We distributed a survey in order to determine the current indications for the use of colonic stents to treat colonic obstruction in Spain and its compliance with international guidelines.
MethodsDescriptive study of a survey distributed by the Spanish Association of Surgeons (Asociación Española de Cirujanos), the Catalan Society of Surgery (Societat Catalana de Cirurgia) and the Spanish Society of Digestive Endoscopy (Sociedad Española de Endoscopia Digestiva).
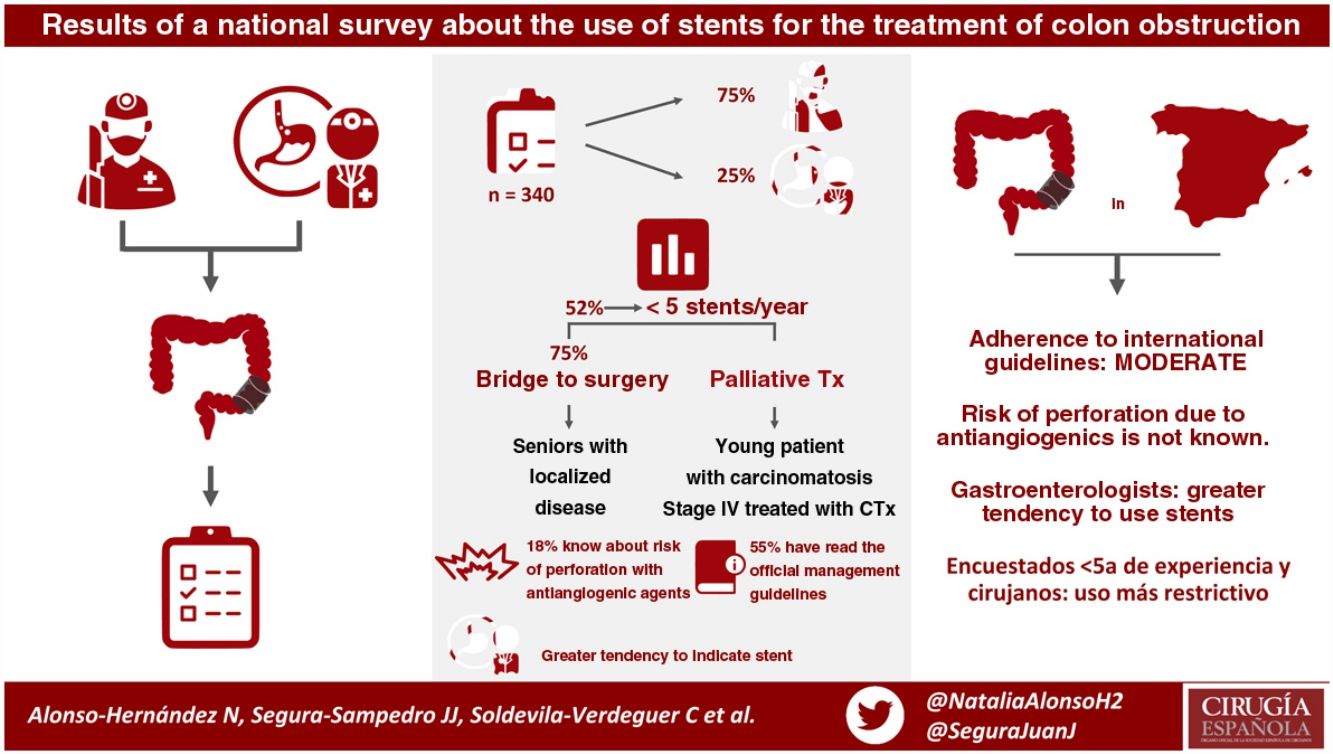
Results340 valid responses were received: 25% from gastrointestinal specialists, and 75% from general surgeons. During the last year, 44.4% of respondents assessed between 10 and 20 COC. Of these, 52.2% indicated less than 5 stents/year, 75% of which were indicated as a prior step to preferential surgery and only 25% were performed with palliative intent. 55.3% of the participants reported knowing the official guidelines, and 64% of respondents would use the stent as a step prior to surgery in elderly patients with localized disease. 75.9% would place stents as palliative therapy in young patients with carcinomatosis, and 61.8% would use them in stage IV malignancies under treatment with chemotherapy. Only 18.1% knew of the risk of colon perforation after stent placement in patients undergoing treatment with antiangiogenics.
ConclusionsIn Spain, the indication for colonic stents is reserved for selected cases and varies according to the specialty and the years of experience of the respondent. The compliance with international guidelines of most respondents is moderate. It is important to insist on the high risk of perforation after angiogenics, which is unknown to most surgeons.
Difundimos una encuesta con el objetivo de conocer las indicaciones actuales para la utilización del stent de colon para el tratamiento de la obstrucción colónica en España y su adecuación a las guías internacionales.
