The spread of the SARS-CoV-2 infection (COVID-19) has required adaptation by hospitals affected by the pandemic, which has caused a reduction in elective surgical activity.
MethodsRetrospective study of patients operated on in the previous month and during the peak of the pandemic. We analysed the COVID-19 infection rate, the severity of respiratory infection according to the Brescia respiratory COVID-19 severity scale, the adopted therapeutic measures and the overall postoperative complications.
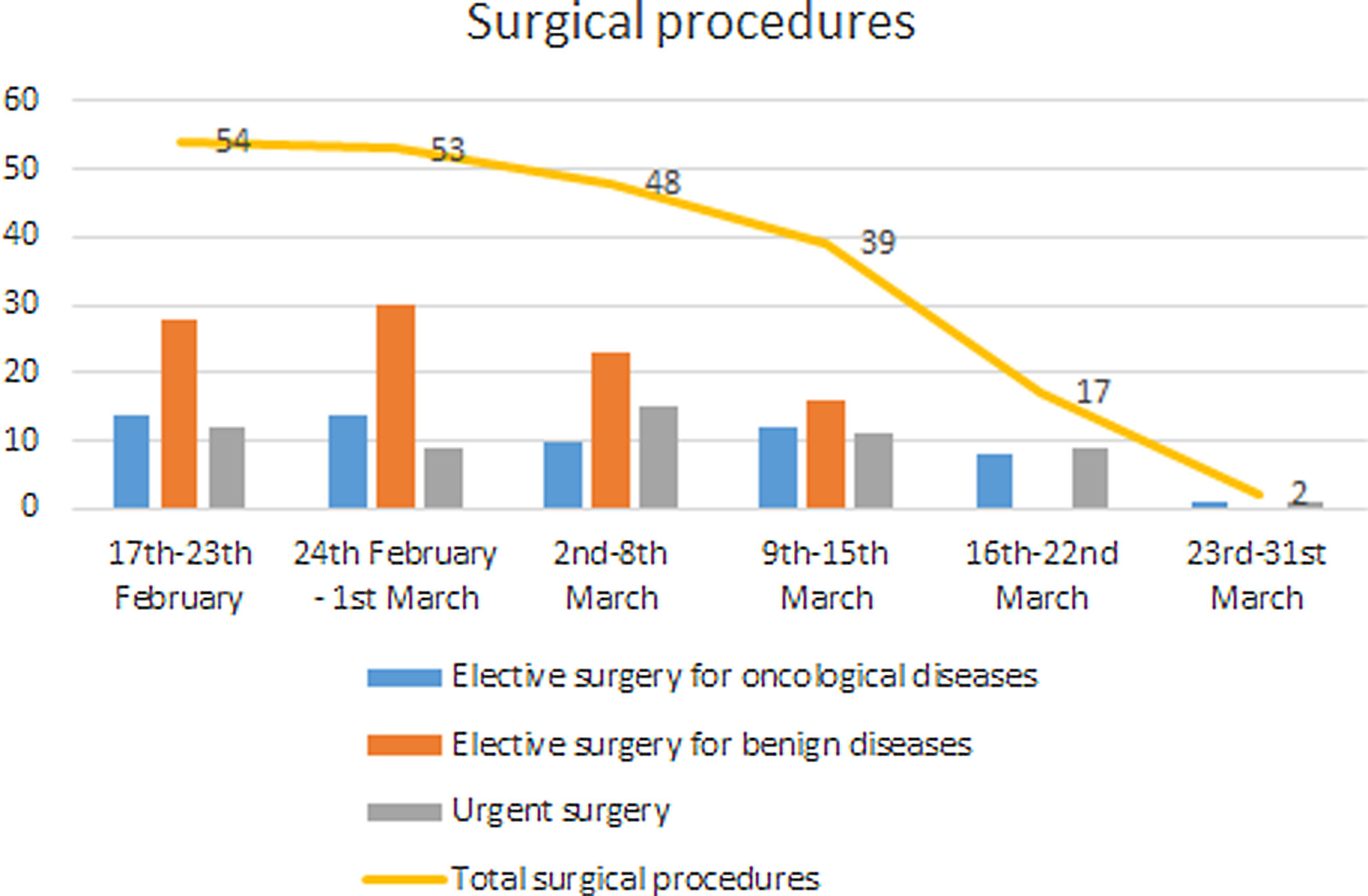
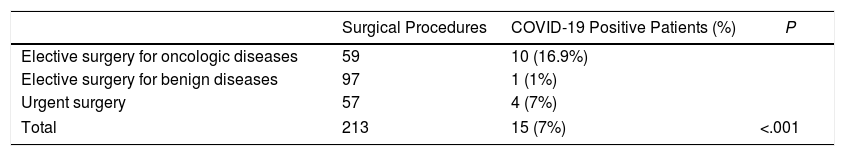
ResultsFrom 17th February to 31st March 2020, there was a progressive decrease in surgical activity, with only 213 patients operated on. This comprised 59 (27.8%) elective operations for oncological diseases, 97 (45.5%) elective operations for benign diseases and 57 (26.7%) as urgent procedures.
