The aim of this study is to evaluate the single port access technique in colorectal disease, as regards its suitability to oncological criteria, reliability, safety and reproducibility of the technique. A descriptive and prospective case study is performed describing the preliminary results of our series.
Materials and methodsWe present a series of 24 patients with colorectal disease who underwent single port access surgery using a Gel point® device between June and December 2010. The operations performed were: 9 right hemicolectomies, 9 sigmoid resections, 4 high anterior resections, 1 left hemicolectomy due to a tumour of the splenic flexure, and 1 sub-total colectomy.
ResultsThe mean surgical time for the right colon was 82.8min (range 40–170), 122.1min (range 75–200) for the left colon and rectum, and 270min for the sub-total colectomy. The median number of ganglia resected was 22 (range: 3–27) for the right colon and 21 (range: 11–28) for the left colon/rectum. The mean length of the surgical specimen was 20.37cm (range: 16.2–27.5) for the right colon, and 24.92cm (range: 14.5–31) for the left colon/rectum. The median overall hospital stay was 6 days (range: 5–13). Morbidity was 8.3% (2 patients); one with an occlusion due to adhesions, and another with a leak in the anastomosis. There were no deaths.
ConclusionsThe single port access technique is safe and reproducible, maintaining oncological criteria, for surgeons accustomed to colorectal surgery by conventional laparoscopy.
A larger number of cases would be required to standardise the technique.
El objetivo del estudio es la evaluación de la técnica monopuerto en patología colorrectal en cuanto su adecuación a criterios oncológicos, fiabilidad, seguridad y reproductibilidad de la técnica. Se realiza un estudio descriptivo y prospectivo de casos describiendo los resultados preliminares de nuestra experiencia.
Material y métodosPresentamos una serie de 24 pacientes con patología colorrectal intervenidos mediante abordaje monopuerto con dispositivo Gel point® durante el periodo de tiempo comprendido entre junio y diciembre del año 2010. Se realizaron 9 hemicolectomías derechas, 9 resecciones de sigma, 4 resecciones anteriores altas, 1 hemicolectomía izquierda por tumour de ángulo esplénico y 1 colectomía subtotal.
ResultadosEl tiempo quirúrgico medio, para el colon derecho fue de 82,77 minutos (rango 40-170), de 122,14 minutos (rango 75-200) para colon izquierdo y recto y de 270 minutos en la colectomía subtotal. La mediana de número de ganglios resecados fue de 22 (rango: 3-27) para colon derecho y 21 (rango 11-28) para colon izquierdo/recto, la media de longitud de la pieza quirúrgica fue de 20,37cm (rango 16,20-27,50) para colon derecho y 24,92cm (rango 14,50-31) para el colon izquierdo/recto, la mediana de estancia hospitalaria global fue de 6 días (rango 5-13). La morbilidad fue del 8,3% (2 pacientes), uno presento una oclusión por bridas y otro fuga en la anastomosis. No hubo mortalidad.
ConclusionesEl abordaje monopuerto es una técnica reproductible y segura, manteniendo criterios oncológicos, en cirujanos habituados a la cirugía colorrectal por vía laparoscópica convencional.
Sería necesario un mayor número de casos para la estandarización de la técnica.
Since the beginning of laparoscopic surgery, various studies have been done comparing the laparoscopic and conventional approaches to colorectal pathology. Laparoscopic surgery has aesthetic and patient welfare advantages, as well as less postoperative pain, a better immune response (CLASICC, COST) and a faster integration into working life. The results for morbidity, mortality and long-term outcomes are similar to open surgery,1–5 preserving oncological criteria (tumour size, resection margins and number of lymph nodes).6
Currently, approaches are being developed to try to reduce parietal trauma using laparoscopic surgery as the basis: surgery through natural orifices (NOTES), surgery with 3mm instruments and surgery via a single incision (SILS®, LESS®, Gel point®).7–23
This study describes the technical details of single port colon surgery, with an analysis of results from our experience to assess the feasibility and safety of the surgical approach.
Materials and MethodsA descriptive case study was performed by prospectively collecting data from patients who underwent single port colorectal surgery between June and December 2010.
The following inclusion criteria were used:
- •
Patients with a preoperative diagnosis of colorectal carcinoma or benign lesions not susceptible to endoscopic resection.
- •
Patients with a diagnosis of complicated diverticular disease with surgical indication.
- •
An absence of distant disease for those with malignant disease.
- •
Elective surgery.
- •
ASA anaesthetic risk
The following exclusion criteria were used:
- •
Emergency pathology.
- •
Mid and lower rectum.
- •
ASA anaesthetic risk ≥IV.