MétodosEstudio descriptivo de una encuesta distribuida por la Asociación Española de Cirujanos, la Societat Catalana de Cirurgia y la Sociedad Española de Endoscopia Digestiva.
ResultadosSe recibieron 340 respuestas válidas, un 25% de médicos digestólogos, y el 75% de cirujanos generales. Durante el último año el 44,4% de los encuestados valoró entre 10 a 20COC. Un 52,2% indicó menos de 5 stents/año, y de estos el 75% se indicó como paso previo a una cirugía preferente y solo el 25% se realizó con intención paliativa. Un 55,3% de los participantes refirió conocer las guías oficiales. El 64% de los encuestados utilizaría el stent como paso previo a cirugía en ancianos con enfermedad localizada. El 75,9% colocaría stent con fines paliativos en jóvenes con carcinomatosis, y un 61,8% los utilizaría en neoplasias estadio IV en tratamiento con quimioterapia. Solo un 18,1% conocía el riesgo de perforación de colon tras stent en pacientes en tratamiento con antiangiogénicos.
ConclusionesEn España la indicación del stent de colon se reserva para casos seleccionados y varía según la especialidad y los años de experiencia del encuestado. La adecuación a las guías internacionales para la mayoría de los encuestados es moderada. Es importante insistir en el alto riesgo de perforación tras angiogénicos, pues la mayoría de profesionales lo desconocen.
It is estimated that some 41,411 new cases of colon cancer are diagnosed in Spain each year, and 10%-30% begin with clinical signs of colon obstruction.1
Treatment of the obstruction differs according to the hospital in which it is treated. Decision-making is influenced by both patient characteristics—tumor location, extension of the oncological disease, age and comorbidities—as well as the characteristics of the healthcare setting—the surgeon's or gastroenterologist's preferences, caseload and availability of resources. For these reasons, different management options include: urgent surgery, decompression with colonic stent prior to preferential surgery (CS-S), and colonic stent as palliative therapy or to initiate neoadjuvant therapy (CS-P).
The objective of this study was to determine the indications for colonic stents (CS) as a treatment for obstructive colon cancer (OCC) performed in Spanish hospitals. As secondary objectives, we analyzed whether there was agreement between these indications and the recommendations of official European and American guidelines (compliance with guidelines) and whether knowing these official guidelines influenced the responses of the participants.2
MethodsA descriptive study was conducted with data collected through an online survey sent to the members of the Spanish Association of Surgeons (Asociación Española de Cirujanos), Catalan Society of Surgery (Societat Catalana de Cirurgia) and the Spanish Society of Digestive Endoscopy (Sociedad Española de Endoscopia Digestiva). The email of each respondent was registered to avoid duplicate responses.
The survey was carried out from March to May 2017 using Google Forms (Appendix B, Annex 1). It consisted of 23 questions, divided into 3 sections: epidemiological data of the respondent (5 questions), data about the hospital where they work (8 questions), and the presentation of 7 theoretical clinical cases (Appendix B, annex 2). Two additional questions were included to determine whether the participant had read the official guidelines and whether they would like to be informed of the results of the survey. At the end of the survey, a link was given for the official ESGE guidelines on the use of colonic stenting in bowel obstruction.
Statistical AnalysisThe statistical analysis was carried out with the SPSS computer software from 2008, version 16.0. The descriptive analysis of the variables was carried out, including means and medians, as well as the proportions for the categorical variables of the main results.
Surveys that did not have complete epidemiological and workplace data were excluded.
ResultsWe received 388 surveys, 340 of which were complete. The epidemiological data of the respondents, as well as the data referring to their usual clinical situation, are summarized in Table 1. In terms of the main national societies, 4.5% of AEC members and 10.5% of SEED associates responded.
Epidemiological Data and Usual Hospital Workplace.
| Epidemiological DataN: 340 | Data from Hospital WorkplaceN: 340 | Data from Hospital WorkplaceN: 340 |
|---|---|---|
| Spanish region of workplaceMadrid 14.1% (48)Catalonia 13.5% (46)Andalusia 11.7% (40)Valencia 8.8% (30)Other 51.5% (176) | N of hospital beds<300 beds 29.1% (99)300–600 beds 35%(119)600–1000 beds 27% (92)>1000 beds 8.8% (30) | Need referral to other hospital?Yes 17% (57)No 83% (283) |
| SexMales 55.8% (190)Females 44.2% (150) | N OCC/year<10 40.6% (138)10–20 44.4% (151)>20 15% (53) | Who placed stent?Endoscopist 67% (228)Interventional Rx 16% (56)Both 16% (56) |
| Age<30 years 5.3% (18)30–40 years 40% (136)40–55 years 39.4% (134)>55 years 15.2% (52) | N stents/year<5 51% (175)5–10 36% (122)10–15 9% (30)>15 4% (13) | Delay in days until surgery in patients with bridge-to-surgery stents?<5 days 11% (39)5–10 days 27% (91)10–15 days 29% (99)>15 days 33% (111) |
| SpecialtyDig. Surg. 44.7% (152)CR Surg. 30.7% (104)GI 24.7% (84) | Percentage CS-S/CS100% CS-S 19% (64)75% CS-S 41% (138)50% CS-S 16% (56)25% CS-S 18% (62)0% CS-S 6% (20) | Have you read the guidelines?Yes 55% (188)No 45% (152) |
| Years of experience<5 years 6% (22)5–10 years 27% (92)10–25 years 44% (149)>25 years 23% (77) | Percentage CS-P/CS0% CS-P 9% (31)25% CS-P 41% (138)50% CS-P 24% (83)75% CS-P 20% (69)100% S 6% (19) | Would you be interested in receiving the results of this survey?Yes 98.8% (336)No 0% (0)Did not respond 0.2% (4) |
The majority of those surveyed (65%) worked in medium-sized hospitals (300–600 beds) or regional hospitals (less than 300 beds). Only 8.8% were employed at hospitals with more than 1000 beds.
