Management of patients diagnosed of acute uncomplicated diverticulitis has evolved lately and according to the latest guidelines, outpatient treatment and management without antibiotherapy may be used in selected patients. The aim of this study is to evaluate the adhesión among national centres to these and others recommendations related to this pathology.
MethodsAn online national survey, that has been broadcast by several applications, was performed. The results obtained were statistically analysed.
ResultsA total of 104 surgeons participated, representing 69 national hospitals. Of those, in 82.6% of the centres, outpatient management is performed for acute uncomplicated diverticulitis. 23.2% of the hospitals have a protocol stablished for treatment without antibiotherapy in selected patients. Centres that do not follow these protocols allege that the mean reasons are the logistic difficulties to set them up (49.3%) and the lack of current evidence for it (44.8%). Significative statistical differences have been found when comparing the establishment of such protocols between centres with advanced accredited units and those who are not, with higher rates of outpatient management and treatment without antibiotics in accredited units (p ≤ .05).
ConclusionsIn spite that this a very common disease, there is a huge national heterogeneity in its treatment. This is why it would adviseable to unify diagnostic and treatment criteria by the collaboration of scientific societies and the simplification of the development of hospitalary protocols.
El manejo de los pacientes diagnosticados de diverticulitis aguda no complicada ha evolucionado en los últimos años y según diversas guías clínicas internacionales actuales, el tratamiento ambulatorio y sin antibioterapia puede ser utilizado en pacientes seleccionados. El objetivo de este estudio es evaluar la adhesión de los distintos centros nacionales a estas y otras recomendaciones en esta patología.
MétodosSe realizó una encuesta online a nivel nacional que se dio a conocer a través de diversas aplicaciones informáticas y se analizaron estadísticamente los resultados obtenidos.
ResultadosParticiparon 104 cirujanos, representando 69 centros hospitalarios nacionales. En el 82,6% de los centros, se realiza manejo ambulatorio de los pacientes diagnosticados de diverticulitis aguda no complicada. El 23,2% de los centros tiene implantado un protocolo de tratamiento sin antibioterapia en pacientes seleccionados, mientras que en los centros que no siguen estas recomendaciones, las razones principales son las dificultades logísticas para su desarrollo (49,3%) y la ausencia de evidencia actual para ello (44,8%). Se han encontrado diferencias estadísticamente significativas al comparar la implantación de dichos protocolos entre centros con unidades acreditadas avanzadas y aquellas que no, con mayores tasas de manejo ambulatorio y sin antibioterapia en los centros acreditados avanzados (p ≤ 0,05).
ConclusionesA pesar de ser una patología muy frecuente, existe mucha heterogeneidad en su tratamiento a nivel nacional, por lo que sería recomendable la unificación de criterios diagnósticos y de tratamiento mediante la colaboración de las sociedades científicas y la simplificación de la puesta en marcha de protocolos hospitalarios.
Acute uncomplicated diverticulitis (AUD) is one of the most common acute abdominal pathologies in our environment.1–3 In 75% of diverticulitis cases, it is an uncomplicated condition that can be treated conservatively.4,5 Its treatment classically consisted of digestive rest, analgesia and oral or parenteral antibiotic therapy, recommending hospital admission.
For some years now, the pathophysiological basis of acute diverticulitis (AD) has been reconsidered, evolving from theories that defended the presence of diverticular microperforations, to those that defend that it could be an inflammatory disease.6 In 2007, the first observational study was published in which its treatment without antibiotic therapy was described,7 and since then the possibility of treating these patients with anti-inflammatories has been investigated, even on an outpatient basis, with six RCT8–13 in this regard existing to date. In all cases the results have been favourable, which is why the most recent clinical guidelines on the subject14,15 admit the possibility of foregoing antibiotic therapy in selected cases.
This management has proven to be safe in terms of the need for urgent admission, surgery or drainage, and has advantages such as avoiding the risk of developing multi-resistance, adverse effects of treatment or avoiding the extra economic cost that comes with the use of antibiotics. It is therefore of interest to determine the degree of implementation of this clinical practice at the national level and to know what difficulties they face in being able to carry out these changes.
