Due to the current pandemic of respiratory disease known as coronavirus disease 2019 (COVID-19) caused by the SARS-CoV-2 virus, many patients with confirmed or suspected COVID-19 infection will require elective surgery, surgery that cannot be postponed, or emergency surgical treatment. In these situations, special measures need to be adopted in order to minimize the possibility of transmission between patients, exposure of healthcare personnel and the development of postoperative complications. This document explains the main principles to consider when managing confirmed or suspected COVID-19 patients during evaluation as well as when surgical treatment is required.
Debido a la actual pandemia de enfermedad respiratoria denominada enfermedad por coronavirus 2019 (COVID-19) causada por el virus denominado SARS-CoV-2, numerosos pacientes con confirmación o sospecha de COVID-19 precisarán tratamiento quirúrgico electivo inaplazable o urgente. Estas situaciones requieren la adopción de medidas especiales da cara a minimizar la posibilidad de contagio entre pacientes, la exposición del personal sanitario y el desarrollo de complicaciones postoperatorias. En el presente documento se explican las principales medidas a tener en cuenta en caso de atención a pacientes COVID-19 o sospecha tanto durante su evaluación como en caso de requerir tratamiento quirúrgico.
Health systems around the world are responding to a pandemic of respiratory disease known as coronavirus disease 2019, or COVID-19. The outbreak is caused by a new coronavirus that has been dubbed SARS-CoV-2. Due to its rapid expansion, it is very likely that patients requiring surgery will have confirmed or suspected COVID-19.
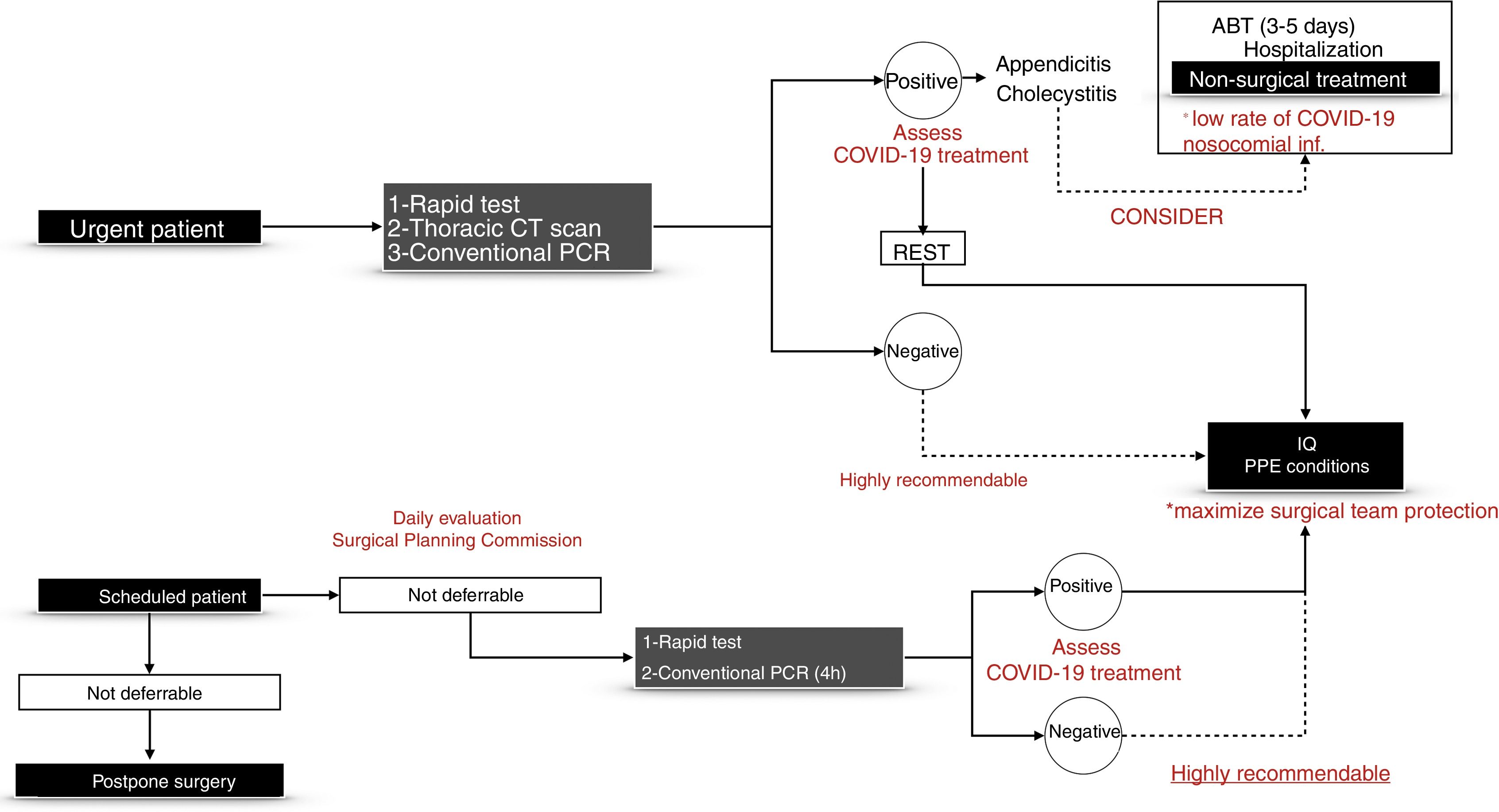
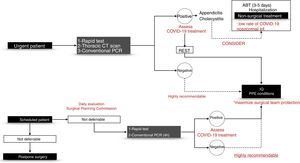
The scenarios in which they are contemplated are emergency surgeries and elective procedures that cannot be delayed. The indication for urgent surgery should be individualized in all cases and based on a diagnosis with the greatest possible certainty. In many cases, the possibility of conservative treatments that have been proven to be safe options should be evaluated (e.g. antibiotic treatment in young patients with incipient acute appendicitis, conservative treatment of certain acute cholecystitis, etc.). In view of the important repercussions of the pandemic and COVID-19 infection, the Surgical Infection Division of the Spanish Association of Surgeons (AEC, Asociación Española de Cirujanos) has issued this document of recommendations for the surgical management of patients with suspected or confirmed COVID-19 infection.