When we analyzed the subgroup of gastroenterologists, 98.9% reported it was not necessary to refer patients to another hospital for stent placement. Also, the specialist who placed the stent was the gastroenterologist, either as the only specialist in the hospital in 88% or as an alternative to interventional radiologists in 10.8% of the gastroenterology specialists surveyed.
If we analyze the subgroup of hospitals with less than 300 beds, we observe that they assessed fewer colon obstructions than the larger hospitals. However, the proportion of the number of CS indicated during the last year was similar between the different hospital sizes.
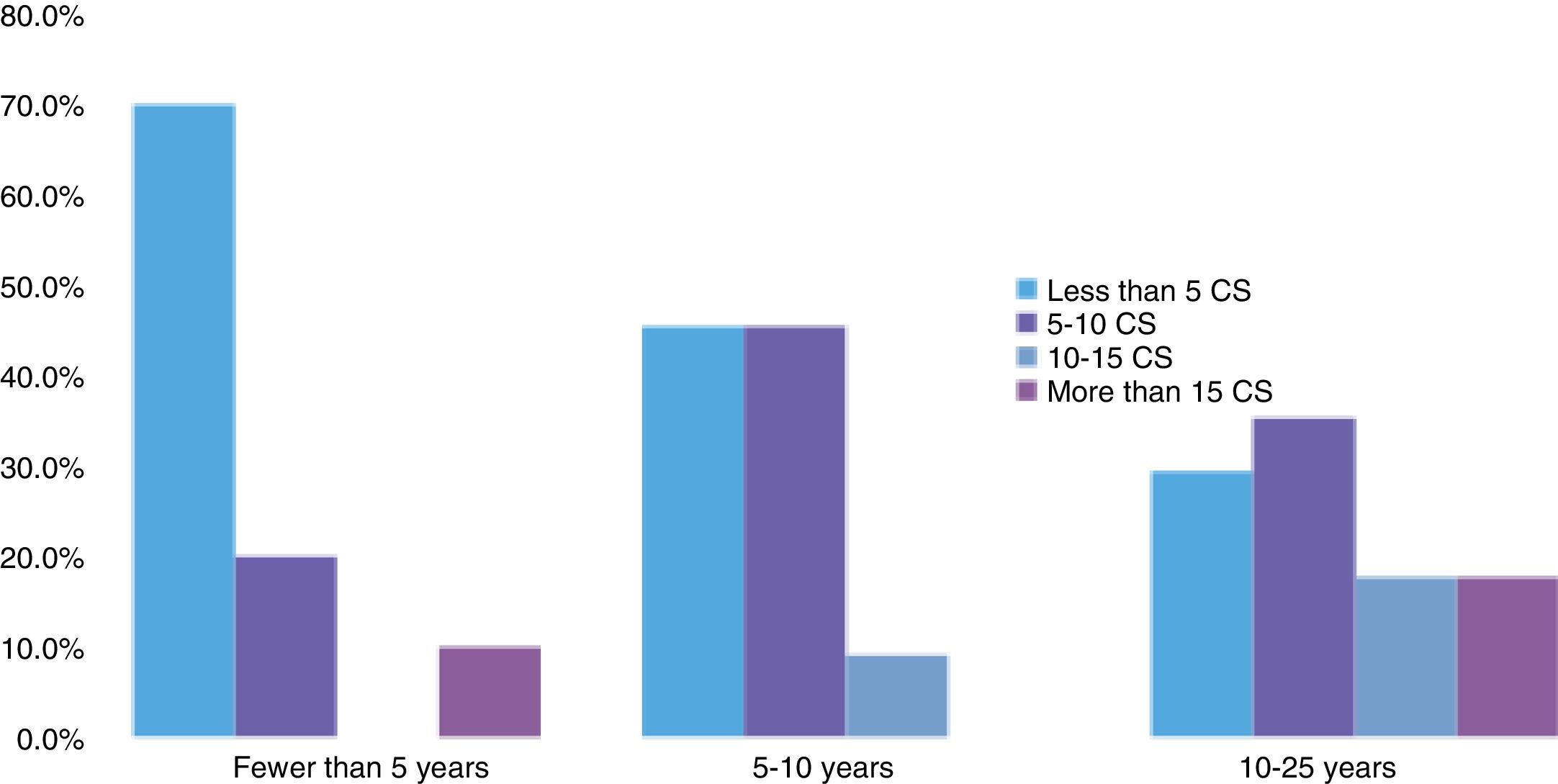
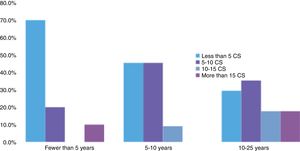
Among the groups with different years of experience, the group of professionals with fewer than 5 years of experience evaluated a higher number of OCC than the most experienced specialists, but no great differences were observed in the number of CS indicated. If we focus on the group that assessed the highest number of OCC (more than 20 per year), a greater tendency to indicate CS was observed in respondents with more than 25 years of experience (Figure 1).