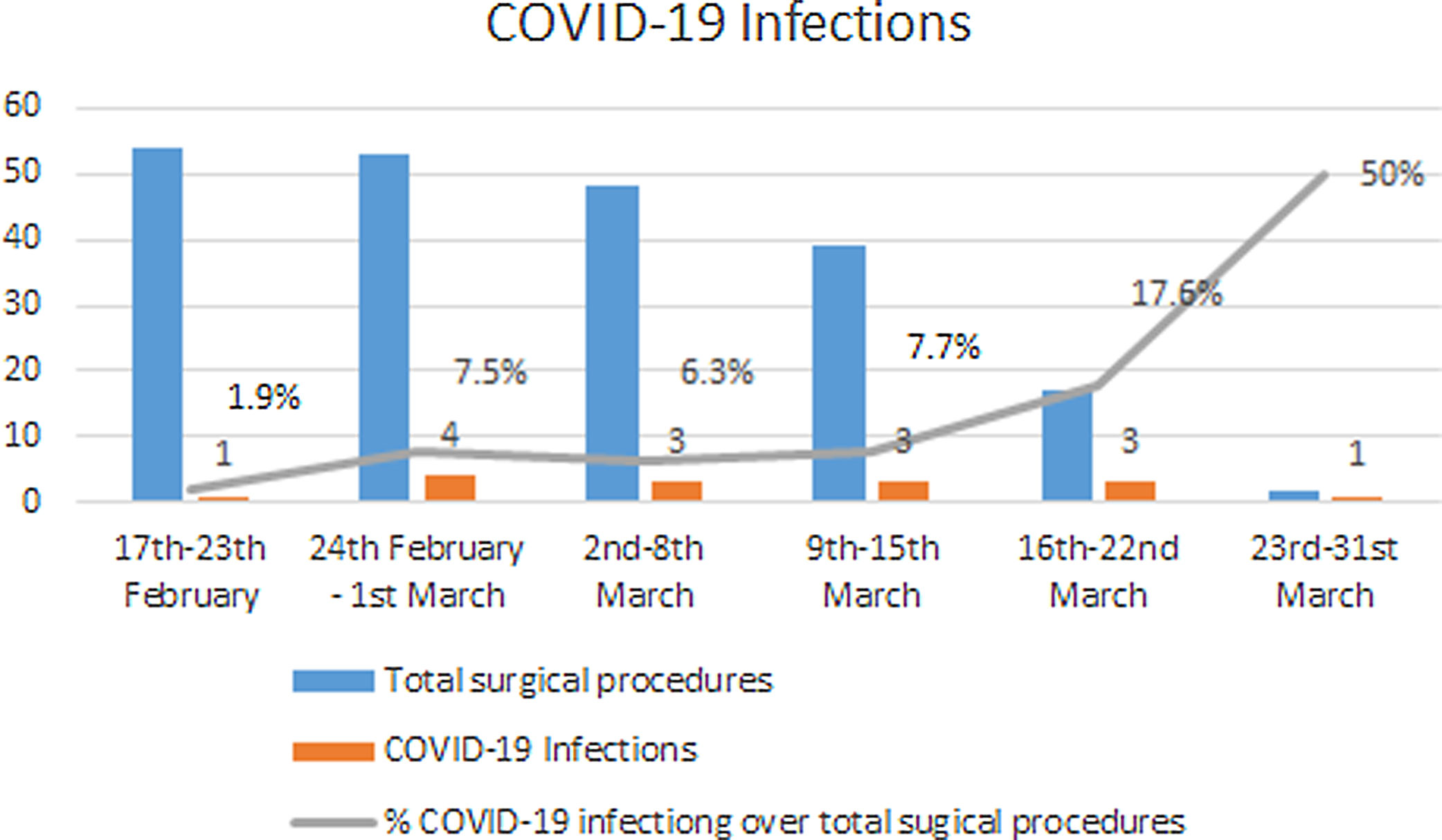
There was a progressive increase in the rate of infection by COVID-19, with a total of 15 cases (7%). This included 10 patients (16.9%) in the elective group for oncological disease, 1 (1%) in the elective surgery group for benign disease and 4 (7%) in the urgent surgery group (P<.001). Five patients presented with a severe respiratory infection, of which 4 were affected by oncological disease. There were 3 deaths (1.4%), which were all due to the worsening of a respiratory infection.
ConclusionsThe patients undergoing the surgical procedures showed high rates of COVID-19 infection and postoperative complications, especially the patients with oncological diseases. Local resumption of surgical activity must be based on the prioritisation of the cases to be operated on, respecting certain premises of security and optimisation of the available resources.
