Walled-off pancreatic necrosis is one of the most feared complications of severe acute pancreatitis. Although most cases evolve favorably with conservative management, up to one-quarter of patients will require interventional techniques1,2. The management of peripancreatic collections has evolved in recent years, and the benefits of the step-up approach have been widely demonstrated3–5. The current debate in this field focuses on demonstrating the superiority of endoscopic necrosectomy (EN) over video-assisted retroperitoneal debridement (VARD), or vice versa6. We present the case of a patient with severe acute pancreatitis and large walled-off necrosis that required the combined use of EN and VARD for its resolution.
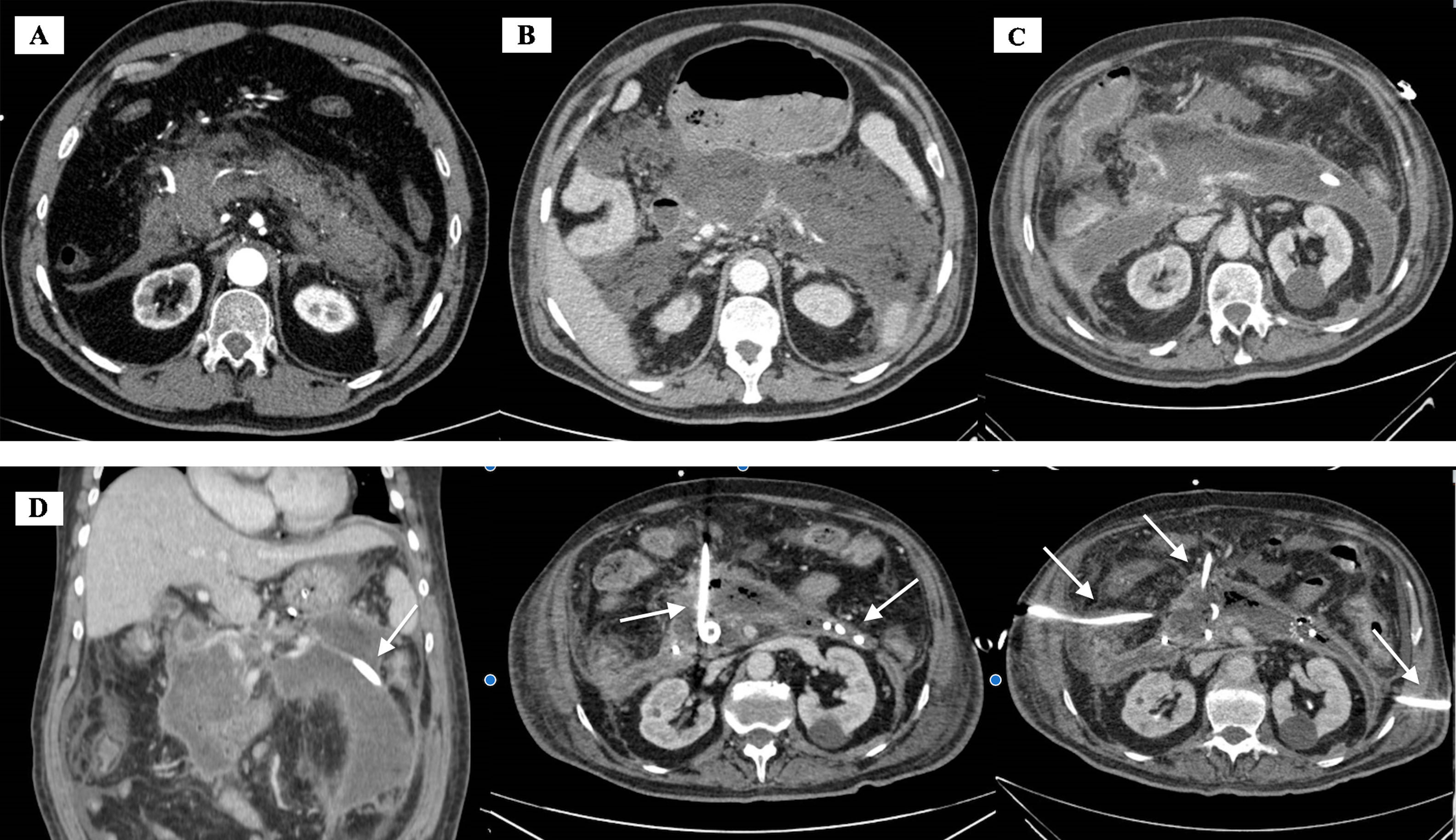
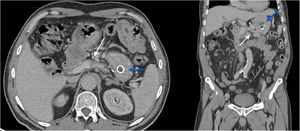
The patient is a 69-year-old man with arterial hypertension and hyperuricemia, who came to the emergency room due to sudden and intense abdominal pain in the epigastrium. We observed notable impairment of his general condition and signs of peripheral hypoperfusion. Blood pressure was 153/95 mmHg; heart rate 86 bpm. He maintained an oxygen saturation of 89%–92%, with an inspired oxygen fraction of 21%. Intra-abdominal pressure was 27 mmHg, measured indirectly. His abdomen was very distended, with generalized tenderness and muscle guarding. Lab work-up showed normal renal function and ions, alanine aminotransferase 256 U/L, aspartate aminotransferase 518 U/L, total