Data on the patients’ clinical characteristics, the surgical technique, Anatomical pathology, hospital stay and intraoperative and postoperative complications were gathered.
Technical and Scientific Quality RequirementsInformed consent (standardised by the Spanish association of surgeons) was duly completed by all patients.
Preoperative staging by abdominal ultrasound and double-contrast axial CT was performed in all patients, ruling out distant disease (exclusion criterion).
ResultsA total of 24 patients were intervened by single port laparoscopic surgery, using the Gel point® device in all cases.
Clinical CharacteristicsThe study consisted of 17 men and 7 women, with an average age of 61.17 years (range 37–82). The mean body mass index (BMI) was 27.92 (range 17–32). There was a history of previous abdominal surgery in 29.2% of patients (2 appendectomies, 2 cholecystectomies, 1 hysterectomy, 1 prostatectomy and 1 inguinal hernia).
The American Society of Anesthesiologists (ASA) risk classification was used to assess anaesthetic risk. There were 2 patients with ASA I (8.3%), 20 patients with ASA II (83.3%) and 2 patients with ASA III (8.3%).
The lesion was located in the right colon in 9 patients, in the left colon in 14 patients (1 splenic flexure, 9 sigma and 4 upper rectum) and 1 patient had multiple polyposis.
The median hospital stay was 6 days (range 5–13).
Surgical TechniqueA right hemicolectomy was performed in 9 patients (37.5%), a left hemicolectomy in 1 patient (4.2%), sigmoid resection in 9 (37.5%), upper anterior resection in 4 (16.7%) and a subtotal colectomy in 1 (4.2%). All cases were performed by the same surgeon within a team that specialised in advanced laparoscopic surgery and colorectal surgery.
All operations were performed under general anaesthesia and pneumoperitoneum pressure of 14mmHg. A 5mm, 30° integrated optic (Olympus®) and conventional straight instrumentation were used in all cases.
In the right colon processes, the patient was placed in the supine position, with a certain degree of Trendelenburg or on the patient's right side according to the time of surgery. The surgeon and assistant were to the patient's left, with the video-laparoscope to the patient's right.
For left colon processes, the patient was placed in a modified lithotomy position (to allow for transanal anastomosis) and a degree of Trendelenburg according to the surgical time. The surgeon and assistant were to the patient's right and the video-laparoscopy device to the patient's left.
In all cases, the Gel point® device (Fig. 1) was used as the working channel. The initial incision was 3cm for all patients as this length was sufficient to insert the device and was independent of the size and location of the lesion. However, depending on the size and difficulty in removing the surgical specimen, the incision was extended to 5cm in some cases. The transumbilical approach was used for the right colon, while for the left colon, the incision was right pararectal in the first 10 cases and transumbilical in the others. The Gel point® device had a gel cap that allowed up to 4 trocars (Fig. 2). In all cases, 4 trocars were placed on the device, 3 of 10mm and 1 of 12mm.
The incision was closed in layers with absorbable braided suture in the peritoneum and fascia. An absorbable braided suture was used in the skin with inverted separate stitches in the dermis.
An additional trocar was required to be inserted in the left parietocolic space for 2 patients, due to technical difficulties (a very redundant sigmoid in 1 case, and traction of the piece while sectioning in a case of upper rectal cancer). A 5mm trocar was used for traction and to help the dissection.
All tumours were treated with oncological criteria. For right hemicolectomies, the dissection began by ligation of its vein and ileocolic artery at the base, then ligation of the right branch of the middle colic artery. In no case was it necessary to perform a ligation of the middle colic artery or extend the dissection transversely, as the more distal lesion was on the hepatic flexure. Dissections on the left side were begun by performing a ligation of the vein and inferior mesenteric artery for the left colon with the inclusion of the mesorectum in the upper rectum. The splenic flexure was released in those cases where it was necessary, due to the tension the colorectal anastomosis may experience. In those cases where the lesion was on the upper rectum, it was preferred to perform a lower anterior resection to ensure that the distal margin was sufficient in terms of oncological safety.
The removal of the specimen and preparation for anastomosis was performed with the same device, by removing the gel cap. This manoeuvre is facilitated by the inside of the Gel point® being covered with a plastic bag protecting the wound and preventing the risk of contamination and tumour spread. The gel cap was then reinserted and the surgery continued without loss of pneumoperitoneum.
In the right colon, the transit reconstruction was sutured with end-to-side extracorporeal circular suture EEA 28 (Covidien®) and GIA 80 (Covidien®) for resection of the colon, with partial closure of the mesocolon in all cases.
For the left colon and subtotal colectomy, the reconstruction was end-to-end with circular suture (Covidien®) via the transanal and intracorporeal routes.