La expansión de la infección por SARS-CoV-2 (COVID-19) ha requerido la adaptación de los hospitales afectados por la pandemia, causando una reducción de la actividad quirúrgica electiva.
MétodosEstudio retrospectivo de pacientes operados durante el mes previo y el pico de la pandemia. Se analizó la tasa de contagio por COVID-19, la gravedad de la infección respiratoria según la Brescia Respiratory COVID-19 Severity Scale, las medidas terapéuticas adoptadas y las complicaciones postoperatorias globales.
ResultadosDesde el 17 de febrero hasta el 31 de marzo de 2020 se produjo una reducción progresiva de la actividad quirúrgica, interviniéndose únicamente 213 pacientes: 59 (27,8%) de forma programada por patología tumoral, 97 (45,5%) por patología benigna y 57 (26,7%) de forma urgente.
Se produjo un aumento progresivo de la tasa de contagio por COVID-19 con un total de 15 (7%) casos. De los pacientes oncológicos, 10 (16,9%) resultaron afectos; en el grupo de cirugía electiva, un paciente (1%); y en el grupo de cirugía urgente, 4 (7%) (p<0,001). Cinco pacientes presentaron una infección respiratoria grave de los cuales 4 estaban afectos por enfermedad oncológica. Hubo 3 (1,4%) fallecimientos, todos debidos a progresión de la infección respiratoria.
ConclusionesLos pacientes sometidos a cirugía presentaron una elevada tasa de infección por COVID-19 y de complicaciones postoperatorias, sobre todo en los pacientes oncológicos. La puesta en marcha de la de la actividad quirúrgica debe basarse en una priorización de los casos a operar, respetando unas premisas de seguridad y optimización de los recursos disponibles.
Since the first cases of the SARS-CoV-2 (COVID-19) infection occurred in late December 2019 in Wuhan, China, the exponential growth of this disease has led to a pandemic, declared as such by the World Health Organization (WHO) on 11th March 2020.1,2 Spain, and specifically the community of Madrid, has been one of the areas with the highest rates of declared infections worldwide,3 which led to the declaration of a National State of Alarm on 14th March 2020.
The expansion of the infection and the high consumption of health resources, such as hospital beds and intensive care units (ICUs), have led to an adaptation of the health system.3,4 To try to serve as many patients as possible, in many centres, staff have been relocated, while the number of ICU beds has been expanded. All these logistical changes, together with the epidemic context, have led to the temporary reduction or suspension of elective surgical activity in many centres affected by the pandemic.5
The reduction or suspension of surgical activity has led to delays in the scheduling of interventions, which can represent a serious problem in the case of oncological diseases.6 Although treatment delays have clearly demonstrated a worsening of the oncological prognosis,7–9 the increase in morbidity and mortality in the patients submitted for surgical procedures, as described by European and Asian groups,6,10,11 cannot be ignored. Surgical stress seems to be associated with a change in the immune profile, which would favour SARS-CoV-2 infection and the severity of its clinical expression.12
At present, very little evidence and limited recommendations by scientific societies are available on the management of patients awaiting elective surgery.13 There are mainly recommendations for urgent/emergent surgery that assess the risk of the SARS-CoV-2 infection versus the benefit of treating the underlying disease.4,14–16
The objective of this study is to analyse the impact of the COVID-19 pandemic on patients undergoing surgical procedures in a general surgery department in a third-level public hospital in Spain that is part of the hospital network of the Madrid Health Service (SERMAS). Patients operated on from the month before the declaration of the national state of alarm in Spain and until the peak of the pandemic were studied. Based on the analysis of our results and a review of the available literature, we propose recommendations regarding the resumption of surgical activity in hospitals affected by the pandemic.
Material and MethodRetrospective analysis of patients undergoing surgical procedures in a third-level university hospital in Spain from 17th February (four weeks before the declaration of the national state of alarm) to 31st March 2020 with a minimum follow-up of 15 days.
The selected hospital is a public hospital that presented a progressive increase in COVID-19 cases and a progressive suspension of surgical activity until it reached a type V scenario, according to the definition of the Spanish Association of Surgeons (AEC).17 This situation implies a percentage of COVID-19 patients hospitalised >75% of total hospitalisations and a significant impact on clinical care activity with limited beds in the ICU. After reaching the type V scenario, coinciding with the declaration of the national state of alarm on the 14th of March 2020, elective surgical activity was almost completely suspended.
