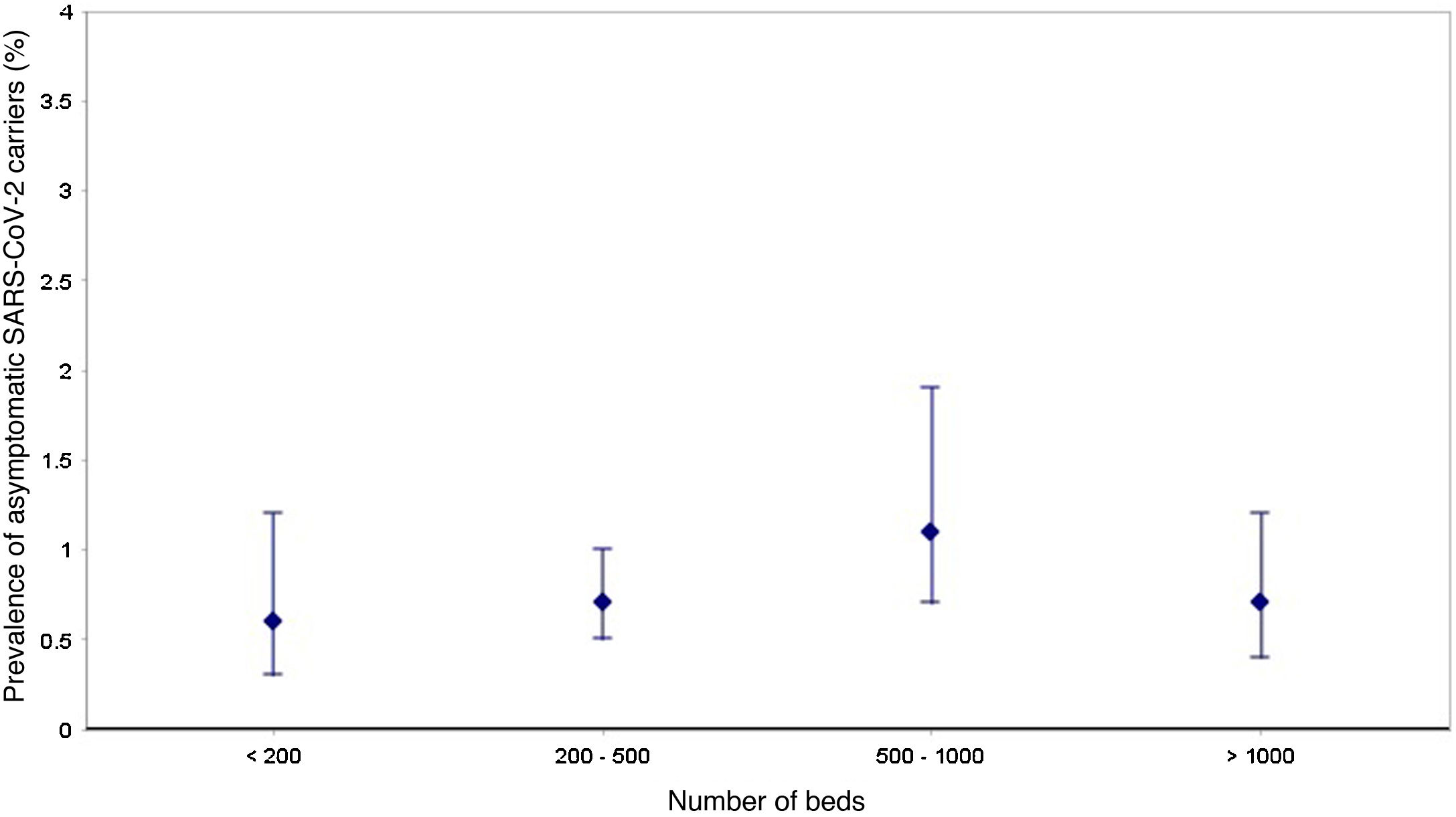
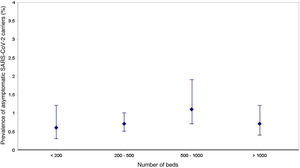
MethodsWe conducted a retrospective multicenter observational study of patients who were either scheduled for surgery or underwent urgent surgery in 17 hospitals in Catalonia between April 20 and May 31, 2020 (6 weeks). The hospitals were classified by groups based on the number of beds: 5 hospitals had less than 200 beds, 9 between 200 and 500 beds, 2 between 500 and 1000, and one more than 1000 beds. This study was approved by the Ethics Committee of Hospital Vall d'Hebron (Barcelona, Spain) (Ethics Committee approval number [PR(AG)331/2020]). The study start date of April 20 was chosen because it was the date that scheduled surgical activity was restarted in most medical centers after having been suspended due to the COVID-19 pandemic. Since then, surgical activity was resumed and hospital protocols as well as the recommendations of the Ministry of Health have been followed15,16, and all hospitals in Catalonia have performed PCR tests using nasopharyngeal samples from all patients requiring scheduled or urgent surgery in order to screen for active SARS-CoV-2 infection. The PCR test is performed 72 h prior to scheduled surgery or immediately before surgery in the case of urgent surgery.