Furthermore, there are other controversies in the follow-up and treatment of these patients in which the guidelines4,15 do not establish clear recommendations, such as the need for treatments to avoid recurrences or the systematic performance of an endoscopy after a first episode.
The objective of this study was to analyse the degree of implementation of treatment recommendations without antibiotic therapy in selected patients diagnosed with AUD at a national level, to evaluate what the limiting factors for their implementation were, and also to analyse other controversial aspects in this very common pathology.
Material and methodsStudy designTo achieve the objective, it was decided to carry out a national survey seeking the greatest representation, which would reflect the current situation, as faithfully as possible, of non-antibiotic treatment of AUD in Spain.
Assuming that this pathology is linked to colorectal surgery, the approach was to try to involve as much as possible the members of the Spanish Association of Coloproctology (AECP for its initials in Spanish), a scientific association that brings together surgeons with specific dedication to this field and whose purpose is to promote the advancement of science, knowledge and good clinical practice in coloproctology.
Within this association there is a working group that aims to encourage academic and teaching actions among its youngest members, under 45 years of age, known as the AECP Young Group (GJ-AECP). For this reason, this was considered an ideal forum to carry out the work and disseminate the survey developed.
This study was registered in ClinicalTrials, with the identification code NCT05784064.
Creation and distribution of the surveyThe survey was developed by two of the authors (ACB and CCS) and supervised and validated by two others (GP and JGS). Its final version was developed using the Google Forms® platform.
Since this was a study in which volunteer professionals participated, it was deemed not to require the approval of a Local Ethics Committee for its implementation. Despite the voluntary nature of participation in it, it was explicitly stated that the subjects who answered the survey granted their consent for the archiving, analysis and publication of the data resulting from their responses.
For the preparation of the project, the recommendations included in the checklist for the preparation of surveys carried out through the Internet or telematic methods (Checklist for Reporting Results of Internet E-Surveys—CHERRIES)16 were taken into account.
On December 14, 2022, the final version of the survey was launched through the WhatsApp® group made up of the 134 members of the GJ-AECP, representing 80 hospitals in Spain. Within this group, 30 of the 36 colorectal surgery units accredited as advanced by the AECP were represented.
When consulting the list of centres reached via WhatsApp®, we reviewed whether there was any representative centre at the level of colorectal surgery that could be left out, and in these cases the invitation was sent directly to a representative of the said centre. Additionally, mobilised through different social networks (Twitter®, Whatsapp®), extending it to surgeons outside the GJ-AECP, without being able to determine how many distributions there were exactly through both social networks.
Monthly reminders were sent during the first two months and in the last month reminders were sent 30 days, 15 days, 7 days and 2 days before its final closure. The survey was open until May 30, 2023.
In order to participate in the survey, respondents were asked, after reading and accepting an informed consent regarding the use of their data, to complete their personal information and the initials of their name. The survey contained 44 questions regarding personal data, the type of hospital they worked in, the diagnosis of the pathology, the treatment and the follow-up (Appendix A). The estimated time to complete it was 7−10 min.
In cases where there were discrepancies in the answers between members of the same centre, the most frequent answer among them was chosen.
Statistical methodCategorical variables were analysed using frequencies and percentages. Continuous quantitative variables with a normal distribution were analysed using means and standard deviation (SD), those with a non-normal distribution were analysed using medians and interquartile ranges. The statistical programme IBM SPSS Statistics® version 24.0 (IBM, Armonk, New York, USA) was used. The p value ≤.05 was considered significant.
ResultsOne hundred and four surgeons agreed to respond to the survey, representing 69 national hospital centres. Of the centres represented, 68.1% had members representing the GJ-AECP.
Seventy-nine point six per cent of those surveyed belonged to a colorectal surgery unit and 8.7% were residents.
Of the 30 units accredited as advanced represented in the GJ-AECP, members of at least 23 of them responded to the survey. This means that 63.9% of the accredited colorectal surgery units in our country were represented and answered the survey. The characteristics of the centres that participated are shown in Table 1.