No drains were placed routinely. A closed active drain was placed in 2 patients due to greater technical difficulty. The surgical wound was closed in layers, with absorbable material.
The mean operating time was 82.77min (range 40–170) for the right colon, 122.14min (range 75–200) for the left colon and rectum, and 270min in subtotal colectomy.
ComplicationsConversion to midline laparotomy was necessary in 2 patients (8.3%) who had both undergone a right hemicolectomy. The first was due to multiple adhesions after prior surgery for endometrial carcinoma, and the second due to observing a large tumour of the ascending colon adhered to the wall.
There were 2 patients (8.3%) with complications in the immediate postoperative period. The first who had undergone right hemicolectomy required a reoperation (3-trocar laparoscopy) for an obstruction secondary to adhesion at the terminal ileum; the patient progressed favourably. Another patient who had undergone a right hemicolectomy presented rectal bleeding at 24h and subsequent leakage of the anastomosis on the 4th day, secondary to a diagnostic colonoscopy and infiltration of the serum with adrenaline for haemostasis. Laparoscopic reoperation was required and conversion to laparotomy was required for ileocolic anastomosis reconstruction; the patient progressed satisfactorily and was discharged after 13 days.
Anatomical PathologyThe 9 right colon lesions consisted of 6 adenocarcinomas and 3 adenomas. The lesions located in the sigmoid colon consisted of 5 adenocarcinomas, 1 adenoma and 3 diverticulitis. In the splenic flexure, there was an adenocarcinoma. There were 4 adenocarcinomas in the rectum; while for the subtotal colectomy, there was multiple polyposis with an adenocarcinoma-type lesion in the sigmoid region.
The average length of the surgical specimen was 20.37cm (range: 16.20–27.50) for the right colon and 24.92cm (range 14.50–31) for the left colon and rectum. The subtotal colectomy length was 89.50cm. The median number of lymph nodes removed was 22 (range: 3–27) for the right colon, and 21 (range: 11–28) for the left colon/rectum.
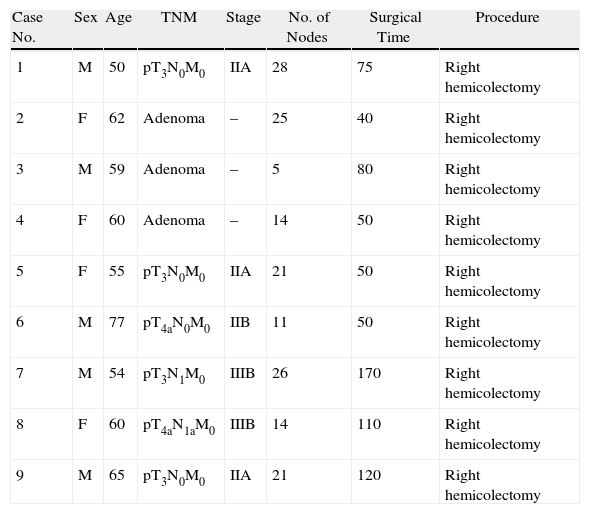
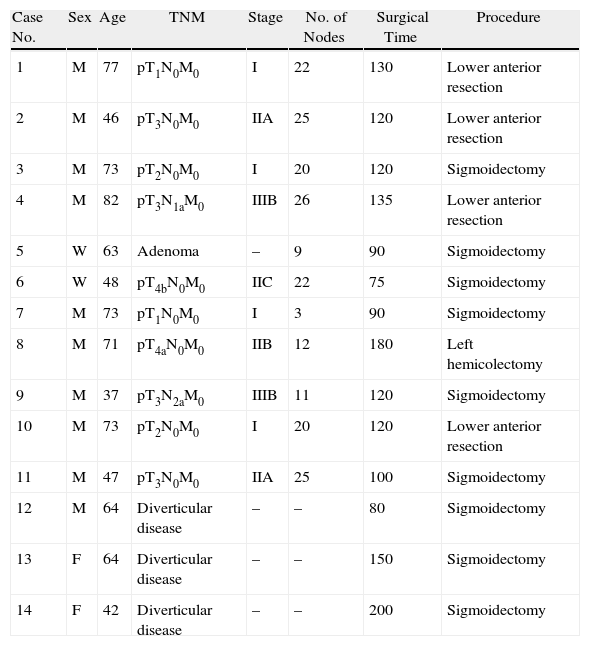
Patients were classified histopathologically according to the pTNM staging system, excluding patients with diverticular disease and benign lesions (Tables 1 and 2).