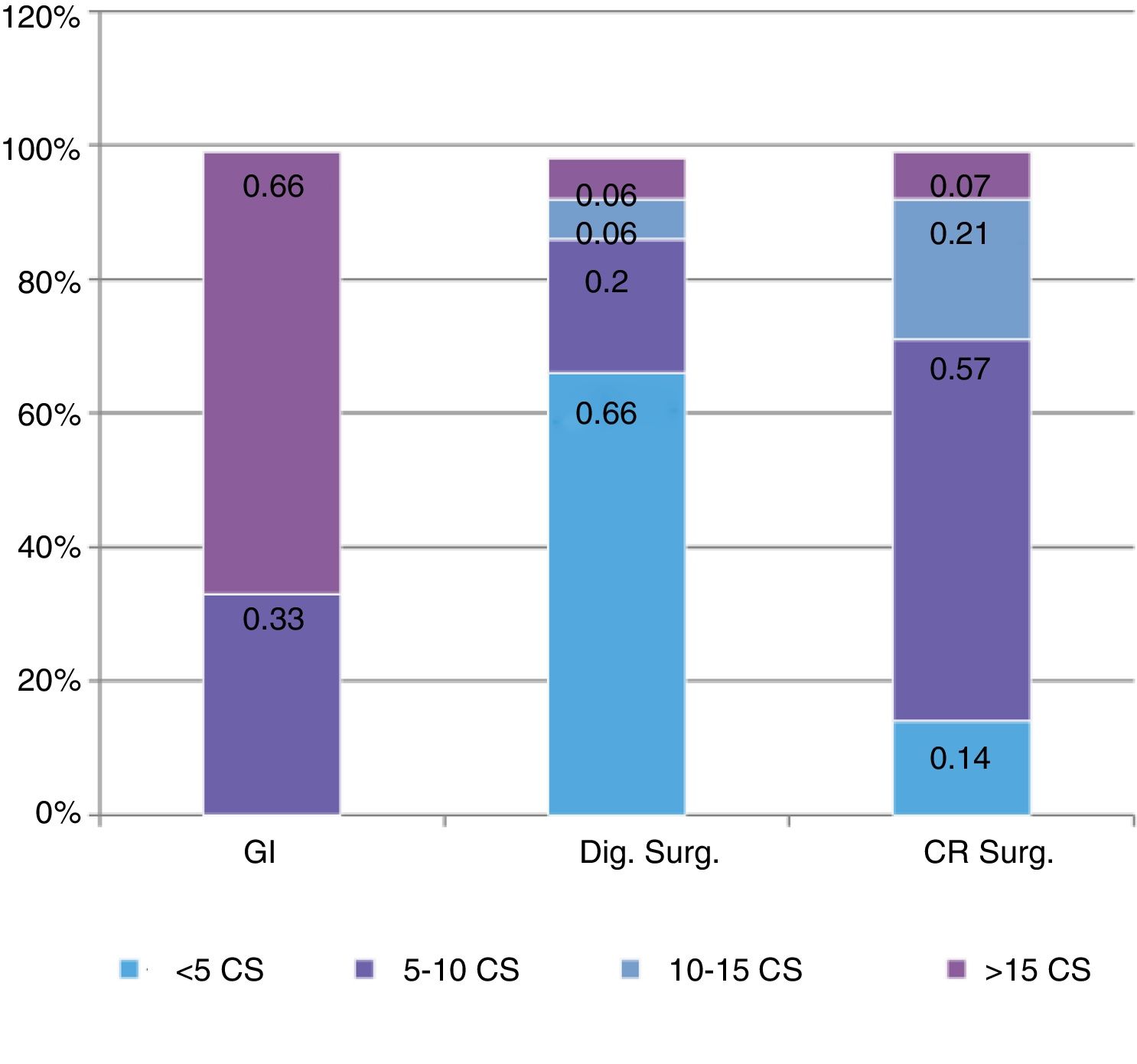
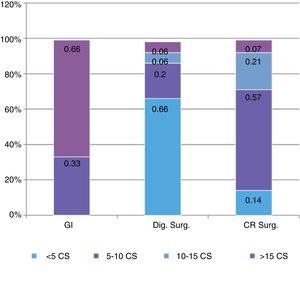
Also within this subgroup that assessed the highest number of OCC during the last year (more than 20 OCC), differences were observed depending on the medical specialty of the respondent. There was a greater tendency to place stents (more than 15 in the last 12 months) in the group of gastroenterology specialists compared to other specialties: fewer than 5 for general surgeons, and 5 to 10 stents during the last year for colorectal surgeons (Figure 2).