Characteristics of the centres represented in the survey.
| N = 69 (%) | ||
|---|---|---|
| Type of hospital | Tertiary level public university hospital | 33 (47.8) |
| Tertiary level public non-university hospital | 1 (1.4) | |
| Tertiary level private university hospital | 3 (4.3) | |
| Second level public university hospital | 22 (31.9) | |
| Second level public non-university hospital | 8 (11.6) | |
| Second level private hospital | 2 (2.9) | |
| Number of beds | <200 beds | 11 (15.9) |
| 200−500 beds | 29 (42.0) | |
| >500 beds | 29 (42.0) | |
| Monthly number of acute diverticulitis cases | <5 case | 9 (13.0) |
| 5−10 cases | 24 (34.8) | |
| >10 cases | 36 (52.2) | |
| Accredited unit | There is no unit | 11 (15.9) |
| Unit without accreditation | 31 (44.9) | |
| Unit with basic accreditation | 4 (5.8) | |
| Unit with advanced accreditation | 23 (33.3) | |
In 94.3% of the centres, the service responsible for the treatment of these patients is General Surgery, while the Digestive and Emergency services are responsible for 4.3% and 1.4%, respectively.
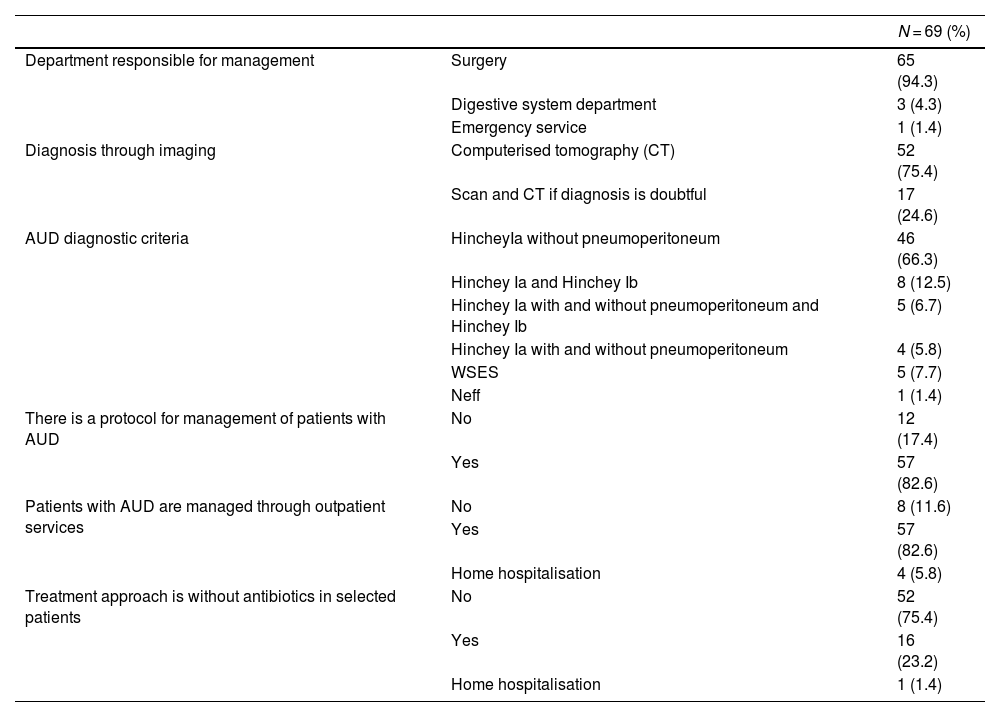
Regarding the definition of AUD, 66.3% agreed on the diagnosis of patients with Hinchey Ia without pneumoperitoneum, while 12.5% defined it as those patients with a diagnosis of Hinchey Ia and Ib. 6.7% define AUD as those with HincheyIa symptoms with and without pneumoperitoneum and Hinchey Ib; 5.8% accept the Hinchey Ia tables with and without pneumoperitoneum and 7.7% do not use the Hinchey classification, but rather that of the World Society of Emergency Surgery (WSES), and 1% that of Neff. (Table 2)
Diagnosis and management of patients with AUD.