bilirubin 1.63 mg/dL (direct 0.96 mg/dL), amylase 6.396 U/L, lipase 21 200 U/L, C-reactive protein 51 mg/dL, leukocytes 262 900 μL (80% neutrophils) and coagulation in normal ranges. Abdominal computed tomography (CT) scan was performed 48 h after admission, showing images compatible with pancreatitis, with focal areas of necrosis and gallstones (Fig. 1A). During the first month of hospitalization in the Intensive Care Unit, he presented multiple organ failure and required non-invasive mechanical ventilation, hemofiltration, and high doses of vasoactive drugs. Due to suspected superinfection of the collection, empirical antibiotic therapy was started with piperacillin/tazobactam 4/0.5 every 8 h. The patient then presented an episode of upper gastrointestinal bleeding and endoscopy was performed, during which a large clot was observed with no other observable findings. An abdominal CT scan showed hemorrhage from the left gastric artery, which was embolized. The CT scan 22 days after admission also revealed a necrosis of more than 80% of the pancreatic parenchyma and a peripancreatic necrotic collection (Fig. 1B). We then decided to insert a percutaneous pigtail catheter under CT guidance. Klebsiella pneumoniae was isolated in the fluid culture, which was treated with 1 g ceftriaxone every 24 h according to the antibiogram. During the next 30 days of hospitalization, the patient continued to present a torpid evolution (improvement after the placement of the drain tube