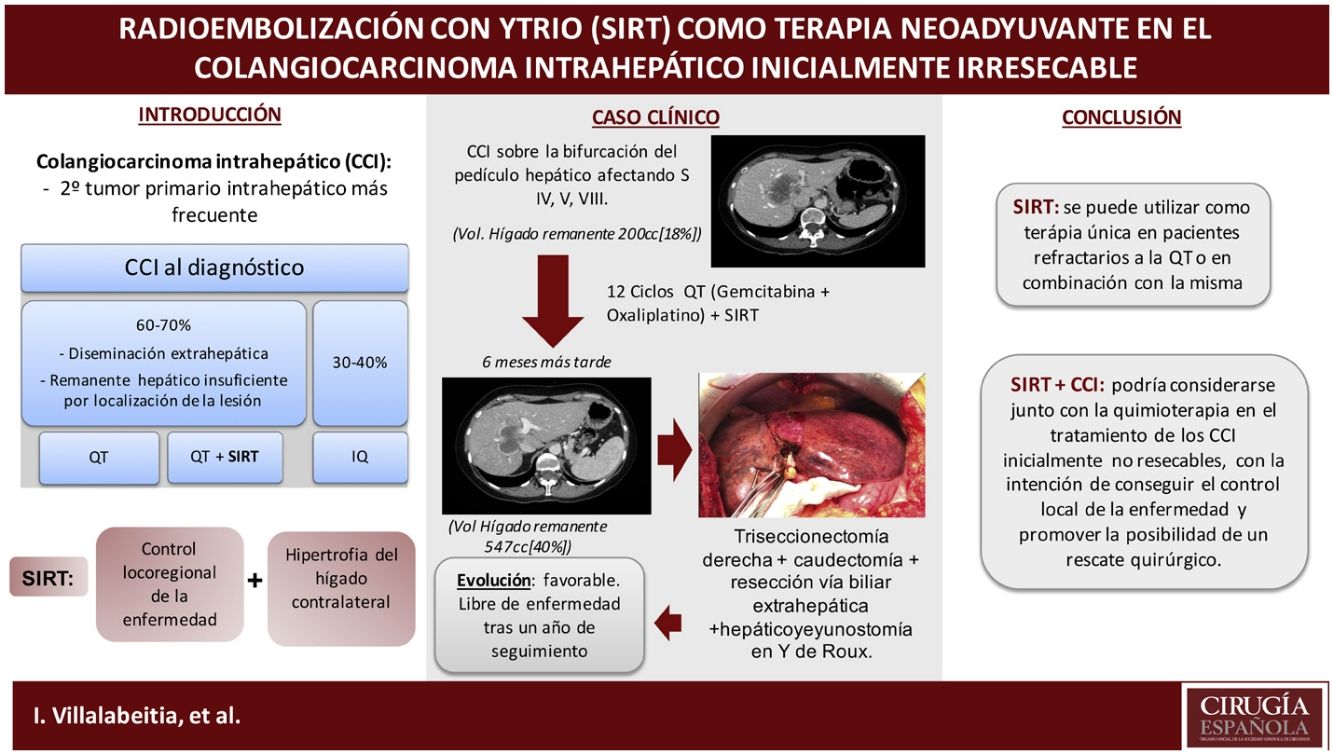
Intrahepatic cholangiocarcinoma (ICC) is the second most common primary liver tumour. Surgical resection is the only potentially curative treatment. However, 60%–70% of cases are not candidates for surgery at diagnosis, either because of disease dissemination or because the hepatic location does not leave sufficient remnant1,2. Although most of these cases are treated with chemotherapy (CT), radioembolization with yttrium microspheres, also known as selective internal radiation therapy (SIRT), has been proposed as a treatment that can salvage patients for surgery with curative intent; however, there is little published evidence on this indication2–4.
SIRT is an intra-arterial brachytherapy primarily used to treat hepatocarcinoma and hepatic metastases, however its use in ICC is not as widespread3,4. In addition to direct locoregional therapy to the tumour, SIRT can induce contralateral liver hypertrophy, allowing liver resection with curative intent in patients with previous insufficient liver remnant2.
