Scintigraphy with technetium-sestamibi (MIBI) is the test of choice for localising adenomas in patients with primary hyperparathyroidism (PHPT). In some studies it has emerged that the increase in sensitivity of this test could be associated with a decrease in the uptake of the radiotracer by the thyroid gland. The aim of this study is to analyse our experience in patients with a negative scintigraphy with MIBI, and in whom the study was repeated after suppression of thyroid function with thyroxine.
Material and methodsA prospective evaluation was performed on 17 patients who, between January 2006 and April 2011, had PHPT and negative imaging using scintigraphy with MIBI and who had the test repeated after the administration of thyroxine. The scintigraphy data and the correlation with the findings in the surgical intervention are reviewed.
ResultsThe mean TSH at the time of repeating the MIBI was 0.12±0.1mIU/L. Of the 17 patients included, the scintigraphy under thyroid suppression was positive in 13 of them (76.5%), and in the other 4 (23.5%) patients no image suggestive of adenoma was found. In the cases where the MIBI was positive after suppression, the positive predictive value (PPV) was 100%.
ConclusionSuppression of thyroid function by giving thyroxine can help to improve the sensitivity of MIBI in patients with previously negative scintigraphy studies and help in the minimally invasive treatment of patients with PHPT.
La gammagrafía con tecnecio-sestamibi (MIBI) es la prueba de elección para la localización de los adenomas en pacientes con hiperparatiroidismo primario (HPTP). En algunos estudios se ha sugerido que el aumento de la sensibilidad de esta prueba podría estar en relación con una disminución de la captación del radiotrazador por parte de la glándula tiroidea. El objetivo de este estudio es analizar nuestra experiencia en pacientes con gammagrafías con MIBI negativas en los que se repitió el estudio tras la supresión de la función tiroidea con tiroxina.
Material y métodosEntre enero de 2006 y abril de 2011 se evaluaron de forma prospectiva 17 pacientes con HPTP e imagen gammagráfica con MIBI negativa en los que se repitió dicha prueba tras la administración de tiroxina. Se revisan los datos gammagráficos y la correlación con los hallazgos en la intervención quirúrgica.
ResultadosLa media de TSH en el momento de repetir la MIBI fue de 0,12 ± 0,1 mIU/L. De los 17 pacientes incluidos, en 13 de ellos (76,5%) la gammagrafía bajo supresión de la función tiroidea fue positiva, y en los otros 4 pacientes (23,5%) no se encontró imagen sugestiva de adenoma. En los casos en los que el MIBI fue positivo tras la supresión, el valor predictivo positivo (VPP) fue del 100%.
ConclusiónLa supresión de la función tiroidea mediante la administración de tiroxina puede ayudar a mejorar la sensibilidad del MIBI en pacientes con estudios gammagráficos previos negativos y ayudar a tratar de una forma mínimamente invasiva a pacientes con HPTP.
The cause of primary hyperparathyroidism (PHPT) in about 90% of cases is a single adenoma.1 At present, the sensitivity of scintigraphy with technetium sestamibi (MIBI) as a localisation test in patients without associated thyroid nodular disease is 80%–95%,2 which allows minimally invasive selective surgery in most patients.2–4 The problem lies in that 10%–15% of cases where the possible adenoma is not detected by scintigraphy. There are several possible reasons for these false negatives, such as the existence of surgical thyroid nodular disease, small adenomas, or a low proportion of oxyphilic cells, although in many cases the real reason is unknown.5 An interesting article published in 2002 recommended suppressing the thyroid function with thyroxine as a method to improve the results with MIBI. No other article has been published since then to either refute or confirm this theory. The aim of our study was to subject patients with negative scintigraphic images to a new scintigraphy after suppression of thyroid function, and compare the results of our experience with the Royal et al.’s6 study.
Patients and MethodPatientsPatients with a clinical and biochemical diagnosis of PHPT between January 2006 and April 2011 in the Hospital Universitario de la Princesa (Madrid) were included. All cases had to be candidates for surgery with a previous negative scintigraphic image. All patients underwent cervical ultrasound and had to have no contraindication for taking thyroid hormone, especially due to heart problems. The hormone was administered initially at a dose of 1μg/kg with weekly analytical controls performed to maintain TSH levels of <0.3mIU/L. The scan was then repeated using the same technique and interpreted by the same nuclear medicine specialist. This image was compared with the previous one and correlated with the surgical findings.
Scintigraphic TechniqueAll patients received a 740MBq dose of 99mTc-sestamibi. The planar images were obtained using a high resolution collimator as close as possible to the patient's neck, with a 128×128 double zoom matrix and a single-head detector (General Electric, Fairfield, CT, USA). The early images were obtained 15min after administration of the radiotracer in 30° left and right anterior oblique positions, with finally a mediastinal image. The delayed images were obtained 90–120min after injection. All cases underwent a thyroid subtraction technique by injecting (185MBq) pertechnetate 240min after the sestamibi, and obtaining a static thyroid image 20min after injection. Thus, all patients were analysed with early and late sestamibi images and then by a subtraction image. All scintigraphic images were interpreted by the same nuclear medicine specialist. The scintigraphic image was considered positive if a focus of uptake independent of the thyroid gland and suggestive of abnormal parathyroid tissue was revealed.