| N = 69 (%) | ||
|---|---|---|
| Department responsible for management | Surgery | 65 (94.3) |
| Digestive system department | 3 (4.3) | |
| Emergency service | 1 (1.4) | |
| Diagnosis through imaging | Computerised tomography (CT) | 52 (75.4) |
| Scan and CT if diagnosis is doubtful | 17 (24.6) | |
| AUD diagnostic criteria | HincheyIa without pneumoperitoneum | 46 (66.3) |
| Hinchey Ia and Hinchey Ib | 8 (12.5) | |
| Hinchey Ia with and without pneumoperitoneum and Hinchey Ib | 5 (6.7) | |
| Hinchey Ia with and without pneumoperitoneum | 4 (5.8) | |
| WSES | 5 (7.7) | |
| Neff | 1 (1.4) | |
| There is a protocol for management of patients with AUD | No | 12 (17.4) |
| Yes | 57 (82.6) | |
| Patients with AUD are managed through outpatient services | No | 8 (11.6) |
| Yes | 57 (82.6) | |
| Home hospitalisation | 4 (5.8) | |
| Treatment approach is without antibiotics in selected patients | No | 52 (75.4) |
| Yes | 16 (23.2) | |
| Home hospitalisation | 1 (1.4) | |
In 82.6% of the centres there is a protocol for the treatment of these patients and in the same percentage of centres, this is carried out on an outpatient basis, with 5.8% of centres carrying out home hospitalisation (Table 2).
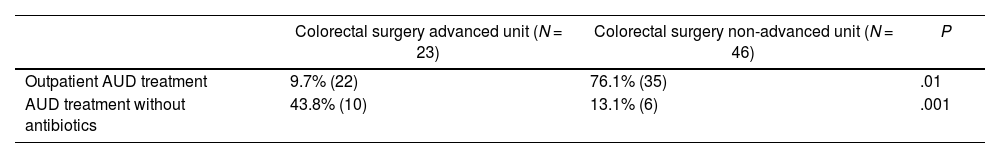
In 16 of the 69 centres (23.2%), treatment without antibiotic therapy is performed in selected cases of AUD. (Table 2). Statistically significant differences have been found when comparing the rates of implementation of outpatient treatment protocols between centres with advanced units and those without (95.7% vs. 76.1%, p = .01) and in the rates of treatment protocols without antibiotic therapy (43.8% vs. 13.1%, p = .001). (Table 3)
Among the respondents who stated that treatment without antibiotic therapy is not applied in their centre, 49.3% (N = 33) allege logistical problems for its development, while 44.8% (N = 30) affirm that there is no enough current evidence to put it into practice at this time.
83.1% make dietary recommendation on discharge, with most combinations being a liquid diet for the first few hours followed by a low-residue diet (67.8%).
65.7% of respondents recommended drugs to prevent recurrence, with 67.4% rifaximin monotherapy, followed by 10.9% combinations of rifaximin and probiotics. 10.8% use mesalazine alone or in combination, while 6.5% recommend the use of oral fibre alone or in combination.
55.9% of the participants performed a systematic colonoscopy after a first episode of AUD and 39.7%, depending on the age of the patient. This colonoscopy is performed in 70.1% of cases between the first and third month after the episode.
DiscussionIt was observed that less than 25% of the centres represented carry out treatment without antibiotic therapy in patients diagnosed with AUD, one of the main reasons being the lack of current evidence. This result is striking, given that in recent years four randomized clinical trials,8–13 and several meta-analyses17,18 have been published that demonstrate that this treatment in selected patients is safe, without higher rates of complications or the need for surgery or urgent percutaneous drainage. In fact, since the European guidelines published in 20181,5 it is recommended to avoid the use of antibiotic therapy in cases of AUD in selected patients.