The most frequent indication for CS was as a step prior to preferential surgery (CS-S), which represented 75% of the indications for the majority of those surveyed (41%), while palliative colonic stent (CS-P) represented 25% of its indications. These indications were similar between general surgeons and specialists in colorectal surgery, although for the group of gastroenterologists the proportion of CS-S was 50% of their indications and CS-P the remaining 50%.
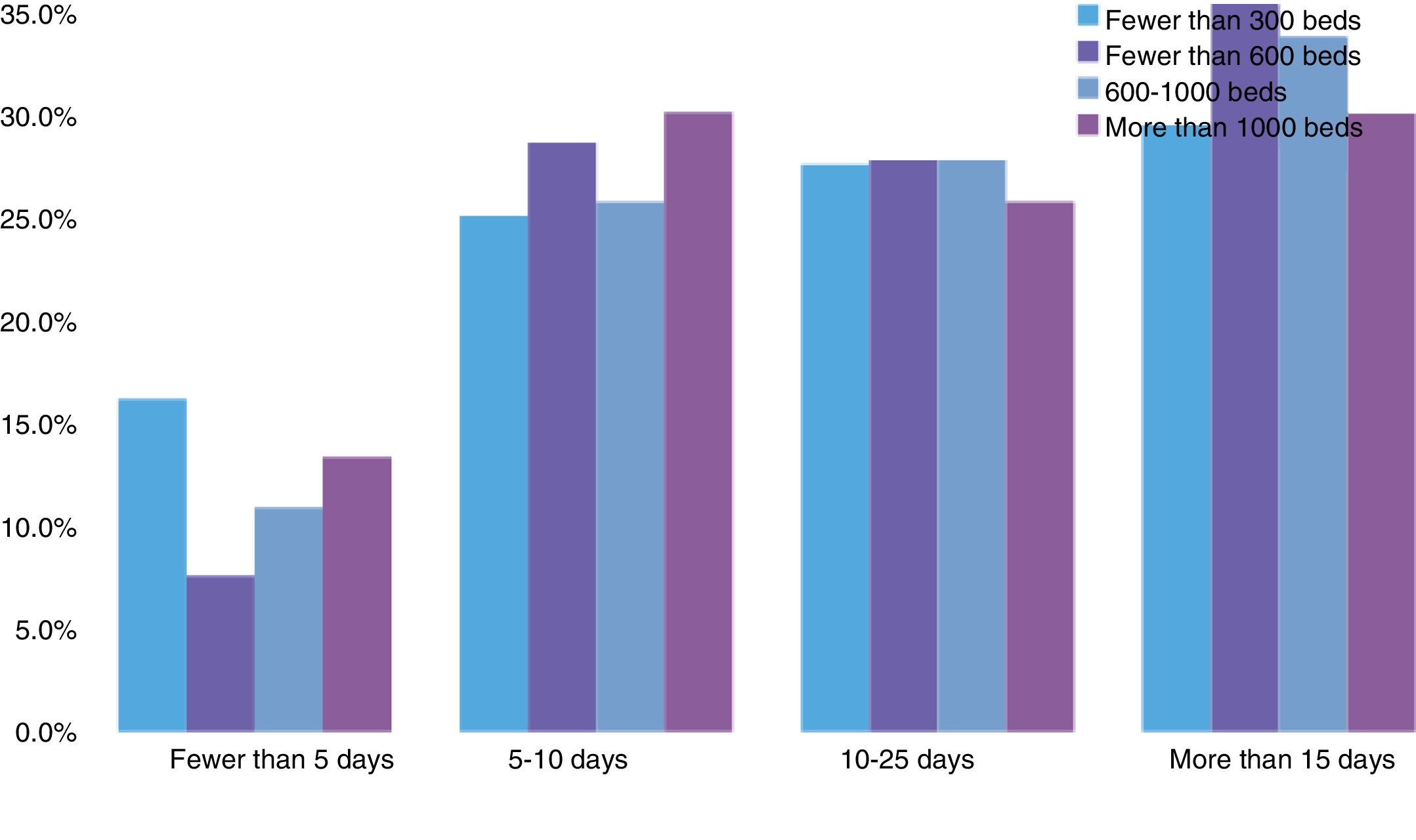
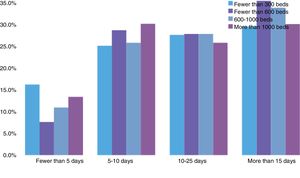
The time interval between stent placement and surgery was more than 15 days for most of the participants (33%). Only 27% complied with the recommendations of the official guidelines for an interval of 5 to 10 days. There were no differences in terms of hospital size (Figure 3).