MethodsWe have conducted a narrative review of the literature using PubMed and have also consulted the websites of the World Health Organization (WHO), Centers for Diseases for Control and Prevention (CDC), European Center for Disease Prevention and Control (ECDC), Society for Healthcare Epidemiology of America and Infectious Diseases Society of America. A bibliographic search was carried out with the following keywords: COVID-19; SARS-CoV-2; surgery; operation; surgical protocol; and guidance. The bibliographic search was performed by all the authors, who selected, summarized, wrote and reached a consensus on the recommendations.
ResultsBasic Characteristics of the Virus and Associated Clinical SymptomsCoronaviruses are a family of viruses that cause disease in people or that circulate among animals. The COVID-19 strain causing the current outbreak (elevated to the category of pandemic and health emergency by the WHO) was first identified in Wuhan, in the Chinese province of Hubei, in December 2019. With more than 500000 cases worldwide and 60000 in Spain in March 2020,1 this infection occurs in the form of fever, dry cough and mild dyspnea in most cases, although it can evolve into severe pneumonia and eventual acute respiratory distress. In this regard, it is very similar to severe acute respiratory syndrome (SARS) described in 2003 and the Middle East respiratory syndrome (MERS) of 2012.2,3 It is spread through respiratory droplets from coughing or sneezing, similar to how flu and other respiratory viruses spread.
Both the high rate of contagion observed and the pathogenesis of the disease itself depend on the anchoring of the virus to human cells (through the receptor-binding domain of transmembrane glycoprotein S), recognition of cellular receptors (specifically angiotensin-converting enzyme 2) and internalization into the cytoplasm using a host transmembrane serine protease (TMPRSS).4 As for involvement of the gastrointestinal tract, fecal–oral transmission has not yet been completely ruled out. Extrarespiratory involvement by COVID-19 is very rare and is usually restricted to nonspecific symptoms (nausea, vomiting, epigastric discomfort, etc.). Pancreatic involvement is exceptionally rare, as is hepatotoxicity, mainly due to some of the treatments used.5,6
Ethical IssuesSurgical teams must treat all patients with COVID-19 who require surgical treatment that cannot be delayed. It is recommended that the surgical teams designated to treat these patients should have extensive and appropriate training. Therefore, surgical teams should be created with surgical technologists, surgeons and anesthetists who are properly trained for any type of urgent surgery. These teams should receive extensive theoretical and practical training in simulated emergency situations, management of protective equipment and surgical protocol. Furthermore, healthcare institutions are obligated to provide the necessary resources for adequate prevention measures for their staff, which should be applied in accordance with current regulations and clinical protocols.
Precautions for Examining Patients With Suspected or Confirmed COVID-19 InfectionPatients are referred to the General Surgery Service from two branches: emergency department and hospital wards. Both settings will have a pre-established location for this type of patient in accordance with the protocols of each hospital.
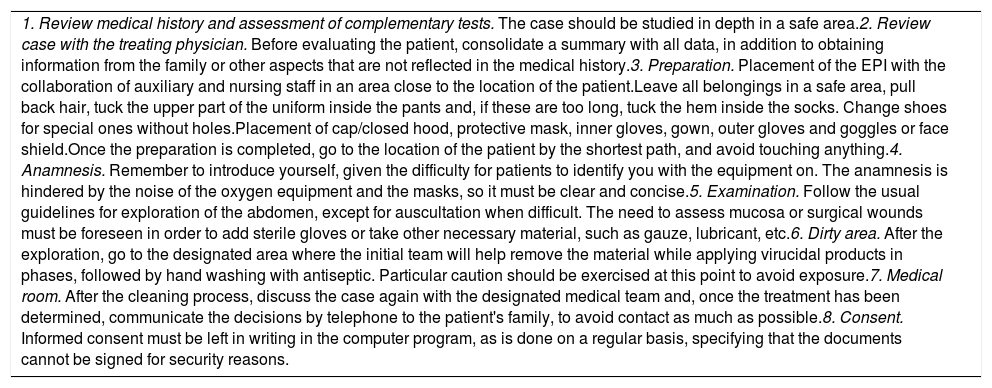
It is essential to divide the patients into two groups: suspected COVID-19 group, and confirmed COVID19 group. Although the measures to be taken when evaluating these patients are very similar, a confirmed diagnosis can modify the therapeutic options. Table 1 summarizes important aspects to consider in the different stages.