To determine the COVID-19 positivity rate, we evaluated all patients who underwent a scheduled or urgent surgical procedure during the study period. Using hospital records, we identified patients who underwent urgent or scheduled surgery and who had a PCR test for SARS-CoV-2 in the 72 h prior to surgery (target population). The microbiological results of the PCR tests were reviewed, and based on the result, the patients were classified as infected or not infected by SARS-CoV-2. Patients with a positive PCR result for SARS-CoV-2 were surveyed by telephone in order to obtain the necessary information to determine the presence of symptoms compatible with the disease and known risk factors. The questionnaire collected data on possible sources of infection and characteristics of the subjects and specifically registered all the information necessary to detect AC (without clinical criteria for COVID-19 infection). According to the WHO definition of a suspected case17, individuals were classified as symptomatic if they presented fever or acute respiratory symptoms at any time during the previous 14 days. In the absence of either, the subject was considered asymptomatic. Likewise, the medical files of patients with positive PCR for SARS-CoV-2 were reviewed to rule out any previously confirmed clinical diagnosis of COVID-19.
Statistical analysisThe prevalence of asymptomatic COVID-19 carriers was calculated in patients who had undergone scheduled or urgent surgery, according to laboratory results (PCR), for each of the study weeks and by hospital groups according to the number of beds. Prevalence was expressed as a percentage with its corresponding 95% confidence interval. The results were expressed as mean and standard deviation for continuous variables, and as frequency and percentage for qualitative variables. To study the possible relationship between qualitative variables, the Pearson chi-squared test or Fisher’s exact test was used, while the Student’s t-test was used to study the relationship between a quantitative variable and a dichotomous qualitative variable. To analyze the evolution of AC prevalence throughout the 6 weeks of the study, the Mantel-Haenszel linear trend test was used. P values <.05 were considered statistically significant. The statistical study was performed with the SPSS 20.0 statistical package (IBM Corp, Armonk, NY) and R version 3.6.8 (R Foundation for Statistical Computing).
ResultsA total of 10 838 patients scheduled for surgery or requiring urgent surgery were screened for COVID-19. Table 1 shows the number of PCR performed, listed by hospital groups. In total, 118 patients (1.09%) were positive for SARS-CoV-2 in the 72 h prior to surgery. Among them, 66.1% (78/118) had no symptoms in the 14 days prior to screening, so the prevalence of AC between April 20 and May 31, 2020 was 0.7% (95% CI: 0.6%–0.9%). A downward trend in the prevalence of AC was observed between the first week and the sixth week of the study (P < .001). Thus, the highest prevalence of AC was in the first week (1.9% [95% CI: 1.1%–3.2%]), while the lowest was in the sixth week [0.4% (95% CI: 0.2%–0.7%)] (Fig. 1). The prevalence of AC appears in Fig. 2 by hospital groups, according to the number of beds.