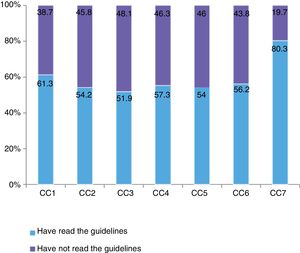
Regarding the knowledge of the official guidelines, 55% of the participants reported having read them. Within this group, there was a greater proportion of gastroenterologists and colorectal surgeons than general and digestive surgeons.
Clinical CasesThe responses given by the respondents to the different clinical cases with colon obstruction are summarized in Table 2.
Result CS-S.
| Case Reports of Occlusive Colon Cancer | ResultsN=340 |
|---|---|
| CC1Young, healthy,neo. sigmoid,no extension | Urgent surgery 60% (204)CS-S 39.7% (135)CS-P 0% (0)Did not respond 0.3% (1) |
| CC2Senior, healthy,neo. sigmoid,no extension | Urgent surgery 33% (112)CS-S 66% (225)CS-P 1% (3) |
| CC3Senior, healthy,rectal neo. at 6cm,no extension | Urgent surgery 63.2% (214)CS-S 36.2% (124)CS-P 0% (0)Did not respond 0.5% (2) |
| CC4Senior, healthy,right neo.,no extension | Urgent surgery 89% (300)CS-S 11% (37)CS-P 0% (0)Did not respond 0.9% (3) |
| CC5Median age,neo. sigmoid,discomfort RIF, diastasis cecumno extension | Urgent surgery 70% (239)CS-S 28% (94)CS-P 1.5% (5)Did not respond 0.5% (2) |
| CC6Young, healthy,neo. sigmoid,carcinomatosis | Urgent surgery 4% (15)CS-S 6% (19)CS-P:For study and treatment 76% (258)Palliative 14% (48) |
| CC7Young, stage IV in CTx,neo. sigmoid,carcinomatosis | Urgent surgery 12% (41)Urgent surgery if antiangiogenics18% (61)CS-S 8% (27)CS-P to continue CTx61% (207) |
ESGE-ASGE 2014 recommendations are in bold.
65.2% of the respondents’ responses followed the recommendations of the official guidelines. Compliance did not change with the years of experience of the respondents.
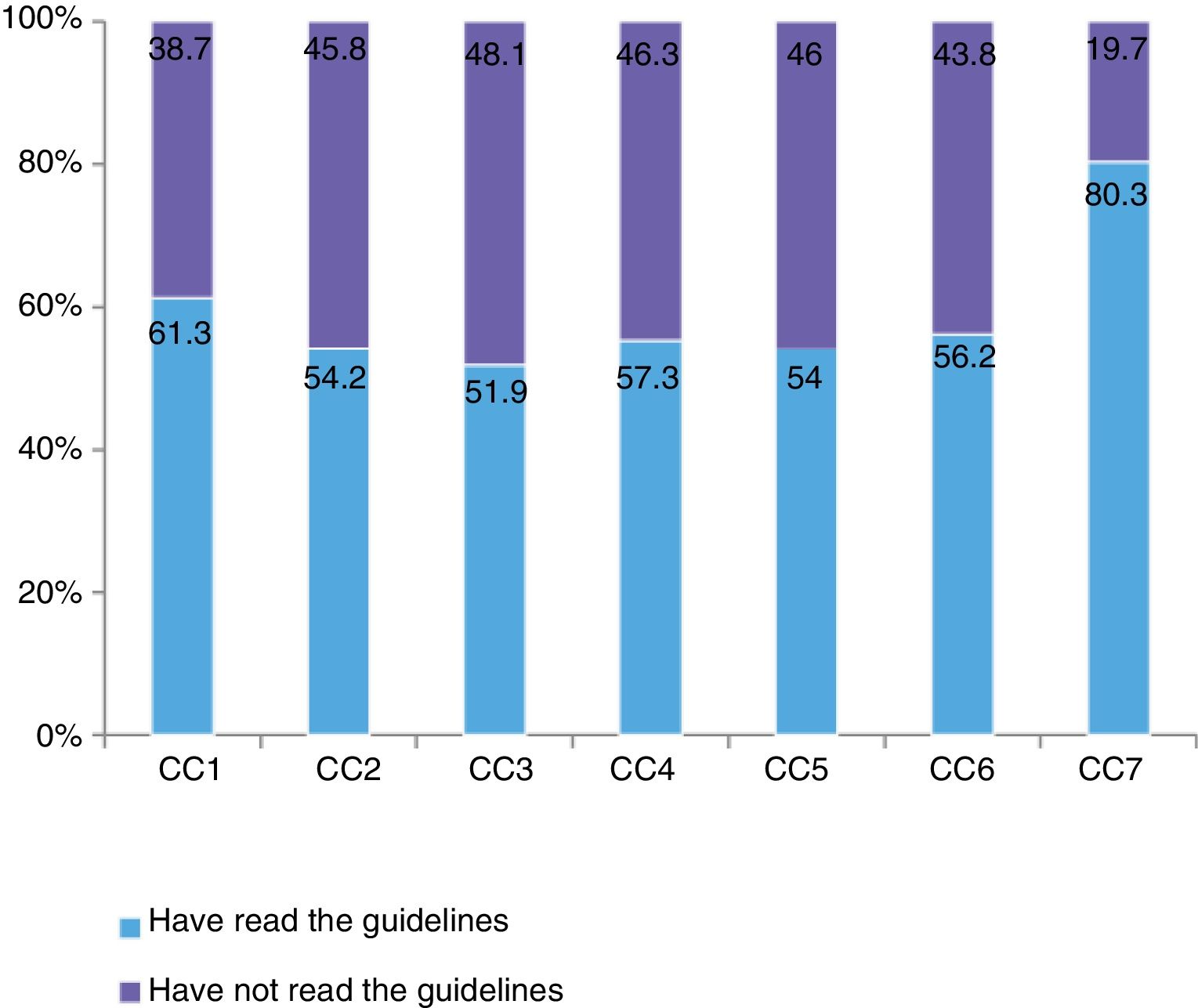
We compared the specialists who reported knowing the guidelines versus those who did not, without observing differences in the overall number of responses according to the guideline recommendations between the 2 groups. However, when we analyzed each clinical case separately, a greater proportion of agreement with the guidelines stood out in the group that did know them for CC7 (Stage IV, under treatment with antiangiogenics) (Figure 4).
The size of the hospital did not modify the degree of adherence to the guidelines.