For confirmation of the suspected cases of SARS-CoV-2-infected patients with suspicious symptoms, the reverse transcriptase-polymerase chain reaction (RT-PCR) test was used, according to the methodology available in the hospital's microbiology laboratory, using nasopharyngeal and oropharyngeal exudates. Radiological signs compatible with COVID-19 were considered to be the appearance of ground glass peripheral opacity, a diffuse alveolar pattern, bilateral opacities and/or organised pneumonia.18
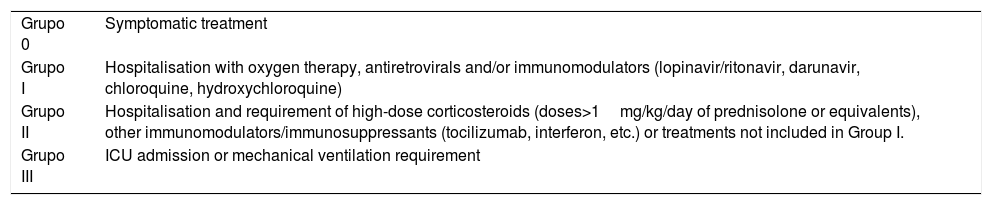
During the peak of the pandemic, it became necessary to prioritise the available resources based on a series of clinical–ethical–epidemiological criteria dictated by the competent local authorities. Therefore, when reporting the morbidity and mortality of surgical patients with the COVID-19 infection, the severity of complications will be indicated according to the Dindo–Clavien classification19; the therapeutic measures used with each patient according to a classification of treatments required (as described in Table 1) and the severity of the respiratory infection according to the Brescia respiratory COVID-19 severity scale (BRCSS).20
Treatment Groups in Relation to COVID-19 Infection.
| Grupo 0 | Symptomatic treatment |
| Grupo I | Hospitalisation with oxygen therapy, antiretrovirals and/or immunomodulators (lopinavir/ritonavir, darunavir, chloroquine, hydroxychloroquine) |
| Grupo II | Hospitalisation and requirement of high-dose corticosteroids (doses>1mg/kg/day of prednisolone or equivalents), other immunomodulators/immunosuppressants (tocilizumab, interferon, etc.) or treatments not included in Group I. |
| Grupo III | ICU admission or mechanical ventilation requirement |
ICU: Intensive Care Unit.
The following variables were analysed: age; sex; functional status (defined according to the ECOG scale)21; personal background; diagnosis; type of surgical intervention; the timing of SARS-CoV-2 infection; the treatment required (Table 1); the severity of the respiratory infection (according to the BRCSS)20; and postoperative complications (according to the Dindo–Clavien classification).19
Statistical analysis was performed using SPSS® v.23 (SPSS®, Chicago, Illinois, USA). The qualitative variables were expressed as a number and a percentage and the median quantitative variables with the median and interquartile range. Categorical variables were analysed with Fisher's exact test. The differences were considered statistically significant when the P-values were <.05.
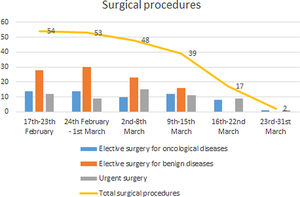
ResultsBetween 17th February and 31st of March 2020, 213 patients underwent a surgical procedure: 59 (27.8%) on an elective basis for oncological disease, 97 (45.5%) on an elective basis for benign disease, and 57 (26.7%) as urgent procedures.
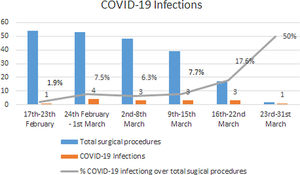
Until 6th March, the usual surgical activity was maintained, but it subsequently decreased, initially at the expense of scheduled procedures for benign diseases and then, after 14th March, with an almost total suspension of surgical activity. Fig. 1 describes the weekly activity level of the surgical department. Out of the 213 patients who were operated on, 15 (7%) presented with a confirmed SARS-CoV-2 infection postoperatively. Fig. 2 describes the number of SARS-CoV-2 infections and the percentage of infected patients over the total number of surgeries performed per week.
Ten (16.9%) of the oncological patients, one (1%) of those operated on electively for benign diseases and four (7%) of the urgent surgery group presented with a SARS-CoV-2 infection, with statistically significant differences in the infection rate of the three groups (P=.004) (Table 2).
Five of the 15 COVID-19 infections were diagnosed during the hospitalisation; the rest of the patients were diagnosed after their discharge, without being able to specify whether the infection occurred during hospitalisation, during postoperative control in the clinic or outside the hospital environment.
Five patients presented with a severe respiratory infection that did not respond to symptomatic treatment or group I medications (Table 1), and thus required additional measures. Four of these patients had a background of oncological diseases: a cholangiocarcinoma, an adenocarcinoma of the pancreas, and a lymphoma in the group of oncologic patients undergoing elective surgery, and a lymphoma in active treatment that underwent drainage of an abscess urgently.
A total of three (1.4%) deaths occurred as a result of progression of the respiratory disease due to COVID-19: one (1.7%) in the group of oncologic patients and two (3.5%) in the group of patients operated on urgently.