and progressive worsening afterwards). The drains were changed twice for others with a larger diameter, but the evolution was similar (Fig. 1C and D). Orotracheal intubation was required as a consequence of nosocomial pneumonia.
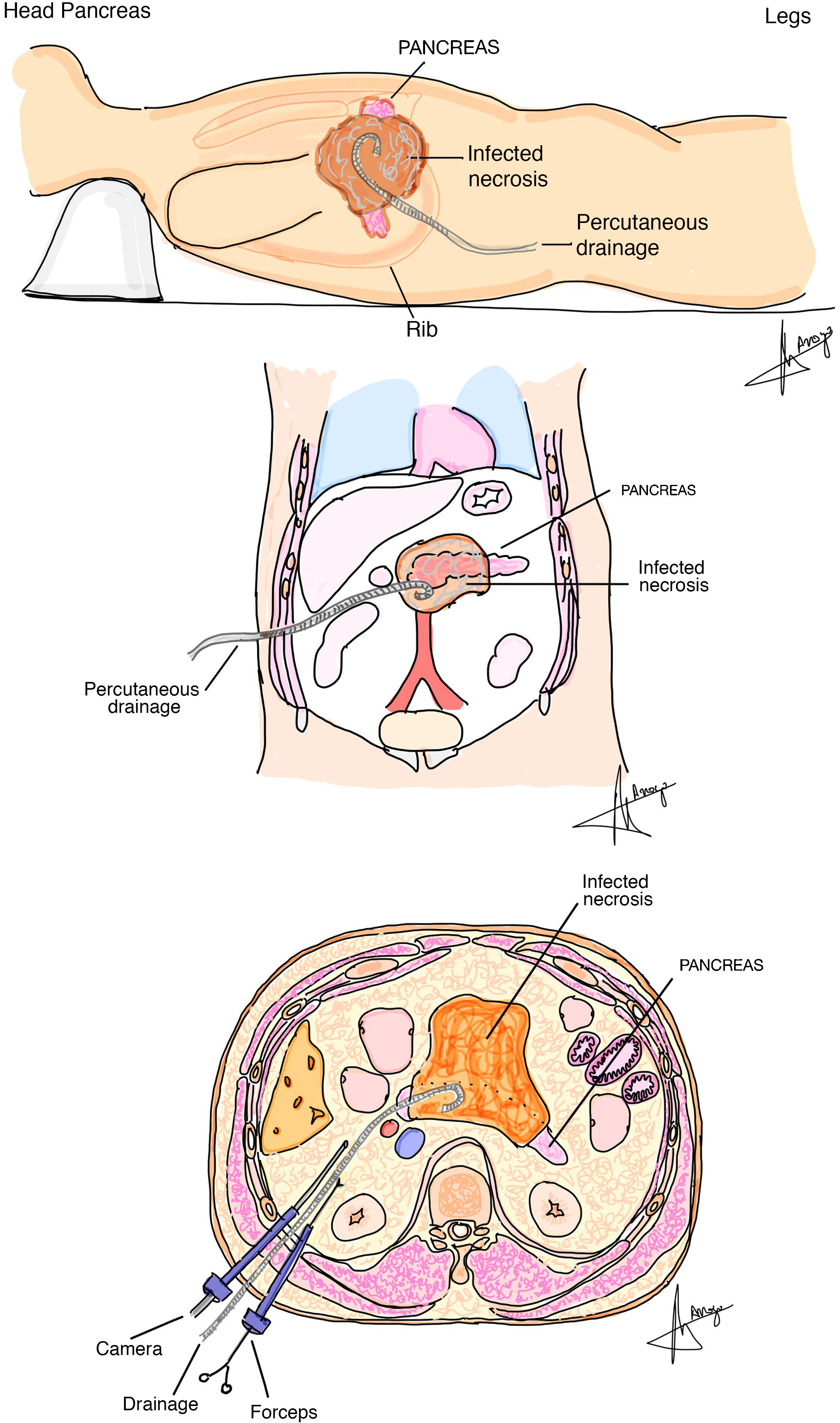
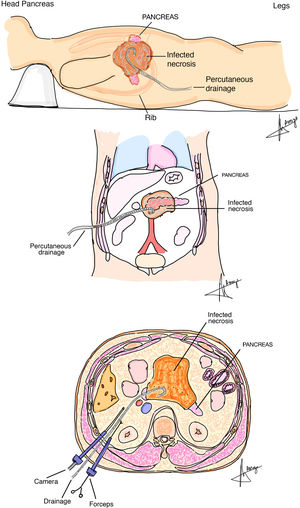
After 62 days, the follow-up CT scan showed an increase in the peripancreatic collection. We decided to carry out EN. A metallic diabolo stent was placed, and a double pigtail catheter was inserted through it. Two successive sessions of EN were carried out with an infusion of 0.3% hydrogen peroxide. In the 3rd session, a 7 Fr nasocystic catheter was inserted, through which saline lavages were carried out. During the 4th session, the stent was accidentally moved, which required replacement. Evolution continued to be torpid. Radiologically, the part of the collection located around the head of the pancreas continued to grow, extending to the right paracolic gutter. We decided to perform VARD (Fig. 2). The collection was accessed by following the pigtail catheter in place. Through a 12 mmHg trocar, 6−8 mmHg retro-pneumoperitoneum was created, and an auxiliary 5 mmHg trocar was inserted. The purulent contents were aspirated, and the necrotic material was removed. Aspiration lavage of the cavity was done with saline and povidone iodine. A grooved 19 Fr Blake silicone drain was placed inside the cavity, which was washed out with saline and urokinase every 12 h.