Precautions for the Study, Anamnesis and Examination of Patients With Suspected or Confirmed COVID-19 Infection.
| 1. Review medical history and assessment of complementary tests. The case should be studied in depth in a safe area.2. Review case with the treating physician. Before evaluating the patient, consolidate a summary with all data, in addition to obtaining information from the family or other aspects that are not reflected in the medical history.3. Preparation. Placement of the EPI with the collaboration of auxiliary and nursing staff in an area close to the location of the patient.Leave all belongings in a safe area, pull back hair, tuck the upper part of the uniform inside the pants and, if these are too long, tuck the hem inside the socks. Change shoes for special ones without holes.Placement of cap/closed hood, protective mask, inner gloves, gown, outer gloves and goggles or face shield.Once the preparation is completed, go to the location of the patient by the shortest path, and avoid touching anything.4. Anamnesis. Remember to introduce yourself, given the difficulty for patients to identify you with the equipment on. The anamnesis is hindered by the noise of the oxygen equipment and the masks, so it must be clear and concise.5. Examination. Follow the usual guidelines for exploration of the abdomen, except for auscultation when difficult. The need to assess mucosa or surgical wounds must be foreseen in order to add sterile gloves or take other necessary material, such as gauze, lubricant, etc.6. Dirty area. After the exploration, go to the designated area where the initial team will help remove the material while applying virucidal products in phases, followed by hand washing with antiseptic. Particular caution should be exercised at this point to avoid exposure.7. Medical room. After the cleaning process, discuss the case again with the designated medical team and, once the treatment has been determined, communicate the decisions by telephone to the patient's family, to avoid contact as much as possible.8. Consent. Informed consent must be left in writing in the computer program, as is done on a regular basis, specifying that the documents cannot be signed for security reasons. |
According to the latest studies, it appears that COVID-19 basically causes diffuse alveolar damage associated with direct damage to pneumocytes, unlike other infections that cause damage due to inflammatory hyperresponsiveness and endothelial damage.7 Furthermore, it gives rise to a cytokine cascade similar to that found in bacterial sepsis or even hemophagocytic lymphohistiocytosis. All this translates into nonspecific respiratory symptoms with fever that appears frequently and especially in the severest cases. Up to 10% of patients may also experience digestive symptoms, such as diarrhea or nausea.5,8
In terms of analytical parameters, unlike bacterial sepsis, COVID-19 does not cause an elevated white blood cell count or classic neutrophilia. It has been associated with lymphopenia in approximately 80% of patients and mild thrombocytopenia in cases with a worse prognosis.2 Nonspecific elevated D-dimer levels are also frequent.
It is important to note that procalcitonin is not elevated in cases of COVID-19 infection according to the studies carried out to date, and procalcitonin levels less than 0.5ng/mL have been found in 95% of the patients analyzed. This point is important with regards to sepsis, where it is a fundamental marker, especially in systemic bacterial infections. However, C-reactive protein (CRP), as in the case of sepsis, can become elevated in a direct relationship with the prognosis and severity of the disease, as high levels are found in cases of hypoxemia and mortality.
Diagnostic Tests for COVID-19 Infection in Patients Requiring Elective Surgery That Cannot Be DelayedRoutine testing for COVID-19 is recommended before urgent or elective surgery.9Fig. 1 shows the proposed management for urgent and elective surgical patients. These recommendations are subject to the evolution over time of the pandemic and the resources of each geographic area.
Management PathwayOnly preliminary data and some reported experiences are available, which are restricted to case reports or series of cases. The recommendations for surgery in patients with viral diseases that are highly transmissible through fluids recommend minimally invasive accesses to minimize the risk of infection of members of the surgical team.10 In the case of COVID-19, infection occurs by air and contact, although the fecal–oral route has not been ruled out. Thus, the risk of aerosolization of particles and fluids must also be considered, although until now the evidence related to the presence of viruses in the pneumoperitoneum during laparoscopy is restricted to the experience with hepatitis B virus.
During gastrointestinal surgery, the use of the scalpel and opening the digestive tract can generate aerosols. Laparoscopy involves the interposition of a physical barrier between the surgeon and the possible source of infection, avoiding occupational exposure and cross infection. The use of hand-assisted surgery through a properly sealed auxiliary port could be considered if the time of the procedure can be reduced without compromising the oncological/functional result. Equipment should be thoroughly checked before surgery. Attempt to minimize the number, size, and size-match of the incision for the trocars. Use central negative pressure systems, and try to evacuate the smoke only once. Constant pressure insufflation systems can be used, and complete exsufflation is recommended before making an assistance incision, if necessary.11,12 As for surgeries in which TaTME, TAMIS or TEM approaches have been used (which have been conducted with extreme precautions in China), the current situation discourages their use due to the high risk of aerosolization and prolonged direct exposure of the surgeon during the perineal stage.13 Likewise, it is essential to remember that the use of stomata (definitive and temporary) generates another possible source of transmission that must be taken into account when cared for by both health workers and family members.
Therefore, it is recommended to prioritize the approach that is most beneficial for the patient, regardless of their COVID-19 infection. In cases where the laparoscopic route is used, protection measures of the airway and mucous membranes should always be maximized, and special precautions will be taken to avoid direct exposure when gas is discharged (evacuations, final exsufflation, etc.). Likewise, although there is no evidence in this regard, the use of smoke filters in the cannulae of each of the laparoscopic ports would be advisable, when available.