SARS-CoV-2 PCR tests performed per week in each hospital group according to number of beds.
| Hospital groups by n of hospital beds | N of hospitals | April 20–April 26 | April 27–May 10 | May 4–May 10 | May 11–May 17 | May 18–May 24 | May 25–May 31 | Total |
|---|---|---|---|---|---|---|---|---|
| PCR done | PCR done | PCR done | PCR done | PCR done | PCR done | PCR done | ||
| n = 730 | n = 883 | n = 1347 | n = 2108 | n = 2721 | n = 3049 | n = 10 838 | ||
| <200 beds | 5 | 59 | 104 | 179 | 295 | 352 | 338 | 1327 |
| 200–500 beds | 9 | 411 | 494 | 776 | 1279 | 1635 | 1825 | 6410 |
| 500–1000 beds | 2 | 111 | 144 | 154 | 237 | 352 | 401 | 1399 |
| >1000 beds | 1 | 149 | 151 | 238 | 297 | 382 | 485 | 1702 |
Regarding patients with positive PCR, the prevalence of patients with symptoms compatible with COVID-19 was 0.4% (95%CI: 0.3%–0.5%). Among the 40 symptomatic cases, 19 (47.5%) had changes in the radiographic images consistent with pneumonia, and fever and cough were the most frequent symptoms. Two patients died during the study period. 45% of symptomatic patients underwent urgent surgery, compared to 50% of AC (P = .6). Meanwhile, 32.5% of symptomatic patients had previous contact with a confirmed case, and 40% did not know the source of infection. The clinical characteristics of the symptomatic and asymptomatic patients with positive PCR test results appear in Table 2.
Clinical characteristics of asymptomatic and symptomatic patients with positive PCR result for SARS-CoV-2 (n = 118).
| Asymptomatic group (n = 78) | Symptomatic group (n = 40) | P | |
|---|---|---|---|
| Age (yrs), mean (SD) | 55 ± 23 | 58 ± 18 | 0.5 |
| Risk factors | |||
| Cardiovascular disease | 17 (21.8) | 9 (22.5) | 0.9 |
| Hypertension | 34 (43.6) | 15 (37.5) | 0.6 |
| Diabetes mellitus | 14 (17.9) | 9 (22.5) | 0.6 |
| COPD | 10 (12.8) | 3 (7.5) | 0.4 |
| Neoplasm | 19 (23.9) | 11 (27.5) | 0.6 |
| Immunosuppression | 7 (8.9) | 3 (7.5) | 0.8 |
| Pregnancy | 10 (12.8) | 9 (22.5) | 0.3 |
| Urgent surgery | 39 (50) | 18 (45) | 0.6 |
| Preoperative symptoms | |||
| Cough | 0 (0) | 21 (52.5) | <0.001 |
| Dyspnea | 0 (0) | 16 (40) | <0.001 |
| Fever | 0 (0) | 25 (62.5) | 0.001 |
| Anosmia | 0 (0) | 12 (30) | <0.001 |
| Ageusia | 0 (0) | 11 (27.5) | <0.001 |
| Nausea/vomiting | 0 (0) | 15 (37.5) | <0.001 |
| Throat pain | 0 (0) | 12 (30) | 0.001 |
| Shivering | 0 (0) | 9 (22.5) | 0.002 |
| Preoperative radiography result | 0.009* | ||
| Pathological | 8 (10.2) | 17 (42.5) | |
| Normal | 39 (50) | 11 (27.5) | |
| Not done | 31 (39.8) | 13 (32.5) | |
| Type of contact | 0.03* | ||
| Contact with confirmed case | 12 (15.4) | 13 (32.5) | |
| Contact with symptomatic person | 7 (9) | 11 (27.5) | |
| Unknown contact | 59 (75.6) | 16 (40) | |
| Mortality | 0 (0) | 2 (2.5) | |
Values expressed as frequencies (percentages) unless otherwise indicated.
SD: standard deviation; COPD: chronic obstructive pulmonary disease.
Using routine nasopharyngeal PCR testing before scheduled and urgent surgery, the results of our study indicate that the prevalence of asymptomatic SARS-CoV-2 carriers in the surgical population of Catalonia was 0.7% (95%CI: 0.6%–9%) during the 6-week period when surgical activity restarted after the initial peak of the pandemic in early April 2020. The rate of asymptomatic infections reported in different studies varies considerably, ranging between 0.13% and 41%4–9. Most of these studies were conducted in small population groups or were seroprevalence studies. As for other studies using preoperative PCR in the surgical population after the resumption of activity, Gruskay et al, in a study of 99 patients scheduled for trauma surgery, found 8% AC8, while Singer et al published a 0.13% preoperative AC rate in a single-center study that included 4751 patients7. To the best of our knowledge, this is the first multicenter study conducted in Spain of preoperative screening for SARS-CoV-2 infection before scheduled elective or urgent surgery.