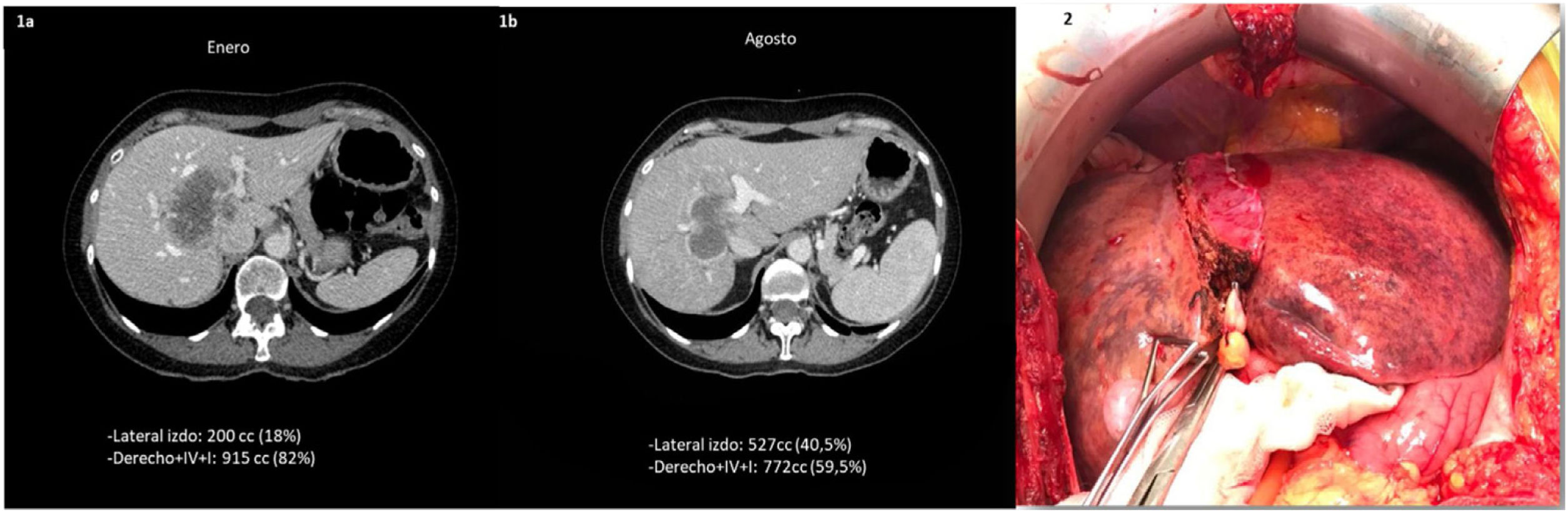
We present the case of a 55-year-old woman with no history of interest, histologically diagnosed with a 60 × 48 × 56 mm ICC located on the bifurcation of the hepatic pedicle, affecting segments IV, V, VIII and in direct contact with the middle hepatic vein without extrahepatic dissemination (Fig. 1a). Initially a right trisectionectomy was required, but the remaining liver (IBS-III) did not have sufficient residual volume (200 cm3 [18%]). Therefore, combined chemotherapy with gemcitabine-oxaliplatin and SIRT was given at two doses of .9 (80%) and .2 (20%) GBq via the right hepatic artery and an S4 branch, respectively. Six months after radioembolization and after 12 cycles of chemotherapy, there was slight decrease of the lesion and hypertrophy of the liver remnant of up to 527 cm3 (40%), representing a growth of 160% (Fig. 1b). The functionality of the future remnant liver was calculated by Tc99-mebrofenin SPECT scintigraphy, resulting in a De Graaf index of 2.1%/min/m2 and HIBA index of 20%. The patient had adequate liver function at all times, with normal bilirubin and liver enzyme values. In view of these findings, surgical resection was proposed.