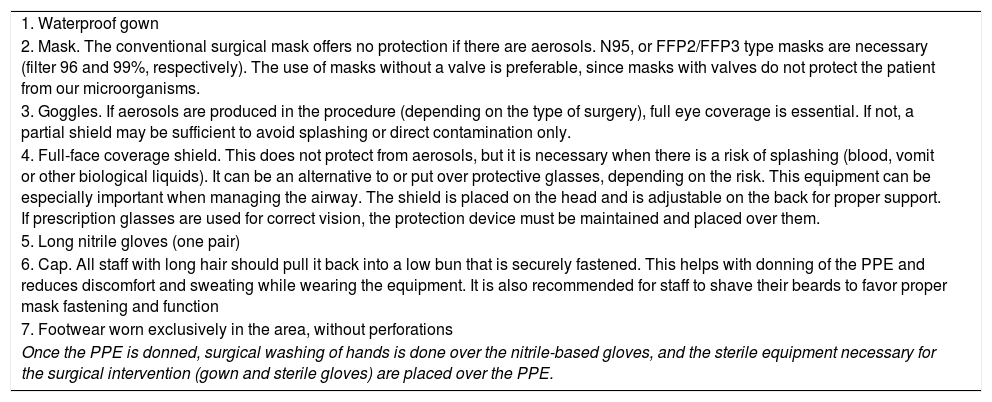
Precautions for Surgical Procedures in COVID-19-Positive Patients14–17In the case of a confirmed positive patient, personal protective equipment (PPE) should be used in conjunction with surgical clothing to ensure adequate protection of operating-room personnel. Even in unconfirmed cases, in the current context of a pandemic all patients should be assumed positive, taking the same protective measures to avoid unnecessary exposure of healthcare staff. There are different types of protective equipment, but the basic elements of protection necessary to be able to carry out a surgical operation under adequate safety conditions are described below.
Elements of Personal Protective Equipment (PPE)PPE are necessary in any procedure considered “close contact”, which includes surgical interventions as well as other operating room procedures (intubation, regional anesthesia, catheterization, etc.). Personal protection equipment, as established by Spanish Royal Decree 773/1997 regarding usage, provides effective protection against infection, without causing additional risks or unnecessary discomfort. The equipment necessary is summarized in Table 2. It is essential for the entire surgical team to have been previously trained in the placement and supervised removal of PPE before performing an actual surgical procedure. The collaboration of all members of the surgical team with each other is also very important. There must be trained substitutes available (from all levels) in case of any unforeseen event (intolerance of PPE, dizziness due to excess heat, etc.). PPE must completely cover the skin, especially the high-risk areas of the body: nostrils, mouth and eyes. Aerosols can be produced during surgical interventions, so PPE must protect against this circumstance. Surgical staff who must use this maximum protection in the operating room include the following (which may vary once all the transmission mechanisms of COVID-19 are determined): main surgeon and assistant; anesthetist and assistant (doctor or nurse); instrument nurse. The following do not need a maximum protection PPE (a surgical mask would suffice, without goggles or a face shield): circulating nurses and operating room assistant (unless they approach the patient during maneuvers at risk of generating aerosols).
Description of Personal Protective Equipment (PPE).
| 1. Waterproof gown |
| 2. Mask. The conventional surgical mask offers no protection if there are aerosols. N95, or FFP2/FFP3 type masks are necessary (filter 96 and 99%, respectively). The use of masks without a valve is preferable, since masks with valves do not protect the patient from our microorganisms. |
| 3. Goggles. If aerosols are produced in the procedure (depending on the type of surgery), full eye coverage is essential. If not, a partial shield may be sufficient to avoid splashing or direct contamination only. |
| 4. Full-face coverage shield. This does not protect from aerosols, but it is necessary when there is a risk of splashing (blood, vomit or other biological liquids). It can be an alternative to or put over protective glasses, depending on the risk. This equipment can be especially important when managing the airway. The shield is placed on the head and is adjustable on the back for proper support. If prescription glasses are used for correct vision, the protection device must be maintained and placed over them. |
| 5. Long nitrile gloves (one pair) |
| 6. Cap. All staff with long hair should pull it back into a low bun that is securely fastened. This helps with donning of the PPE and reduces discomfort and sweating while wearing the equipment. It is also recommended for staff to shave their beards to favor proper mask fastening and function |
| 7. Footwear worn exclusively in the area, without perforations |
| Once the PPE is donned, surgical washing of hands is done over the nitrile-based gloves, and the sterile equipment necessary for the surgical intervention (gown and sterile gloves) are placed over the PPE. |
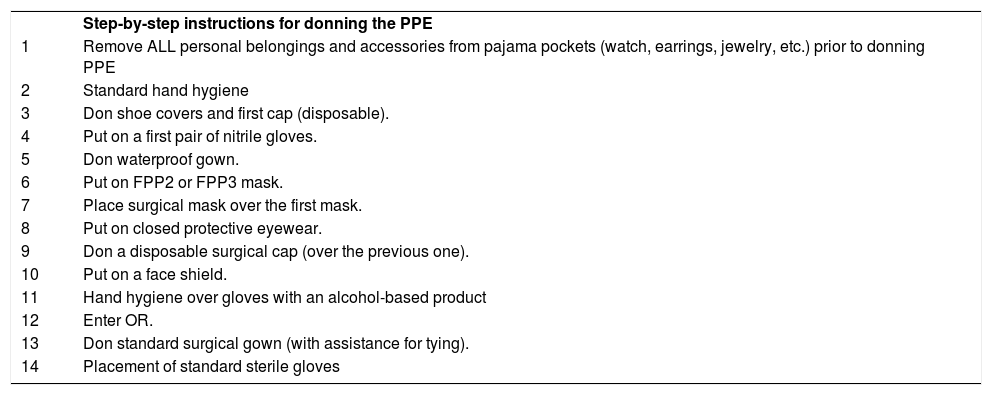
The sequence for these maneuvers is shown in Tables 3 and 4 and in Appendix B with material from the CDC. It is essential to doff the equipment calmly, slowly, avoiding sudden movements and under the supervision of a trained partner. Ideally, personnel who have been in the operating room should remove the PPE one by one under the supervision of an observer with a checklist. This should be done as far away from the patient as possible and near the door. A large container must be available to dispose of PPE, as well as alcoholic disinfectant for hands and surfaces. It may be useful to set up a ‘dirty’ room to remove the equipment, with sufficient space.