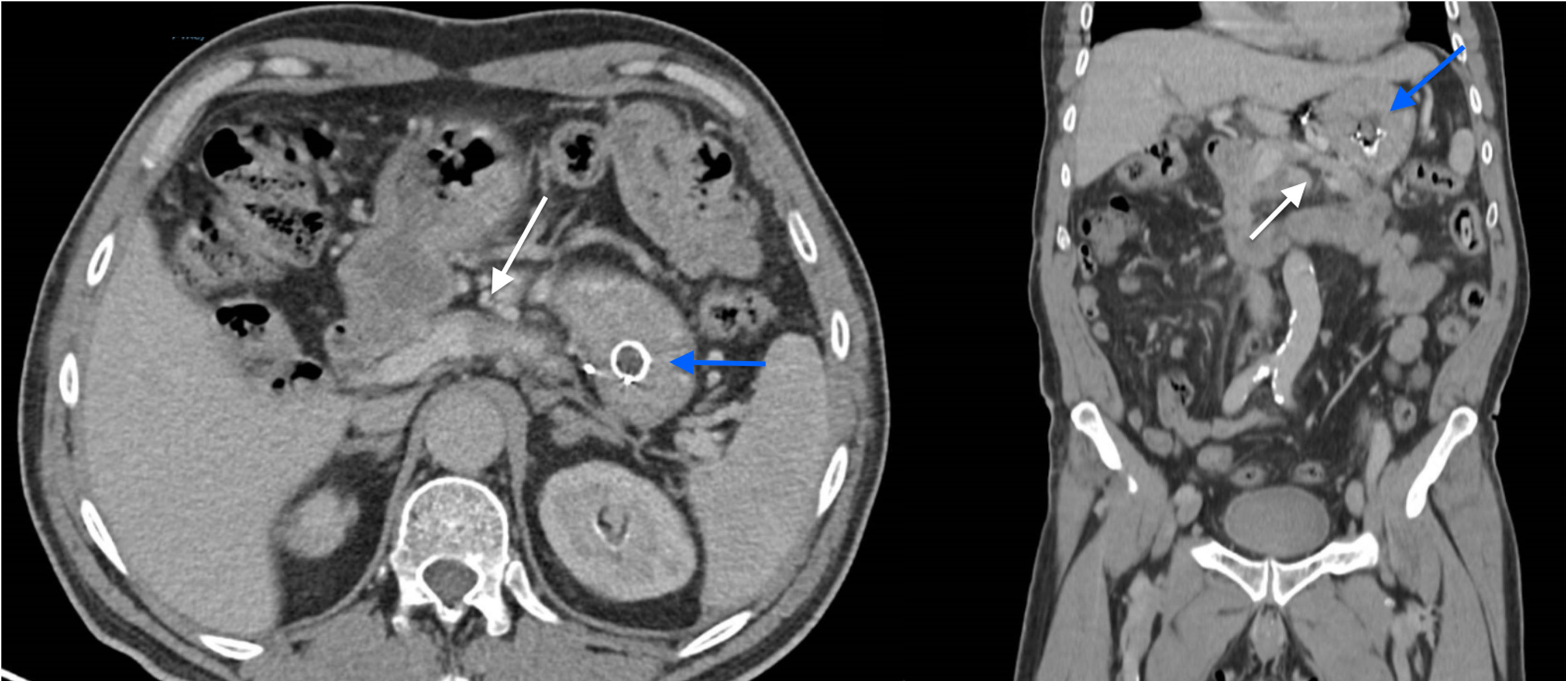
The patient progressed favorably. The pigtail catheter was removed on the 10th day and the Blake drain on the 16th day. On the 20th postoperative day, the patient was transferred to the hospital ward, and after 190 days of total hospital stay, he was discharged. The gastric prosthesis was removed 9 months later, after having verified that the collections had resolved correctly (Fig. 3). The patient is currently asymptomatic and under treatment for pancreatic insufficiency.
An important factor in the management of patients with severe acute pancreatitis is the correct characterization of pancreatic collections. It is recommended to wait until the definitive conformation of the wall (generally 4 weeks) before attempting any invasive technique7,8 (Fig. 1A–C). Within the step-up approach, there are different accepted routes to perform necrosectomy. One of them is the VARD technique. This involves stepwise management, since radioguided placement of a catheter inside the collection is necessary beforehand. There are many studies that have demonstrated a reduction in complications and mortality compared to open surgery5,9. In addition, EN is also evolving as a safe technique within stepwise management. The advent of lumen-apposing metal stents seems to reduce the number of complications, especially migration, as in our patient10. The TENSION study (multicenter, controlled and randomized) found no differences in terms of morbidity and mortality between the two techniques, although it did demonstrate superiority of the endoscopic technique in terms of reducing pancreatic fistula and hospital stay compared to VARD10. In our case, however, both techniques used in conjunction for the correct resolution of the symptoms. Thus, EN was more suitable for retrogastric collections, and VARD was more useful in the paracolic gutters.
In conclusion, the combination of different necrosectomy techniques should be considered a tool for the management of severe pancreatitis and should be considered part of the multidisciplinary management of patients in hospitals with extensive experience.
Please cite this article as: Cerrato Delgado S, Valverde Martinez A, Gómez Sánchez T, Fierro Aguilar A, Pacheco García JM. Step-up approach en pancreatitis necrosante grave: combinación de desbridamiento retroperitoneal videoasistido y necrosectomía endoscópica. Cir Esp. 2022;100:52–55.