Right Colon Surgery.
| Case No. | Sex | Age | TNM | Stage | No. of Nodes | Surgical Time | Procedure |
| 1 | M | 50 | pT3N0M0 | IIA | 28 | 75 | Right hemicolectomy |
| 2 | F | 62 | Adenoma | – | 25 | 40 | Right hemicolectomy |
| 3 | M | 59 | Adenoma | – | 5 | 80 | Right hemicolectomy |
| 4 | F | 60 | Adenoma | – | 14 | 50 | Right hemicolectomy |
| 5 | F | 55 | pT3N0M0 | IIA | 21 | 50 | Right hemicolectomy |
| 6 | M | 77 | pT4aN0M0 | IIB | 11 | 50 | Right hemicolectomy |
| 7 | M | 54 | pT3N1M0 | IIIB | 26 | 170 | Right hemicolectomy |
| 8 | F | 60 | pT4aN1aM0 | IIIB | 14 | 110 | Right hemicolectomy |
| 9 | M | 65 | pT3N0M0 | IIA | 21 | 120 | Right hemicolectomy |
Left Colon Surgery.
| Case No. | Sex | Age | TNM | Stage | No. of Nodes | Surgical Time | Procedure |
| 1 | M | 77 | pT1N0M0 | I | 22 | 130 | Lower anterior resection |
| 2 | M | 46 | pT3N0M0 | IIA | 25 | 120 | Lower anterior resection |
| 3 | M | 73 | pT2N0M0 | I | 20 | 120 | Sigmoidectomy |
| 4 | M | 82 | pT3N1aM0 | IIIB | 26 | 135 | Lower anterior resection |
| 5 | W | 63 | Adenoma | – | 9 | 90 | Sigmoidectomy |
| 6 | W | 48 | pT4bN0M0 | IIC | 22 | 75 | Sigmoidectomy |
| 7 | M | 73 | pT1N0M0 | I | 3 | 90 | Sigmoidectomy |
| 8 | M | 71 | pT4aN0M0 | IIB | 12 | 180 | Left hemicolectomy |
| 9 | M | 37 | pT3N2aM0 | IIIB | 11 | 120 | Sigmoidectomy |
| 10 | M | 73 | pT2N0M0 | I | 20 | 120 | Lower anterior resection |
| 11 | M | 47 | pT3N0M0 | IIA | 25 | 100 | Sigmoidectomy |
| 12 | M | 64 | Diverticular disease | – | – | 80 | Sigmoidectomy |
| 13 | F | 64 | Diverticular disease | – | – | 150 | Sigmoidectomy |
| 14 | F | 42 | Diverticular disease | – | – | 200 | Sigmoidectomy |
Although conventional laparoscopic surgery produces little trauma to the abdominal wall, it requires 4–5 working ports and minilaparotomy (5–8cm) for the extraction of the surgical specimen.
To minimise surgical trauma, reduce the risk of complications (e.g., infection, hernia or implants) at the ports of entry and shorten patient convalescence, other less aggressive approaches have been developed. Natural orifice surgery (NOTES)7–9 and single-incision surgery (SILS®, LESS, etc.)10–14 have been effective in dealing with simple surgeries, such as cholecystectomy and appendectomy, with results similar to those of conventional laparoscopic surgery. This has extended its indication to more complex interventions, such as obesity15,16 and colorectal surgery.17,18
NOTES surgery currently has a number of instrumental limitations (still under development): the difficulty of triangulation for certain technical manoeuvres, surgical specimen size and access routes. Although some published results have been aceptable,19 it is technically difficult and not very reproducible, which limits the progress of the technology and its standardisation.The single-incision technique has fewer problems, provides a view of the abdominal cavity similar to standard laparoscopic surgery and follows the same steps for cancer surgery.20–23
The SILS® or LESS® type devices are used with small incisions of just 2–3cm to prevent loss of pneumoperitoneum and to keep the device in place. To extract the specimen, the wound must be enlarged in most cases, with the resulting loss of pneumoperitoneum due to continuing the laparoscopic surgery and the subsequent risk of wound contamination. SILS® requires a protective wall to be added to manipulate the specimen without contaminating the wound. LESS® has a protective device, but this cannot be used if the incision has to be extended to remove the specimen. The Gel point® includes a wall protection device (Alexis® type) and allows an initial 3cm incision which can be easily widened to extract the specimen, minimising the risk of wound contamination and the possibility of tumour spread in the abdominal wall.
SILS® and LESS® type devices have a smaller diameter, making triangulation with the forceps difficult. They also require the use of curved or hinged forceps, while at times having to use the non-dominant hand to perform some precise manoeuvres.