(1) Progress after neoadjuvant treatment. (1a) Venous phase of initial CT scan, prior to treatment: large hypodense mass in central position in direct contact with the middle hepatic vein. (1b) Post-embolization CT scan: significant contralateral hypertrophy (S II–III). (2) Surgical intervention: right hepatic atrophy and contralateral hypertrophy, of segments II–III.
The operation was performed 339 days after diagnosis, revealing significant atrophy of the right liver and hypertrophy of the left lateral sector (Fig. 1.2). A right trisectionectomy with caudectomy and resection of the extrahepatic bile duct with lymphadenectomy was performed. Biliodigestive reconstruction was performed with a double Roux-en-Y hepaticojejunostomy. Portal pressures were taken at the beginning and end of the surgery, showing a gradient of 10 mmHg between the portal vein and the suprahepatic inferior vena cava, and therefore we decided not to act on portal flow. The definitive pathology report confirmed a poorly differentiated ICC (G3) with free margins without perineural or vascular infiltration (pT1bN0).
On the 8th postoperative day, with no test data of liver failure (Br 0.8, FA 120, GGT 990 GOT/GPT 75/38, TP 1.02), the patient developed ascites, and therefore a new pressure measurement was taken, showing a gradient of 13 mmHg between free and wedged hepatic vein. In view of these findings, a selective partial embolization of 60% of the splenic parenchyma was performed. After one year of follow-up, the patient is free of disease, and her tumour marker levels Ca 19.9, CEA and AFP remain within normal limits.
SIRT involves the controlled infusion of yttrium-loaded microspheres through the arteries supplying the tumours causing controlled tissue damage5. It can be used as a stand-alone therapy in CT-refractory patients or in combination with CT4. There is currently insufficient evidence to recommend initial SIRT versus CT + SIRT, they can be used concomitantly or even months after CT. In ICC, SIRT has been proposed as salvage treatment in patients initially not candidates for surgery, and achieves similar survival to patients treated with initial surgery2,5,6. This treatment, on the one hand, produces tumour necrosis, thus achieving local control of the disease in half of cases and even a reduction in tumour size in up to 36.4% of cases2. On the other hand, contralateral hypertrophy occurs, resulting in an increased liver remnant. In our case, because the remnant was insufficient, we decided to add SIRT to standard chemotherapy (CT) to achieve both benefits.
Several studies have identified low FDG avidity in tumours on PET/CT scan, adequate hepatic reserve, radiological response, and low tumour burden as potential prognostic factors for response to SIRT3–5. Although there is little published evidence in this field, several studies listed in Table 1 show the benefit of SIRT in the management of ICC.
Summary of published results of patients with ICC treated with neoadjuvant chemotherapy with yttrium and subsequent surgical resection.
| Publication | Type of tumour | Type of neoadjuvant chemotherapy | Patients with salvage surgery | Type of resection | Hypertrophy of liver remnant (%) | Months of follow-up | Recurrence |
|---|---|---|---|---|---|---|---|
| Vouche et al.7 | ICC | Gemcitabine ± Cisplatin | 1 | Right hepatectomy | 38 | ND | 1/1 |
| Rayar et al.8 | ICC | Gemcitabine + Platinum | 8 | Right hepatectomy 2 | 9 | 7.2 | 2/8 |
| Right Tri. 5 | |||||||
| Left Tri. 1 | |||||||
| Servajean et al.9 | ICC | GEMOX + FOLFIRINOX | 1 | Left hepatectomy | ND | 12 | 0/1 |
| Lewandowski et al.10 | ICC | No | 2 | Right hepatectomy | 30 | 20 | 1/2 |
| Gaba et al.a | ICC | No | 3 | Right hepatectomy | 36,3 | ND | 1/3 |
ICC: Intrahepatic cholangiocarcinoma; Left Tri.: Left trisectionectomy; ND: no data; Right Tri.: Right trisectionectomy.
In conclusion, SIRT could be considered in conjunction with CT in the treatment of an initially unresectable ICC, to achieve local control of the disease and offer the possibility of surgical salvage. However, prospective studies with long-term follow-up are needed.
Conflict of interestsThe authors have no conflict of interests to declare.