A large part of those surveyed affirm that the main problem they face in implementing treatment protocols without antibiotic therapy are the logistical aspects. We should try to reflect on what the problems they refer to may be, given that most of them have hospital protocols for the treatment of this pathology that can be updated to include the updates proposed by the clinical guidelines. Perhaps the difficulty in establishing a clinical change among the professionals themselves is being attributed to logistical problems because it is an attitude that has been established for decades. It is possible that, thanks to the publication of the results and protocols carried out by various multidisciplinary teams, this obstacle to progress in routine clinical practice could be improved.19
Regarding the outpatient management of these patients, a non-negligible percentage of centres continue to systematically hospitalise those diagnosed with AUD. This data is striking, since, as in treatment without antibiotic therapy, the evidence that exists in favour of performing outpatient treatment is very extensive, both in terms of safety due to the absence of major complications,20,21 and in terms of healthcare costs and nosocomial complications associated with admission,20–22 even in elderly patients.23
In many cases, it is probably due to the weight of tradition and problems in developing innovative projects in some surgical services or to the intrinsic difficulties of each hospital in implementing new clinical protocols, which could benefit from research activity of societies such as the GJ-AECP or by the publication of monographs such as that carried out by the Spanish Association of Surgeons.24 The positioning of these scientific associations should be aimed at convincing their surgeons of better clinical practice, knowing the situation and the resistance to change shown in this survey.
It is striking that among centres with colorectal surgery units accredited as advanced, the implementation of outpatient treatment protocols or without antibiotic therapy is greater than in centres without this accreditation. These figures could be related to the fact that, upon being evaluated by an external agent, these units have carried out an internal audit exercise to improve the monitoring of new protocols such as the one mentioned.
Other points in which there is heterogeneity among the respondents are dietary recommendations and the performance of control endoscopies after an episode of AUD.
Regarding the use of drugs to prevent recurrences and intercurrent symptoms, just over half of those surveyed use them regularly, with results in line with usual recommendations. In general, the use of rifaximin has been shown to improve intercurrent symptoms, alone or in association with soluble oral fibre, while mesalazine has not presented such good results.25–27
Another of the great controversies is the need for systematic colonoscopy after an episode of AUD, and it has been discussed on numerous occasions, with disparate trends. The rates of colorectal cancer in patients with AUD range between 3.5% and 1.2%,28 so we cannot rule out its performance, even in extreme age groups (<50 years and >80 years), where there are series that have shown rates around 8.7% and 24% of the colonoscopies performed, respectively.29
With the results obtained, we can conclude that there are points to be resolved regarding the management of patients with AUD, the implementation of protocols being of vital importance, in which the inclusion criteria of patients, both radiological and clinical, are well defined.
With the existing evidence to avoid the use of antibiotics in selected cases of AUD, the low proportion of hospitals in which it is used is striking. This forces scientific societies and health institutions to decide whether transformation in this sense represents value and to try to provide strategies that guarantee safe change.
The main limitations of the study would be its sample size, which could be larger, and the difficulty in evaluating points such as the selection criteria for patients treated with and without antibiotic therapy. Furthermore, since it is an individual survey, we can find some variability between the responses of members of the same hospital centre, so these data have been taken into account when carrying out the analysis. Although participation could have been higher, there is a representation of 63.9% of colorectal surgery units accredited as advanced.30
In light of the results, we consider that a unification of criteria and standardisation of recommendations for patients diagnosed with AUD would be advisable, for which the collaboration of institutions, the positioning of scientific societies and the simplification of the implementation of protocols by hospital centres would be necessary.
This is the first study in Spain that has been developed to evaluate the level of implementation of treatment without antibiotic therapy in AUD, a topic that is as common as it is heterogeneous and that has been constantly changing in recent years thanks to new research in this regard. Our work offers a realistic snapshot of trends in routine clinical practice that can help us identify the main points of controversy at the current time.
FundingNone.
Conflict of interestsNone.
It is declared that no type of funding was received for the preparation of this study and there is no conflict of interest. No experiments with animals and/or humans were carried out for its execution and the patient signed the informed consent, agreeing with the publication of this manuscript, it being necessary to access their clinical history following the protocols of clinical ethics and confidentiality established for it. The signing authors have read and approved the manuscript, meeting its authorship requirements.
The authors Alba Correa Bonito and Carlos Cerdán Santacruz contributed equally to the preparation of this manuscript.