We used the Gel point® device in all our cases. This device avoided the technical difficulties we encountered in the use of other single-port devices in less complex surgery (cholecystectomy, appendix, hernia), such as triangulation, the use of conventional straight forceps20 and systematically working manually. In addition, the size of the laparotomy did not have to be modified to remove the specimen, and portals of 5, 10, 12 or 14mm could be used as required by insertion in the gel. This allowed single-port surgery to follow the steps of conventional laparoscopic surgery safely, according to oncological criteria.24,25
In our cohort, lymph node removal, with a median of 22 nodes for the right colon and 21 for the left, was acceptable for current oncologic criteria and comparable to the reviewed studies.1–4,24,25 Also, after evaluating the resection margins, they were always found to be appropriate regardless of the lesion location. The morbidity observed was comparable with current quality standards used in the conventional laparoscopic technique.
By including a device to protect the wall, it reduced the risk of surgical wound infection and metastatic implants. However, lesions larger than 8cm were a relative contraindication for the technique,26 given the difficulty in handling the lesion laparoscopically and removing it. Similarly, locally advanced lesions with invasion of the parietal peritoneum or adjacent organs represented a problem, and the open approach must be considered as an option. These two latter conditions are determining factors for performing the laparoscopic procedure, either conventionally or by a single port. In addition, BMI is an independent factor in evaluating the technique, as those patients with a BMI over 30 have more adipose tissue in the abdominal wall and mesocolon, making manipulation difficult when performing the dissection.27 It is known that the thicker the abdominal wall, the more difficult it is to operate the forceps in the conventional technique. However, this technical difficulty does not exist for single-port devices, as the forceps can move freely in the space created. The technique is reproducible and similar to conventional laparoscopic surgery, and therefore has a similar learning curve.
We observed no technical differences in dissection when comparing it to the conventional laparoscopic approach for the transumbilical route to the right colon. The technique is not adapted to this approach, but it is performed in the same way as the usual approach. Thus, dissection is conveniently performed in the right colon (irrespective of the location of the lesion).17,18 There were no transverse injuries in our cohort, so a ligation of the middle colic pedicle or extension of the dissection was not necessary. Anastomosis could be performed completely with an intracorporeal approach, using the endoscopic stapler and closing the inlet port of the machine with a manual suture in 2 layers. This was technically more difficult when tying and manipulating the needle. Due to the complexity of this anastomosis, we preferred to perform extracorporeal anastomosis in this initial series.
In the first cases of the left colon, the right pararectal route was used, as it was considered a technically simpler approach for being ‘farther’ from the mesenteric vessels. After gaining confidence and safety with the single-port approach, we routinely made a transumbilical incision without noting any greater technical complexity. Thus, currently we use the transumbilical approach in both the right colon and left colon, regardless of the size or location of the tumour.28 The umbilical approach is not a limiting technique when performing colorectal anastomosis, as long as the left colon is properly released, as is usually done in the conventional laparoscopic technique.21–23 It is clear that the more redundant the sigmoid colon is, the less release is required. In addition, once the colon is exteriorised, it should be checked that the site selected for the proximal section is easily manoeuvred without stressing the patient's pubis.
We excluded patients with lesions of the middle and lower rectum, as we believed that using the articulated cutting machine on the distal portion was technically difficult in these cases, as it leaves an oblique section, which limits the safety of later end-to-end colorectal anastomosis (with an increased risk of leakage). An additional 12mm trocar is recommended in these cases in the right iliac fossa for the linear endocutter.
As in any new surgery, placing and locating the device was technically more difficult in the first cases. Triangulation is feasible, however, one has to get used to working in a different horizontal plane with each hand so as not to strike the forceps outside the abdomen. The same situation occurred when an assistant had to introduce a third clamp through the fourth trocar. Another useful recommendation is to remove the camera from the operating field with the use of integrated or long optics to minimise contact with the instruments.
We believe that the single-port approach for the management of colorectal disease is another option in the laparoscopic approach, as are robotic surgery and the natural orifice approach. It reduces the complications inherent in additional ports with the conventional technique. It is reproducible for surgeons familiar with laparoscopic surgical anatomy and the learning curve depends on getting used to the device and handling the forceps in different planes. We think its future lies at a point where there is less invasion, increased oncological and technical safety using single-port approach devices and robotic surgery, which are currently being developed on an experimental basis.
ConclusionThe single-port approach with the Gel point® device is reproducible, safe and maintains oncological criteria, for surgeons familiar with conventional laparoscopic colorectal surgery.
However, more cases are required to standardise the technique.
Please cite this article as: Durán Escribano C, et al. Cirugía Monopuerto en patología colorrectal: resultados preliminares. Cir Esp. 2011;89:588–94.