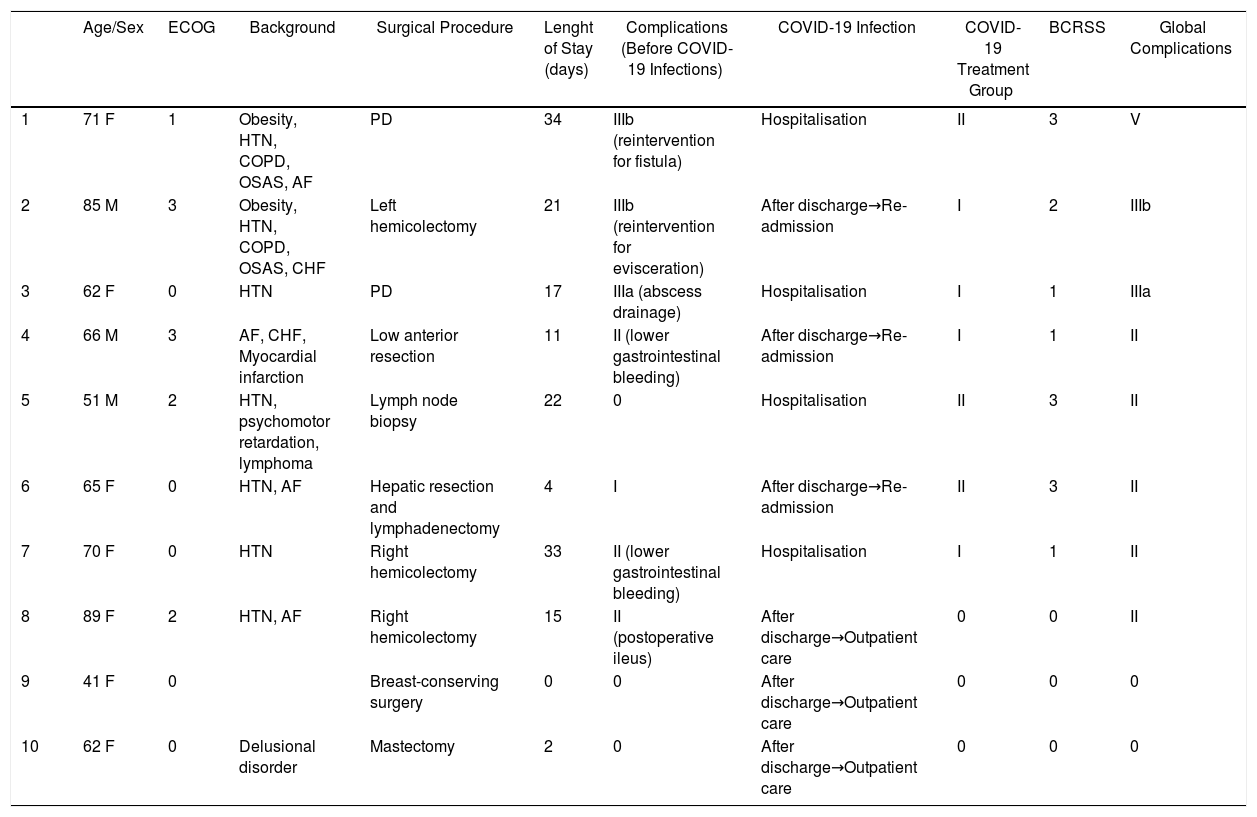
Elective Oncologic Surgery GroupOut of the 59 patients undergoing oncologic surgery, ten (16.9%) developed a SARS-CoV-2 infection (Table 3).
Patients Positive for COVID-19, Who Underwent Elective Surgical Procedures for Oncologic Diseases.