Dr. Manuel González Bermúdez, Complejo Hospitalario Universitario de A Coruña (A Coruña); Dr. Yousef Allaoua, Hospital Universitario Príncipe de Asturias (Alcalá de Henares, Madrid); Dra. María Carmona Agúndez, Dra. Isabel M Gallarín Salamanca, Dra. Beatriz Martín Pérez, Hospital Universitario de Badajoz (Badajoz); Dra. Marta Jiménez Toscano, Dra. Silvia Salvans, Hospital del Mar (Barcelona); Dra. Romina Pena López, Hospital Clinic (Barcelona); Dra. Ana Centeno Álvarez, Consorci Sanitari Integral (Barcelona); Dra. Ruth Blanco Colino, Dr. Franco Marinello, Hospital Vall d´Hebrón (Barcelona); Dra. Laura Sobrerroca Porras, Hospital Sant Joan Despí Moisés Broggi (Barcelona); Dra. Ana Roberta Gálvez Saldaña, Hospital de Bellvitge (Barcelona); Dra. Montserrat Guasch Marcé, Parc Sanitari Sant Joan de Deu (Barcelona); Dr. Gonzalo P. Martín-Martín, Centro Médico Teknon (Barcelona); Dr. José Granados García, Hospital Infanta Margarita (Cabra, Córdoba); Dra. Tatiana Gómez Sánchez, Dr. Javier Varela Recio, Hospital Puerta del Mar (Cádiz); Dr. Gonzalo Gómez Dueñas, Dr. Francisco Javier Medina Fernández, Hospital Universitario Reina Sofía (Córdoba); Dr. Juan Gabriel Tejerina Riera, Hospital del Henares (Coslada, Madrid); Dr. Luis Miguel Estela Villa, Dr. Pedro Benjamín Ramos Martín, Hospital Virgen de La Luz (Cuenca); Dra. Cristina Lillo García, Dr. Luis Sánchez-Guillén, Dra. Mónica Serrano Navidad, Hospital General Universitario de Elche (Elche, Alicante); Dra. Tamara Fernández Miguel, Hospital Galdakao-Usansolo (Galdakao, Bilbao); Dra. Marta González Bocanegra, Dra. Ainhoa Valle Rubio, Hospital Universitario de Getafe (Getafe, Madrid); Dr. Carlos Álvarez Laso, Dra. María Desirée Díaz González, Dra. Helena Padín Álvarez, Hospital Universitario de Cabueñes (Gijón); Dra. Nuria Ortega Torrecilla, Hospital Universitario Doctor Josep Trueta (Girona); Dr. Alberto Carrillo Acosta, Hospital Universitario Virgen de Las Nieves (Granada); Dra. Mireia Amillo Zaragüeta, Hospital de Granollers (Granollers, Barcelona); Dra. Mireia Merichal Resina, Hospital Universitari d´Igualada (Igualada, Lleida); Dra. Elsa Castelo Álvarez, Hospital de Jarrio (Jarrio, Asturias); Dr. Javier Rivera Castellano, Hospital Universitario de Canarias (La Laguna); Dra. Maria del Mar Camaces de Arriba, Hospital Valle del Nalón (Langreo, Asturias); Dra. Cristina Gas Ruiz, Hospital Universitario Arnau de Vilanova (Lleida); Dr. Antonio Navarro-Sánchez, Complejo Hospitalario Universitario Insular Materno-Infantil (Las Palmas de Gran Canaria); Dr. Antonio Ramos Bonilla, Hospital Severo Ochoa (Leganés, Madrid); Dr. Johnn Henry Herrera Kok, Complejo Asistencial Universitario de León (León); Dra. Lara Blanco Terés, Dr. Carlos Cerdán Santacruz, Dra. Ángela de la Hoz Rodríguez, Dra. Cristina Marín Campos, Hospital Universitario de La Princesa (Madrid); Dr. Javier Tomás Morales Bernaldo de Quirós, Hospital Central de La Defensa (Madrid); Dra. Nuria Chavarrías Torija, Hospital Universitario de La Paz (Madrid); Dr. Juan Ocaña Jiménez, Hospital Universitario Ramón y Cajal (Madrid); Dra. Elena Viejo Martínez, Hospital