PPE Donning Sequence.
| Step-by-step instructions for donning the PPE | |
| 1 | Remove ALL personal belongings and accessories from pajama pockets (watch, earrings, jewelry, etc.) prior to donning PPE |
| 2 | Standard hand hygiene |
| 3 | Don shoe covers and first cap (disposable). |
| 4 | Put on a first pair of nitrile gloves. |
| 5 | Don waterproof gown. |
| 6 | Put on FPP2 or FPP3 mask. |
| 7 | Place surgical mask over the first mask. |
| 8 | Put on closed protective eyewear. |
| 9 | Don a disposable surgical cap (over the previous one). |
| 10 | Put on a face shield. |
| 11 | Hand hygiene over gloves with an alcohol-based product |
| 12 | Enter OR. |
| 13 | Don standard surgical gown (with assistance for tying). |
| 14 | Placement of standard sterile gloves |
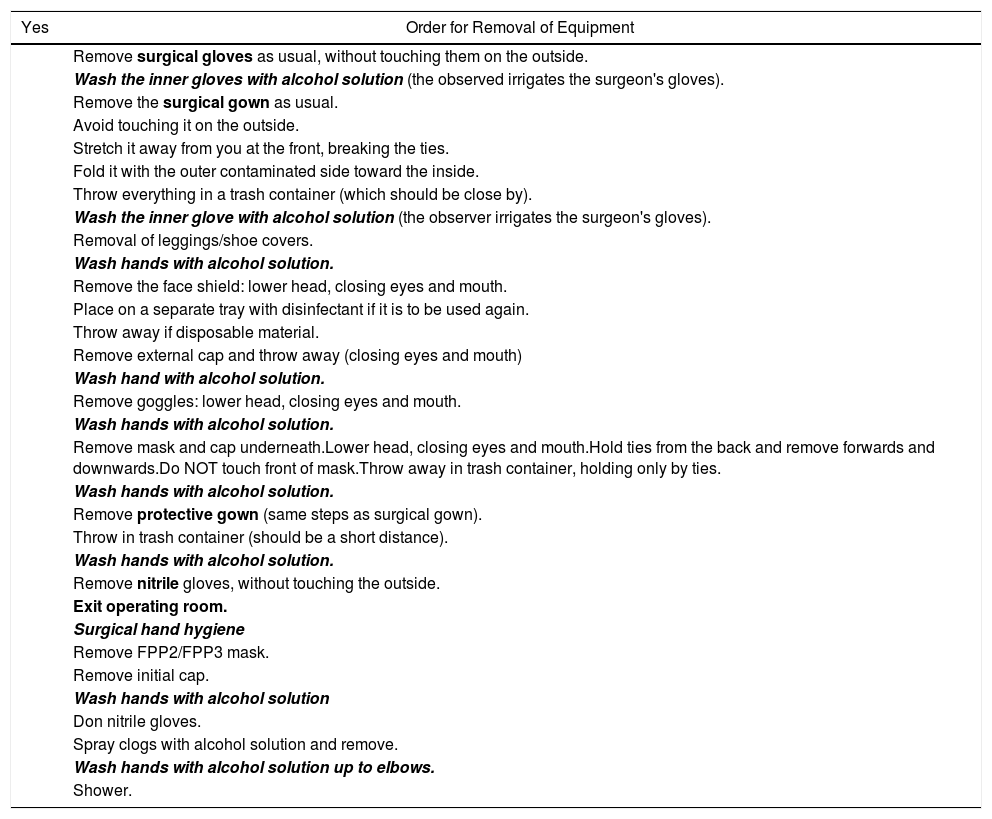
PPE Doffing Sequence.