DiscussionSince the appearance of CS, several official guidelines have been published for the treatment of OCC,2–5 which coincide in the majority of their recommendations. In other European countries like France, Sweden, Norway and the Netherlands, CS have been all but abandoned.3 Meanwhile, stents continue to be the standard treatment for many surgeons in the United Kingdom, who are themselves responsible for their placement. In Spain, the situation and compliance with guidelines had not been determined.
The results obtained in our survey confirm that CS are part of the therapeutic arsenal of surgeons and gastroenterology specialists in Spain. Bridge-to-surgery stenting (CS-S) is reserved for elderly patients with obstructive sigmoid colon disease and no CT scan findings of extension (64% of respondents), while it is indicated for palliative purposes in young patients with carcinomatosis (75.9%) and for patients with stage IV neoplasms under treatment with chemotherapy (61.8%).
The responses collected are very heterogeneous. The majority demonstrated adherence to the official guidelines (32%-36% made 4–5 indications in accordance with the guidelines from a total of 7 CC). Compliance rates did not increase in the group that reported having read the guidelines.
34.8% of respondents did not follow the instructions of the official recommendations. This lack of adherence to clinical practice guidelines is consistent with the literature and with a similar study conducted in Canada.6 The causes for this lack of compliance can be varied, from fear of possible complications derived from the use of the stent to lack of means for its placement at the time of indication, or the difficulty in managing and scheduling preferential surgery after the placement of said stent.
One of the cases with the greatest discrepancies was CC2 (elderly man with localized sigmoid neoplasia). 35% of the participants indicated surgery instead of the CS-S recommended by the guidelines. This fact may indicate a certain limitation in the use of stents. When we analyzed the subpopulations of those who indicated surgery (Table 3), we observed that they were slightly younger and had intermediate experience. However, there were no differences in terms of hospital size or the need for referral. There was a surprising short interval of days in the group that indicated surgery, with a waiting time of 5 to 10 days between the stent and surgery.
Analysis of CC2 Response.