ResultsThe study consisted of 17 patients, 12 of whom were women (70.6%), with a mean age of 62.1±7 years. Table 1 shows the demographic and biochemical characteristics of the patients. The mean preoperative calcium level was 2.8±0.2mmol/L and parathyroid hormone (PTH) 148±43ng/L. The mean TSH before repeating the MIBI was 0.12±0.1mIU/L.
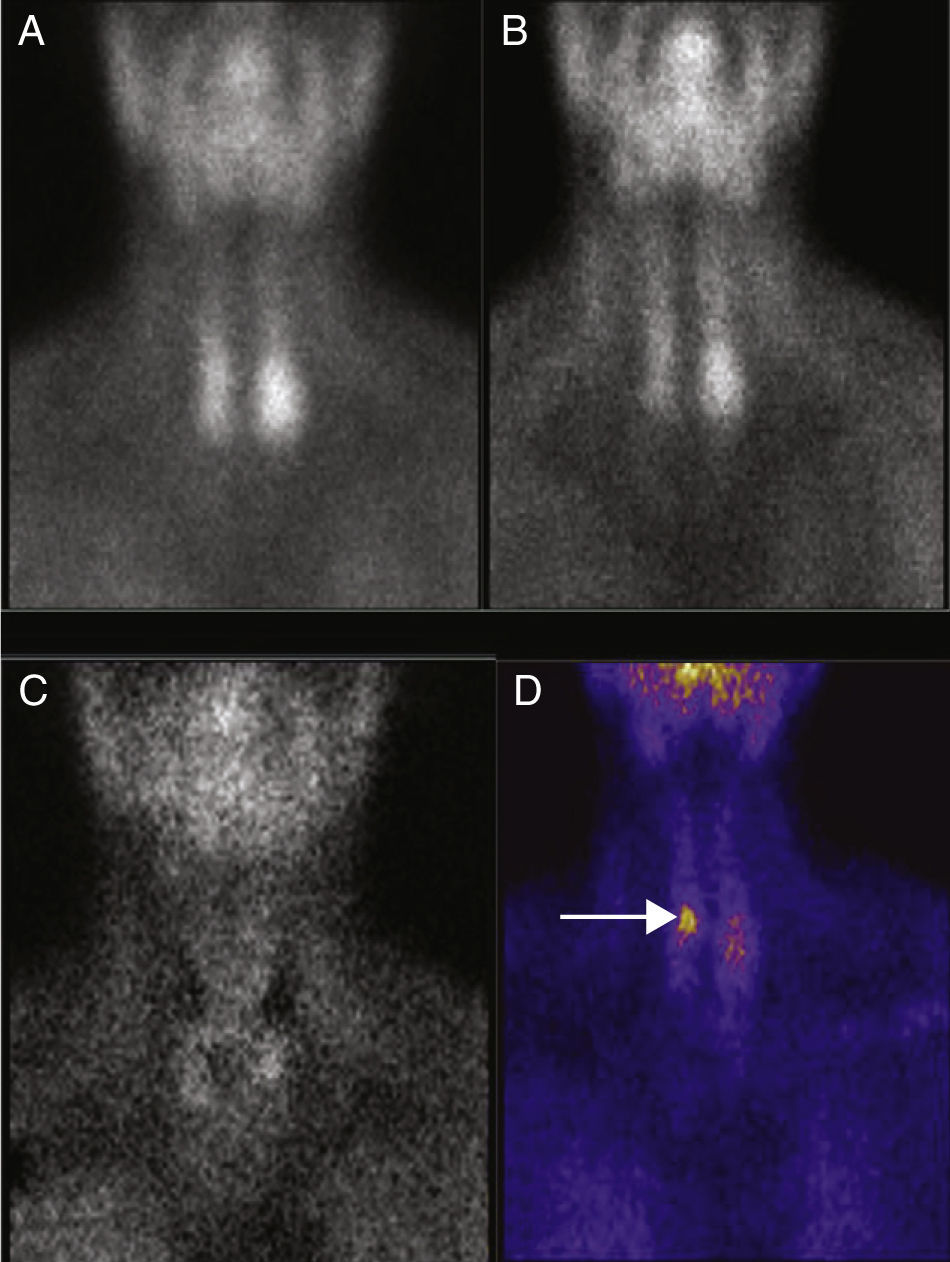
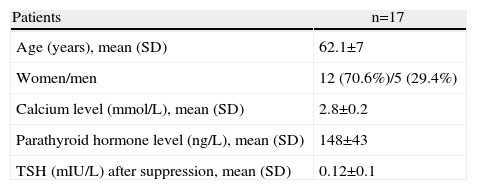
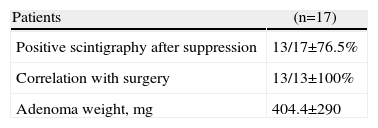
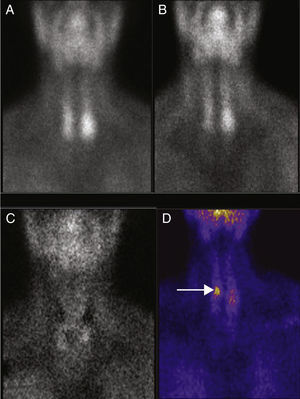
Scintigraphy after thyroxin suppression was positive in 13 of the 17 patients (76.5%) (Table 2, Fig. 1). The other 4 patients (23.5%) had no MIBI images suggestive of adenoma.