| Age/Sex | ECOG | Background | Surgical Procedure | Lenght of Stay (days) | Complications (Before COVID-19 Infections) | COVID-19 Infection | COVID-19 Treatment Group | BCRSS | Global Complications | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 71 F | 1 | Obesity, HTN, COPD, OSAS, AF | PD | 34 | IIIb (reintervention for fistula) | Hospitalisation | II | 3 | V |
| 2 | 85 M | 3 | Obesity, HTN, COPD, OSAS, CHF | Left hemicolectomy | 21 | IIIb (reintervention for evisceration) | After discharge→Re-admission | I | 2 | IIIb |
| 3 | 62 F | 0 | HTN | PD | 17 | IIIa (abscess drainage) | Hospitalisation | I | 1 | IIIa |
| 4 | 66 M | 3 | AF, CHF, Myocardial infarction | Low anterior resection | 11 | II (lower gastrointestinal bleeding) | After discharge→Re-admission | I | 1 | II |
| 5 | 51 M | 2 | HTN, psychomotor retardation, lymphoma | Lymph node biopsy | 22 | 0 | Hospitalisation | II | 3 | II |
| 6 | 65 F | 0 | HTN, AF | Hepatic resection and lymphadenectomy | 4 | I | After discharge→Re-admission | II | 3 | II |
| 7 | 70 F | 0 | HTN | Right hemicolectomy | 33 | II (lower gastrointestinal bleeding) | Hospitalisation | I | 1 | II |
| 8 | 89 F | 2 | HTN, AF | Right hemicolectomy | 15 | II (postoperative ileus) | After discharge→Outpatient care | 0 | 0 | II |
| 9 | 41 F | 0 | Breast-conserving surgery | 0 | 0 | After discharge→Outpatient care | 0 | 0 | 0 | |
| 10 | 62 F | 0 | Delusional disorder | Mastectomy | 2 | 0 | After discharge→Outpatient care | 0 | 0 | 0 |
F: female; M: male; ECOG: Eastern Cooperative Oncology Group; BCRSS: Brescia Respiratory COVID-19 Severity Scale; HTN: benign hypertension; COPD: Chronic Obstructive Pulmonary Disease; OSAS: Obstructive Sleep Apnoea Syndrome; AF: Atrial Fibrillation; CHF: Congestive Heart Failure; PD: Pancreatoduodenectomy.
The median age of these cases was 65 years (57–78), and three of the patients were male. The most frequently associated comorbidities were cardiovascular and respiratory. Two patients had undergone a pancreatoduodenectomy, five had a colorectal resection, two had a breast resection and one who was undergoing active treatment for lymphoma had an adenopathy removed. Three patients (5%) presented with grade ≥IIIa complications, according to Dindo–Clavien classification, before presenting the respiratory infection.
Four patients (6.7%) were infected during hospital admission, while six (10.1%) were discharged and diagnosed later. Three patients required symptomatic treatment, while the other seven required re-admission or prolonged hospitalisation. Of these, three presented with severe pneumonia that required group II treatment.
When we compared the changes in the severity of the complications, according to the Dindo–Clavien scale and before and after the respiratory infection, three patients presented with a modification in the severity of their complications and one of them died.
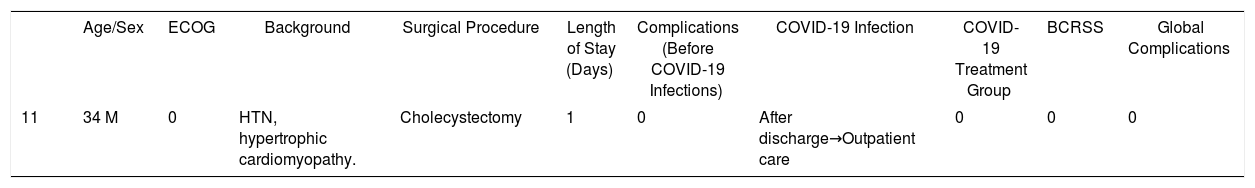
Elective Non-oncological Surgery GroupOf the 97 patients who underwent an elective non-oncological surgical procedure, one (1%) tested positive for COVID-19 (Table 4). The patient was treated at home with symptomatic treatment.
Patients Positive for COVID-19, Who Underwent Elective Surgical Procedures for Benign Diseases.
| Age/Sex | ECOG | Background | Surgical Procedure | Length of Stay (Days) | Complications (Before COVID-19 Infections) | COVID-19 Infection | COVID-19 Treatment Group | BCRSS | Global Complications | |
|---|---|---|---|---|---|---|---|---|---|---|
| 11 | 34 M | 0 | HTN, hypertrophic cardiomyopathy. | Cholecystectomy | 1 | 0 | After discharge→Outpatient care | 0 | 0 | 0 |
F: female; M: male; ECOG: Eastern Cooperative Oncology Group; BCRSS: Brescia Respiratory COVID-19 Severity Scale; HTN: benign hypertension.
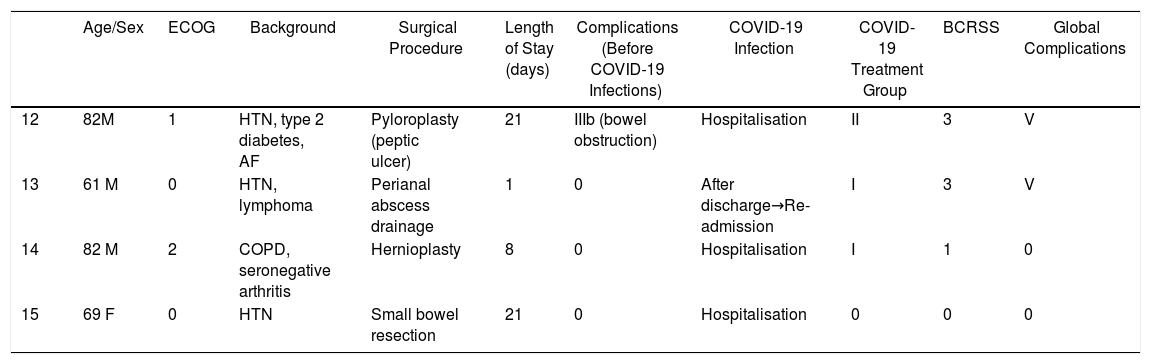
Of the 57 patients who underwent urgent surgery, four (7%) was positive for COVID-19 (Table 5). One patient (1.7%) presented with grade ≥IIIa complications, according to Dindo–Clavien, before testing positive for COVID-19 and required a reoperation due to intestinal obstruction.