| Yes | Order for Removal of Equipment |
|---|---|
| Remove surgical gloves as usual, without touching them on the outside. | |
| Wash the inner gloves with alcohol solution (the observed irrigates the surgeon's gloves). | |
| Remove the surgical gown as usual. | |
| Avoid touching it on the outside. | |
| Stretch it away from you at the front, breaking the ties. | |
| Fold it with the outer contaminated side toward the inside. | |
| Throw everything in a trash container (which should be close by). | |
| Wash the inner glove with alcohol solution (the observer irrigates the surgeon's gloves). | |
| Removal of leggings/shoe covers. | |
| Wash hands with alcohol solution. | |
| Remove the face shield: lower head, closing eyes and mouth. | |
| Place on a separate tray with disinfectant if it is to be used again. | |
| Throw away if disposable material. | |
| Remove external cap and throw away (closing eyes and mouth) | |
| Wash hand with alcohol solution. | |
| Remove goggles: lower head, closing eyes and mouth. | |
| Wash hands with alcohol solution. | |
| Remove mask and cap underneath.Lower head, closing eyes and mouth.Hold ties from the back and remove forwards and downwards.Do NOT touch front of mask.Throw away in trash container, holding only by ties. | |
| Wash hands with alcohol solution. | |
| Remove protective gown (same steps as surgical gown). | |
| Throw in trash container (should be a short distance). | |
| Wash hands with alcohol solution. | |
| Remove nitrile gloves, without touching the outside. | |
| Exit operating room. | |
| Surgical hand hygiene | |
| Remove FPP2/FPP3 mask. | |
| Remove initial cap. | |
| Wash hands with alcohol solution | |
| Don nitrile gloves. | |
| Spray clogs with alcohol solution and remove. | |
| Wash hands with alcohol solution up to elbows. | |
| Shower. |
Limit number of staff and movement in operating room. Complete with an external observer other than persons wearing PPE.
The removal sequence starts with the most contaminated element (gloves) and ends with the least contaminated (mask).
Activity Protocol in the Surgical AreaWe recommend the use of a checklist for the entire procedure that explicitly includes the patient's COVID-19 status. As for anesthesia, the AEC subscribes to the recommendations made in this regard by the Spanish Society of Anesthesiology, Resuscitation and Therapeutics of Pain (SEDAR).
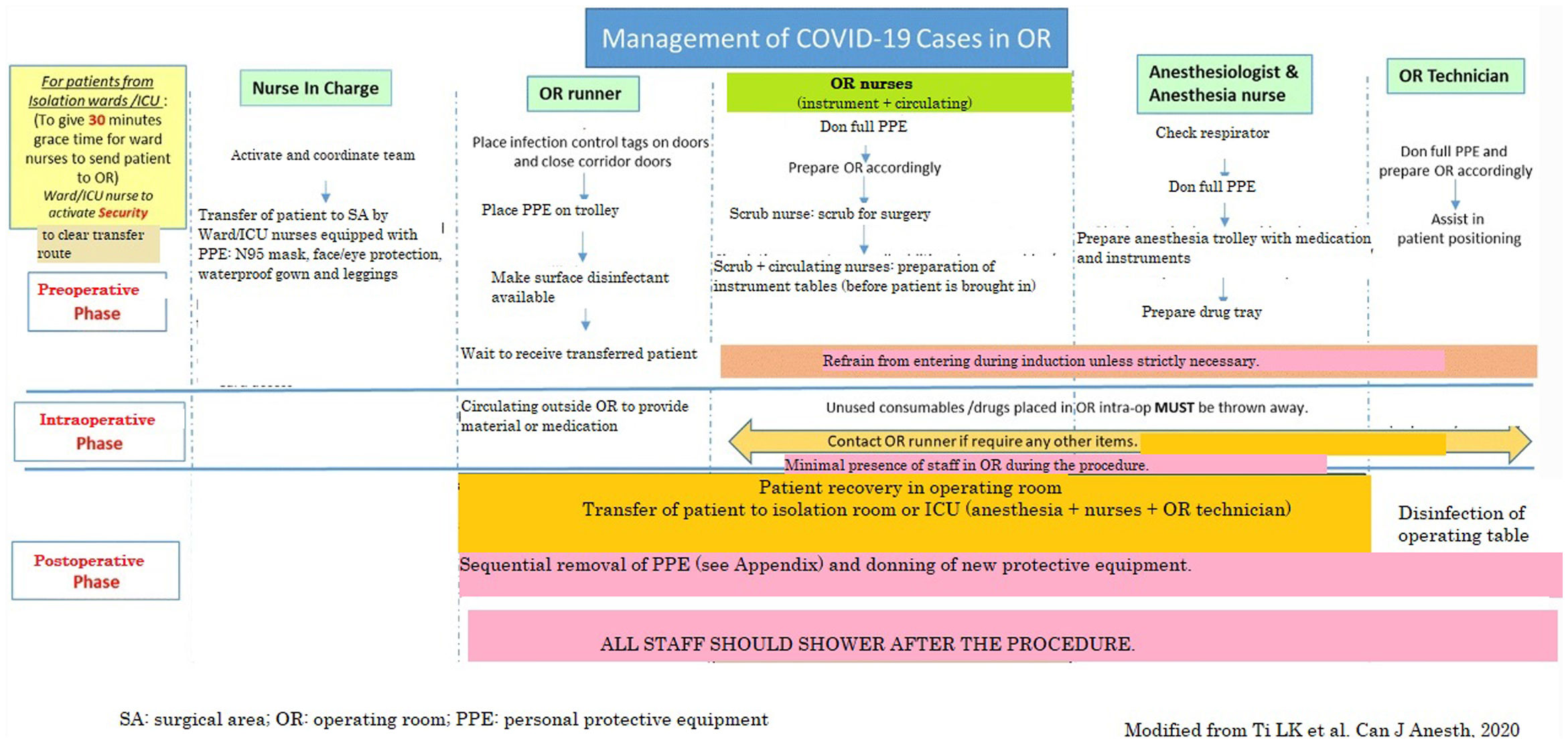
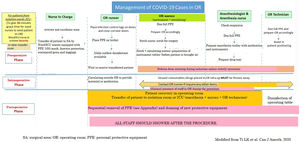
It is suggested that an operating room and all its equipment (respirator, etc.) should be designated exclusively for COVID-19 patients for use throughout the epidemic. Ideally it should be independent or away from other operating rooms. An adequate circuit should be planned to transfer these patients from the corresponding isolation area (ICU, ward, etc.) to the designated surgical area. Fig. 2 shows the surgical area protocol for surgical procedures involving patients with COVID-19, adapted from Ti et al.14
COVID-19 case management in the surgical area.