| CC2 Surgery Response | CC2 Stent Response (CS-S and CS-P) | |
|---|---|---|
| Age | ||
| <30 years | 8.9% | 3.5% |
| 30–40 years | 41.4% | 39% |
| 40–55 years | 36.6% | 40.7% |
| >55 years | 12.5% | 16.6% |
| Years of experience | ||
| <5 years | 8.9% | 24.5% |
| 5–10 years | 33.9% | 23.6% |
| 10–25 years | 38.3% | 46.5% |
| >25 years | 18.7% | 24.5% |
| Hospital size | ||
| <300 beds | 33.9% | 26.7% |
| <600 beds | 30.3% | 37.2% |
| 1000 and >1000 beds | 37% | 35.9% |
| Specialty | ||
| Colorectal | 26.7% | 32.4% |
| General surgery | 53.5% | 40.3% |
| Gastroenterologist | 19.6% | 27.19% |
| N OCC assessed last year | ||
| <10 OCC | 38.4% | 41.2% |
| 10–20 OCC | 27.6% | 46% |
| >20 OCC | 21.4% | 12.7% |
| N CS indicated last year | ||
| <5 CS | 67.8% | 43.4% |
| 5–10 CS | 24.1% | 41% |
| 10–15 CS | 0% | 10.5% |
| More than 15 CS | 2.6% | 4.4% |
| Need for referral for CS-placement | ||
| Yes | 17.8% | 16.2% |
| No | 82.1% | 83.7% |
| Percentage CS-S among total CS | ||
| None | 13.4% | 2.2% |
| 25% | 33.9% | 10.5% |
| 50% | 13.4% | 18.4% |
| 75% | 28.5% | 46% |
| 100% | 10.7% | 22.8% |
| Percentage of CS-P among total CS | ||
| None | 4.4% | 11% |
| 25% | 16% | 49.5% |
| 50% | 26.7% | 23.2% |
| 75% | 33% | 14.03% |
| 100% | 10% | 2.2% |
| Days between CS-S and surgery | ||
| <5 days | 17.8% | 8.3% |
| 5–10 days | 49.1% | 28.07% |
| 10–15 days | 0% | 31.14% |
| More than 15 days | 33% | 32.4% |
| Have read the guidelines | ||
| Yes | 56.2% | 54.8% |
| No | 43.7% | 45.17% |
The data for the greatest percentages of each variable analyzed are in bold.
We found a higher percentage of participants who assessed fewer colon obstructions in the group that indicated surgery and also indicated a lower number of CS per year, reserving CS mostly for use as CS-P.
There were no major differences in the percentage that reported having read the guidelines; there was only a slightly higher percentage of those familiar with the guidelines among the specialists who indicated surgery. It therefore seems that one of the causes of this lack of adherence in CC2 was the tendency to reserve CS for palliative indications, as demonstrated by observing a greater compliance with the recommendations of the guidelines in cases of palliative use (CC6 and CC7).
We should comment on the delay in surgery involved in the placement of CS-S, reported as greater than 15 days by most surgeons. These responses were similar among all participants, regardless of hospital size, which may reflect the difficulty in managing hospital resources to meet the deadlines recommended by the literature, far from the reality of healthcare practice.
The gastroenterologists showed a greater tendency to indicate CS and a lack of adherence to the guidelines in the CC (3, 4 and 5) when they recommended urgent surgery. This may be influenced by the fact that urgent surgery is not part of the therapeutic arsenal of gastroenterologists. It should be noted that this discrepancy coincides with the clinical practice reported by British surgeons, who also share the possibility of placing CS.
In smaller hospitals, fewer assessed colon obstructions were reported. In addition to the smaller population of their area, other factors may be responsible for this lower number of indications, such as the need to refer patients to another hospital for placement.
Only 18.1% of the participants were aware of the risk of colon perforation after CS placement in patients treated with antiangiogenic agents. The increasing use of antiangiogenic drugs makes it essential to know this fact, since it implies worse clinical and oncological prognosis for the patient.2,7
Limitations of Our StudyAs it is a survey, the responses provided about previous activities may be influenced by subjective perceptions of the respondent, and therefore differ from the use of CS and its actual indications due to memory bias. Similarly, there may be a certain participation bias in the survey, and those who have responded are mainly those most interested in the use of the stent, altering the representativeness of its use. These biases could be avoided through a national registry on CS use, which would obtain more reliable data on their actual use in Spain.
ConclusionColonic stents are an established therapeutic option for the treatment of colon obstruction in Spain. The vast majority of participants used it only in selected cases, and we observed heterogeneous indications and a greater tendency of its use by gastroenterologists than by surgeons.
The compliance with international guidelines reported by most participants was moderate.
A high percentage of respondents did not act in accordance with the recommendations, and we have observed a tendency to reserve SC for indications of CS-P.
Most professionals surveyed did not know about the risk of perforation after CS in patients receiving antiangiogenic drugs.
There are no guidelines promoted by the different Spanish associations that address CS management. This study demonstrates the need for nationwide recommendations.
Conflict of InterestsThe authors have no conflict of interests to declare.
The authors would like to thank the Asociación Española de Cirujanos, Societat Catalana de Cirurgia and the Sociedad Española de Endoscopia Digestiva for their approval and distribution of the survey, as well as all the participants for their responses.
Please cite this article as: Alonso-Hernández N, Segura-Sampedro JJ, Soldevila Verdeguer CM, Ochogavía Seguí A, Olea Martinez-Mediero JM, Fernández Isart M, et al. Resultados de una encuesta nacional sobre el uso de stent para el tratamiento de la obstrucción de colon. Cir Esp. 2020. https://doi.org/10.1016/j.ciresp.2020.02.006