Patients Positive for COVID-19, Who Underwent Urgent Surgical Procedures.
| Age/Sex | ECOG | Background | Surgical Procedure | Length of Stay (days) | Complications (Before COVID-19 Infections) | COVID-19 Infection | COVID-19 Treatment Group | BCRSS | Global Complications | |
|---|---|---|---|---|---|---|---|---|---|---|
| 12 | 82M | 1 | HTN, type 2 diabetes, AF | Pyloroplasty (peptic ulcer) | 21 | IIIb (bowel obstruction) | Hospitalisation | II | 3 | V |
| 13 | 61 M | 0 | HTN, lymphoma | Perianal abscess drainage | 1 | 0 | After discharge→Re-admission | I | 3 | V |
| 14 | 82 M | 2 | COPD, seronegative arthritis | Hernioplasty | 8 | 0 | Hospitalisation | I | 1 | 0 |
| 15 | 69 F | 0 | HTN | Small bowel resection | 21 | 0 | Hospitalisation | 0 | 0 | 0 |
F: female; M: male; ECOG: Eastern Cooperative Oncology Group; BCRSS: Brescia Respiratory COVID-19 Severity Scale; HTN: benign hypertension; COPD: Chronic Obstructive Pulmonary Disease; AF: Atrial Fibrillation.
Three patients (5.2%) were diagnosed during admission, while one (1.7%) was diagnosed after discharge and required readmission for the respiratory infection. One patient required symptomatic treatment, another required group I treatment and the remaining two required group II treatment.
When we compared the changes in the severity of complications before and after the respiratory infection, two patients, who eventually died due to respiratory infection, presented a modification in the severity of the complications, according to Dindo–Clavien classification.
DiscussionThis analysis confirms the high rate of SARS-CoV-2 infection in patients undergoing surgical procedures and its higher incidence in oncologic patients. Our data supports the experiences published by Asian and European authors10,11,22 who have shown an increase in morbidity and mortality in patients undergoing surgical procedures during the pandemic.
There are pathophysiological elements and epidemiological data that allow us to suppose that adding surgical stress to a patient with COVID-19 or, conversely, the infection developing in an operated patient can be very harmful to patients undergoing major surgery, especially oncological surgery.10–12 A recently published study by an Asian group suggests an increased susceptibility to developing a severe SARS-CoV-2 infection in patients with malignancy, probably due to underlying immunosuppression.6 The authors describe a severe respiratory infection rate up to 75% in patients operated on or treated in the month before the SARS-CoV-2 infection. Our data describe an infection rate of 16% and a mortality rate from respiratory failure of 1.7% in oncologic patients operated on in the month before and during the peak of the COVID-19 pandemic. In addition to this, the five patients who presented with a severe infection in our series needed group II treatment; four of these were patients who had a background of oncological diseases. Although there could be a greater susceptibility to infection in the group of oncologic patients, it should also be considered that these patients were the ones who presented with a higher rate of postoperative complications and longer hospital stays and, therefore, an increased risk of hospital transmission. In summary, the pathophysiological alterations due to tumour disease, as well as the increase in morbidity secondary to the surgical procedure and the prolongation of a hospital stay, could contribute to an increase in the infection rate of SARS-CoV-2.
Regarding the contagion rate, five patients were diagnosed with COVID-19 after being admitted to a ward that was supposed to be COIVD-19 free. The source of the infection could not be clearly determined in the ten patients who were diagnosed after discharge without ruling out nosocomial contagion. Among the possible causes of a nosocomial infection one could have been the limitations of diagnostic tests and false negatives, as also documented by other authors.23 However, the real efficiency of the isolation measures established during the pandemic is questionable, too. Despite several security measures as: the creation of areas dedicated to patients without respiratory symptoms and/or suspicion of COVID-19 infection; the addition of measures for both cleaning and protecting professionals and patients; the application of traffic restrictions in these areas; these measures may not have been sufficient to guarantee the absence of nosocomial infections. Therefore, it would be necessary to consider the design of a watertight circuit including all the stages of the diagnostic and therapeutic process of the patients admitted during the pandemic.