SA: surgical area; PPE: personal protective equipment; OR: operating room.
Source: Modified from Ti et al.14
Limit the number of medical professionals in the operating room and their movements as much as possible to reduce the risk of contamination.
Limit as much as possible the number of people who carry out maneuvers that carry the risk of generating aerosols.
Use disposable materials, as much as possible.
Keep the doors of the operating room closed, except for the circulation of personnel, patients and instruments. When absolutely necessary, keep them open as little as possible.
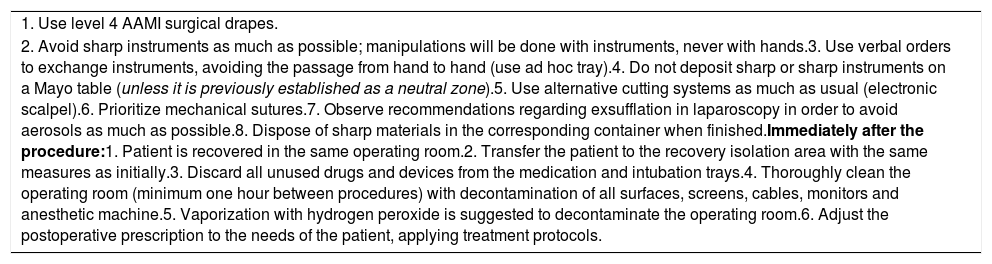
Open the guillotines during operation only if necessary (delivery of material). Table 5 shows the surgical protocol.
Surgical Protocol.
| 1. Use level 4 AAMI surgical drapes. |
| 2. Avoid sharp instruments as much as possible; manipulations will be done with instruments, never with hands.3. Use verbal orders to exchange instruments, avoiding the passage from hand to hand (use ad hoc tray).4. Do not deposit sharp or sharp instruments on a Mayo table (unless it is previously established as a neutral zone).5. Use alternative cutting systems as much as usual (electronic scalpel).6. Prioritize mechanical sutures.7. Observe recommendations regarding exsufflation in laparoscopy in order to avoid aerosols as much as possible.8. Dispose of sharp materials in the corresponding container when finished.Immediately after the procedure:1. Patient is recovered in the same operating room.2. Transfer the patient to the recovery isolation area with the same measures as initially.3. Discard all unused drugs and devices from the medication and intubation trays.4. Thoroughly clean the operating room (minimum one hour between procedures) with decontamination of all surfaces, screens, cables, monitors and anesthetic machine.5. Vaporization with hydrogen peroxide is suggested to decontaminate the operating room.6. Adjust the postoperative prescription to the needs of the patient, applying treatment protocols. |
No specific routine treatment is recommended. Antiviral treatment follows the same indications as for any patient infected with COVID-19. To date, only confirmed cases have been treated, recording in the medical record that a specific treatment has been proposed for which the patients have given their consent (at least verbally). Hydroxychloroquine and lopinavir/ritonavir are currently being used. In elderly and/or polymedicated patients, only hydroxychloroquine is preferred, although it should be avoided in case of liver disease. The most severe patients may also receive treatment with interferon β/tocilizumab, and even remdesivir has been considered.18–20 However, the degree of evidence for these treatments is very limited and based fundamentally on the experience accumulated to date.
Other recommended complementary measures are oxygen therapy and avoiding administering corticosteroids and nebulizers. Regarding the use of drugs that can alter the expression and/or function of the angiotensin-converting enzyme 2 (ACE2), the data are too preliminary to make any firm recommendations. In this case, the use of NSAIDs such as ibuprofen could be questioned, although there is no clear evidence in humans that it can favor the infection or worsen its course. Regarding the therapeutic management of a possible intra-abdominal infection, initially the recommended guidelines for this type of situation should not be modified, neither generally nor according to the protocols of each hospital.21 It is strongly recommended to check the interactions of antiviral drugs. There are currently online registries such as www.covid19-druginteractions.org where updated interactions can be easily consulted.