(A) 99mTc-sestamibi, planar scintigraphic image (early phase). (B) Image at late phase. (C) Image after performing pertechnetate subtraction. No images suggesting possible adenoma are observed. (D) Subtraction technique after suppression of the thyroid function. There is an area with marked uptake near the upper pole of the right thyroid lobe (arrow) which was later confirmed as an adenoma.
The 13 patients with a positive scan after suppression underwent a minimally invasive selective parathyroidectomy. The adenoma was always found in the location specified by the MIBI. There was no need to convert to conventional cervicotomy in any patient and there were no complications. An ultrasound scan was positive in 8 of these 13 patients and in 6 coincided with the position marked by the MIBI, and therefore the location of the adenoma during surgery (a false positive result was found for 2 patients, probably due to concomitant thyroid nodular disease). Although, the MIBI and ultrasound were not in agreement regarding the position of the adenoma in 7 patients, the initial approach was minimally invasive, due to the high positive predictive value of MIBI in our hospital2 (over 95%), without any other imaging test or intraoperative determination of PTH.
All patients maintained normocalcaemia 1 month and 6 months after surgery. In these patients, the ultrasound correctly located the adenoma in 9 cases and showed no suspicious image in 4 patients. The average weight of the adenomas was 404.4±290mg.
For the 4 patients with a negative MIBI after thyroid suppression, the ultrasound did not detect the adenoma. All patients underwent surgery by bilateral neck exploration. Two of them had a single adenoma (1 in the retro-oesophageal position), another patient had multiglandular disease, and the adenoma causing the disease in another patient was not found.
ConclusionsSurgical treatment of patients with PHPT has changed in the last 20 years towards a selective parathyroidectomy with a minimally invasive approach. This has resulted in a fast, patient-friendly and effective surgery in experienced hands. This type of intervention can be performed in up to 75% of cases, even under local anaesthesia.7 However, it requires previous agreement on the precise localisation, preferably by 2 imaging techniques: one providing anatomical information and the other functional information about the possible adenoma by MIBI. Almost a decade ago, Royal et al.6 published a study suggesting improved localisation by MIBI after suppressing the thyroid function in patients who had had a previous negative scintigraphic image. There has been no other study published since then either to confirm or refute these findings, except for a letter to the editor some years later casting doubt on these results.8
In hospitals with reference endocrine surgery units, the sensitivity of MIBI must be above 80% and the false negative rate less than 15%. In our hospital, the sensitivity of MIBI in patients with PHPT is above 95%, with a positive predictive value of 97%, allowing us to use location by scintigraphy as the primary preoperative imaging test, often as the only test. The main concern of nuclear medicine specialists, endocrinologists and endocrine surgeons is to find ways to minimise the rate of false negatives. Following the aforementioned Royal et al.’s6 study, our study found a MIBI sensitivity of 76% in patients with previously negative scans, after repeating the test under the suppression of thyroid function. Furthermore, for all the patients whose new scan was positive, the adenoma was found during surgery in the area shown by the MIBI (a positive predictive value of 100%). Moreover, all patients benefited from a minimally invasive approach.
Although the mechanism by which this technique can increase the uptake of tracer is not completely clear, there is a suggestion that it is due to the suppression of the thyroid cell metabolism, leading to increased uptake by the adenoma combined with less interference from the thyroid gland when performing the scan. Although questioned by some authors, this explanation seems to account for the results of both the Royal et al.’s study and our own.
However, more patients are required to confirm these results and clarify the cellular mechanism by which thyroxine-induced suppression improves the sensitivity of MIBI in patients with previous negative results. The results obtained so far are optimistic and may lead to different studies on the subject. Minimally invasive selective parathyroidectomy is an effective technique with a low complication rate in experienced hands. However, it requires accurate preoperative localisation, primarily via scintigraphy. Therefore, our efforts must be aimed at improving the outcomes of this technique to get the largest possible number of patients benefiting from this type of surgery.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Gómez-Ramírez J, et al. Supresión tiroidea en pacientes con hiperparatiroidismo primario: ¿mejora la localización gammagráfica preoperatoria? Cir Esp. 2011;89:595–8.