Our results also show that 1.07% of patients had a positive preoperative PCR result for SARS-CoV-2, and 34.6% of these presented symptoms compatible with COVID-19. This indicates that 65.4% of the patients diagnosed with SARS-CoV-2 were asymptomatic at the time of the PCR, which implies that these patients could have undergone surgery while infected, which could be associated with a high risk of postoperative COVID-19–related complications. We must bear in mind that this is a period of time in which the use of PCR tests in Spain was limited by the scarce availability of these tests, which meant that they were used mainly in patients with acute respiratory symptoms and a high degree of clinical suspicion. Thus, patients who were scheduled for surgery or who underwent emergency surgery were one of the first population groups to be universally tested with PCR. Carrying out these tests in surgical patients allowed us to determine the prevalence of AC in this population group at a time when few data were available on the prevalence of AC in the general population. In this context, the identification of asymptomatic patients with a positive SARS-CoV-2 result is a critical point to control the spread of the disease, protect health workers, and maximize the care required by patients who undergo surgical procedures.
Furthermore, as Spain had already had 43 days of ‘state of alarm’ status and total confinement measures (except for essential workers) at the start of the study, the low prevalence of positive patients could indicate the effectiveness of the measures adopted to halt the spread of the pandemic. The downward trend in the prevalence of AC observed between the first and sixth week of the study would indicate that there was a drop in the population transmission of the virus, which was more accentuated as more time passed after the ‘state of alarm’ had been declared. All this indicates that the results of the PCR tests in patients who underwent surgery between April 20 and May 31, 2020, is very useful and could serve as a knowledge base in the event that similar restrictions were necessary due to the evolution of the pandemic.
When interpreting our data, we must consider the characteristics of our target population. Patients scheduled for surgery at the hospitals that participated in the study may inherently represent a population at lower risk of COVID-19 infection. This group of patients likely includes fewer subjects from nursing homes and community living facilities, where the known prevalence of COVID-19 is higher. Furthermore, patients awaiting surgical procedures can also practice stricter social distancing to avoid exposure to COVID-19 that could interfere with the scheduling of surgical procedures.
In addition, it is likely that the prevalence of AC obtained in our study may be underestimated since the sensitivity of PCR techniques is below 90%, and there may be false negative results18,19. However, it is considered the test of reference to diagnose SARS-CoV-2 infection. The rapid development of tests for SARS-CoV-2 has included the combination of genetic, antigen and serological tests. The first two are useful for the diagnosis of the disease in the acute phase or in the presymptomatic phase, while antibodies are not detected until 7-12 days after the onset of symptoms20. The better reliability achieved with the new rapid antigen tests compared to those that were marketed during the first wave of the pandemic opens up a possible future strategy for faster and more efficient preoperative screening.
In conclusion, our study found very low rates of asymptomatic carriers of COVID-19 infection (prevalence 0.7%) in the surgical population of hospitals in Catalonia. These results indicate that, during the study period, most patients were able to undergo surgical procedures without the perioperative risk of complications associated with COVID-19, and with a low probability of exposure for healthcare workers and other hospitalized patients. In the first wave of the pandemic, the scarce data available on AC due to the limited availability of PCR tests mean that the results obtained in this study can serve as a knowledge base in the context of new increases in COVID-19 incidence that once again require suspending surgical activity.
FundingThis present study has received no specific funding from public, commercial or non-profit organizations.
Conflicts of interestsNone.
The authors thank Dr Rosa M Villalonga Vadell and the Societat Catalana d’Anestesiologia, Reanimació i Terapèutica del Dolor (SCARTD) for their support of this study.
These authors contributed equally to the work.
Please cite this article as: de Miguel Negro M, González Tallada A, de Nadal M, Biarnes Suñé A, Manrique Muñoz S, Campins Martí M, et al. Prevalencia preoperatoria de portadores asintomáticos de COVID-19 en hospitales de Cataluña durante la primera ola tras el reinicio de la actividad quirúrgica. Cir Esp. 2022;100:352–358.