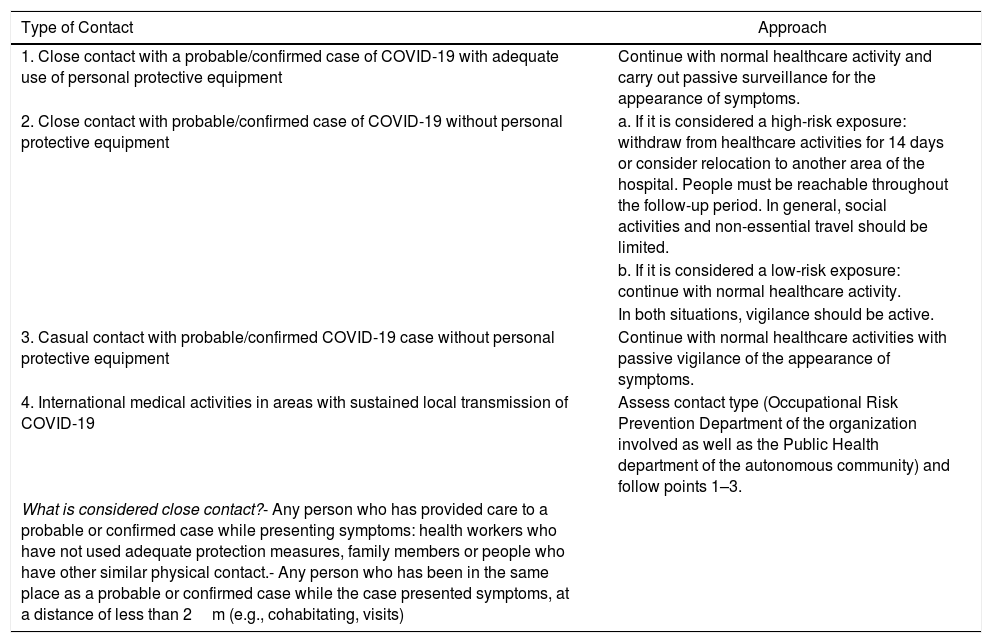
Approach to a Member of the Surgical Team With Suspected COVID-19 Infection9Any member of the healthcare staff who has had close contact with a patient under investigation with probable or confirmed of coronavirus infection should immediately notify the Preventive Medicine/Occupational Health/Occupational Risk Prevention Department of their hospital. This department will establish the approach to follow based on general and local recommendations as well as the corresponding hospital protocol. Depending on the presence of community transmission, active or passive surveillance protocols will be established.
Table 6 shows the definitions of epidemiological contacts and the approach to follow in each case. The hospital service in charge must carry out an individualized risk assessment, the result of which will be communicated to the Public Health services of the autonomous community. The evaluation must take into account the following aspects:
- A.
Type of exposure (e.g., procedures that generate aerosols, such as aspiration of the respiratory tract, intubation or bronchoscopy, resuscitation maneuvers, laboratory accidents)
- B.
Exposure time (more than 15min less than 2m away)
- C.
Service in which they carry out their healthcare activity (units with especially vulnerable patients, such as hematology, ICU, oncology or burn units)
Classification of Contact Types and Approach.
| Type of Contact | Approach |
|---|---|
| 1. Close contact with a probable/confirmed case of COVID-19 with adequate use of personal protective equipment | Continue with normal healthcare activity and carry out passive surveillance for the appearance of symptoms. |
| 2. Close contact with probable/confirmed case of COVID-19 without personal protective equipment | a. If it is considered a high-risk exposure: withdraw from healthcare activities for 14 days or consider relocation to another area of the hospital. People must be reachable throughout the follow-up period. In general, social activities and non-essential travel should be limited. |
| b. If it is considered a low-risk exposure: continue with normal healthcare activity. | |
| In both situations, vigilance should be active. | |
| 3. Casual contact with probable/confirmed COVID-19 case without personal protective equipment | Continue with normal healthcare activities with passive vigilance of the appearance of symptoms. |
| 4. International medical activities in areas with sustained local transmission of COVID-19 | Assess contact type (Occupational Risk Prevention Department of the organization involved as well as the Public Health department of the autonomous community) and follow points 1–3. |
| What is considered close contact?- Any person who has provided care to a probable or confirmed case while presenting symptoms: health workers who have not used adequate protection measures, family members or people who have other similar physical contact.- Any person who has been in the same place as a probable or confirmed case while the case presented symptoms, at a distance of less than 2m (e.g., cohabitating, visits) |
Thus, once the exposure has been reported and the situation assessed by the corresponding department at the workplace, if the member of the surgical team does not present symptoms and is considered low risk, the current recommendation is to continue normal activities, while monitoring body temperature twice a day. Therefore, it is possible to continue carrying out scheduled and urgent surgical activity using the recommended protection measures for each case. In the event that symptoms appear, the Occupational Risk Prevention Department should be notified as soon as possible, as established in each autonomous community of Spain. The professional will withdraw from healthcare activity, the protocol for notification to the Public Health Department will be activated, and it will be considered a case under investigation.
Protocol in the Event of Biological Exposure of the Surgical TeamIn the event of exposure without PPE to a patient under investigation, with probable or confirmed COVID19 infection, the exposed staff should be considered close contact and will be managed as such, depending on the specific indications of each hospital. All exposed medical professionals should immediately contact the Preventive Medicine/Occupational Health/Occupational Risk Prevention Department at their medical center and follow the instructions that are indicated. To date, there have been no specific studies of post-exposure prophylaxis (PEP) for COVID-19.9 A retrospective study by Park et al. from 2019 on PEP for MERS in a limited number of healthcare professionals showed good results using a combination of antivirals (lopinavir/ritonavir plus ribavirin).22 However, it is a study with several probable biases in favor of PEP. At the present time, there is no evidence to recommend PEP for COVID-19.
FinancingNone declared.
Conflict of InterestsThe authors declare no conflict of interest.
Please cite this article as: Balibrea JM, Badia JM, Rubio Pérez I, Martín Antona E, Álvarez Peña E, García Botella S, et al. Manejo quirúrgico de pacientes con infección por COVID-19. Recomendaciones de la Asociación Española de Cirujanos. Cir Esp. 2020;98:251–259.