Infanta Leonor (Madrid); Dr. Alfredo Vivas López, Hospital Universitario Doce de Octubre (Madrid); Dra. Paula Dujovne Lindenbaum, Dr. Álvaro Landeras López, Dra. Yeniffer Tatiana Moreno Salazar, Dra. Patricia Tejedor Togores, Hospital Universitario Gregorio Marañón (Madrid); Dra. Patricia Sáez Carlín, Hospital Sanitas Moraleja (Madrid); Dra. Marta Roldón Golet, Quirón Salud Málaga (Málaga); Dra. Natalia Alonso Hernández, Dr. Sebastián JeriMcFarlane, Hospital Universitario Son Espases (Mallorca); Dra. Ángeles Pérez Aisa, Hospital Costa del Sol (Marbella, Málaga); Dra. Rocío Santos Rancaño, Hospital Comarcal de Melilla (Melilla); Dra. Ana Muñoz Rivas, Dr. César Levano-Linares, Hospital Rey Juan Carlos (Móstoles, Madrid); Dr. Emilio Peña Ros, Hospital Universitario Reina Sofía (Murcia); Dr. Jesús Abrisqueta Carrión, Hospital Universitario Virgen de La Arrixaca (Murcia); Dra. Inés Aldrey Cao, Complexo Hospitalario Universitario de Ourense (Ourense); Dra. María Fernández-Hevia, Dr. Daniel Fernández Martínez, Dr. Luis García Flórez, Dra. Giana Pamela Ibero Casadiego, Hospital Universitario Central de Asturias (Oviedo, Asturias); Dr. Jorge Arredondo Chaves, Clínica Universidad de Navarra (Pamplona, Navarra); Dr. Gabriel Marín, Hospital Universitario de Navarra (Pamplona, Navarra); Dra. Rocío Maqueda González, Dra. Elena Sagarra Cebolla, Hospital Infanta Cristina (Parla, Madrid); Dr. Jonás García Fernández, Hospital del Oriente de Asturias (Parres, Asturias); Dra. Marina Alarcón Iranzo, Hospital de Sagunto (Sagunto, Valencia); Dr. Francisco Blanco Antona, Hospital Universitario de Salamanca (Salamanca); Dr. Álvaro Gancedo Quintana, Hospital Universitario Infanta Sofía (San Sebastián de los Reyes, Madrid); Dr. Jorge Abellán Fernández, Hospital Universitario Nuestra Señora de La Candelaria (Santa Cruz de Tenerife); Dra. Natalia Suárez Pazos, Hospital Universitario Marqués de Valdecilla (Santander) Dra. María Luisa Reyes Díaz, Dr. Luis Tallón-Aguilar, Hospital Universitario Virgen del Rocío (Sevilla); Dra. Laura Arriero Ollero, Dra. Teresa Calderón Duque, Dra. Lourdes Gómez Ruíz, Hospital Nuestra Señora del Prado (Talavera de la Reina, Toledo); Dr. Sixto Javier Genzor Ríos, Hospital Reina Sofía (Tudela, Navarra); Dra. Leticia Pérez Santiago, Hospital Clínico Universitario de Valencia (Valencia); Dr. Antonio Melero Abellán, Consorcio Hospital General Universitario (Valencia); Dra. Mónica Millán Scheiding, Hospital Universitari i Politecnic La Fe (Valencia); Dr. Óscar Cano-Valderrama, Dr. Erene Flores Rodríguez, Dr. Enrique Moncada Iribarren, Dr. Alberto de San Ildefonso Pereira, Dr. Vincenzo Vigorita, Hospital Universitario Álvaro Cunqueiro (Vigo, Pontevedra); Dr. Gerardo Rodríguez León, Hospital de Viladecans (Viladecans, Barcelona); Dra. Andrea Jiménez Salido, Hospital Comarcal Alt Penedés (Vilafranca del Penedés, Barcelona); Dr. Norman Cervantes Juárez, Hospital General de Villarrobledo (Villarrobledo, Albacete); Dra. Teresa Pérez Pérez, Hospital Lluís Alcanyis de Xátiva (Xátiva, Valencia); Dra. Nieves Sánchez Fuentes, Hospital Universitario Miguel Servet (Zaragoza).