It is highly likely that, in the months following the peak of the pandemic, a more or less prolonged period of ‘coexistence’ with the disease due to COVID-19 will have to be experienced, generating the problem of the resumption of surgical activity, especially in oncologic patients. Although delaying oncologic patients’ treatments can worsen their long-term prognosis,6,10,11 it is very important to consider the increase of postoperative morbidity and mortality of these patients if they are infected with SARS-CoV-2. In order to offer the best possible treatment, it is necessary, on the one hand, to optimise the available resources and, on the other, to prioritise the patients who are awaiting surgical intervention.24
Regarding the optimisation of the available resources for the resumption of surgical activity in hospitals that have been treating patients with COVID-19, it would be necessary to guarantee security measures for both the patients and the professionals who look after them.16 If we cannot achieve national or regional coordination for the creation of centres that are exclusively dedicated to the treatment of positive or disease-free patients, we believe that there are fundamental premises that will need to be respected in each centre. These measurements are based on the following points:
- 1)
The creation of decontamination programmes in the case of a proven or suspected area of infection and the design of appropriately prepared clean, watertight areas, possibly with colour codes (for example, green, yellow and red) and according to the risk of possible environmental contamination in the future.25,26
- 2)
The selection and training of staff.6,27
- 3)
A guarantee of patient safety, detecting asymptomatic cases that could worsen after the intervention.27,28
- 4)
The prevention of the contamination of these protected areas in order to avoid outbreaks within hospitals, thus guaranteeing the safety of patients and staff.29,30
Regarding the prioritisation of patients on the surgical waiting list, it should be kept in mind that during the ‘coexistence’ with the pandemic, it is unlikely that the patients can be assured of the complete absence of a risk of infection after surgical procedures. Decision-making regarding the most appropriate treatment for each patient should be carried out through a multidisciplinary committee, based on the following factors:
- a)
The risk of complications related to the patient (preoperative anaesthetic classification ASA, ECOG).21,31
- b)
The risk of complications related to the disease, its progression and the surgical procedure.32–35
- c)
The availability of therapeutic alternatives to lower surgical risks (chemotherapy, radiotherapy, endoscopic procedures, thermal ablation, etc.).36–39
- d)
The timeframe related to the evolution of the pandemic, health care pressure and the available resources in each centre.4
This prioritisation of the indications must, undoubtedly, include detailed information for the patients and their families about the risks and benefits in each case, as well as the necessary family support at home after the discharge due to the importance of early hospital discharge in order to reduce the risk of infection. Patients should be thoroughly informed of the risks and benefits of undergoing the surgical procedures based on their comorbidities, the condition of the hospital regarding the spread of the pandemic and the characteristics of the surgical procedure itself. The risk of acquiring SARS-CoV-2 infection, its repercussion on the development of postoperative complications and the eventual associated mortality must be clearly and concisely explained to the patient. In addition, the patient must be informed regarding any change in the long-term prognosis of his or her disease and the benefit that the surgical treatment could bring in his or her case.
ConclusionsPatients undergoing elective surgery before and during the peak of the COVID-19 pandemic showed a high rate of postoperative complications, with a SARS-CoV-2 infection rate of up to 16% in patients undergoing oncologic surgical procedures.
The resumption of surgical activity in hospitals that have been treating, and continue to treat, COVID-19 positive patients should be based on a prioritisation of the cases to be operated on, respecting safety rules and optimising available resources in order to assure the safety of both patients and staff members.
Coauthors' GroupElena Bermejo Marcos, Carlos Cerdán Santacruz, Jesús Delgado Valdueza, Beatriz Doblado Cardellach, Iñigo García Sanz, Alberto Gimeno Calvo, Cristina Marín Campos, José Luis Martín Álvarez, Teresa Pérez de la Fuente, Ana Rodríguez Sánchez, Mónica Sánchez Gallardo, Luis Sánchez-Urdazpal González, Emma Torres Mínguez, Álvaro Valdés de Anca, Francisco Eduardo Viamontes Ugalde, Jose María Lopesino González, Lara Blanco Teres, Álvaro Gancedo Quintana, Julia Revuelta Ramírez, Livia Delgado Burdalo, Rodrigo Tovar Pérez, Ramón Sanz Ongil.
Conflict of interestThe authors certify that there is no conflict of interest with no financial/research/academic organization, regarding the content that is analyzed in the manuscript.
Please cite this article as: Di Martino M, García Septiem J, Maqueda González R, Muñoz de Nova JL, de la Hoz Rodríguez Á, Correa Bonito A, et al. Cirugía electiva durante la pandemia por SARS-CoV-2 (COVID-19): análisis de morbimortalidad y recomendaciones sobre priorización de los pacientes y medidas de seguridad. Cir Esp. 2020. https://doi.org/10.1016/j.ciresp.2020.04.029