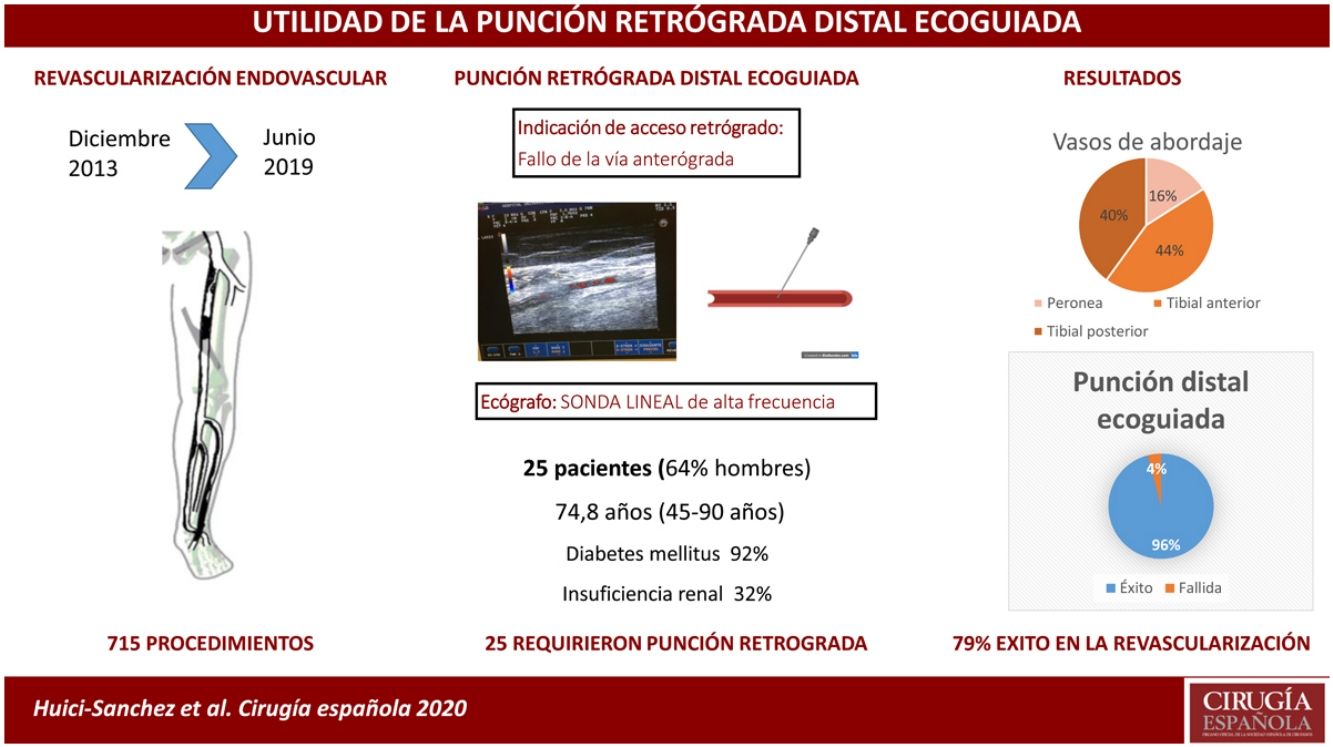
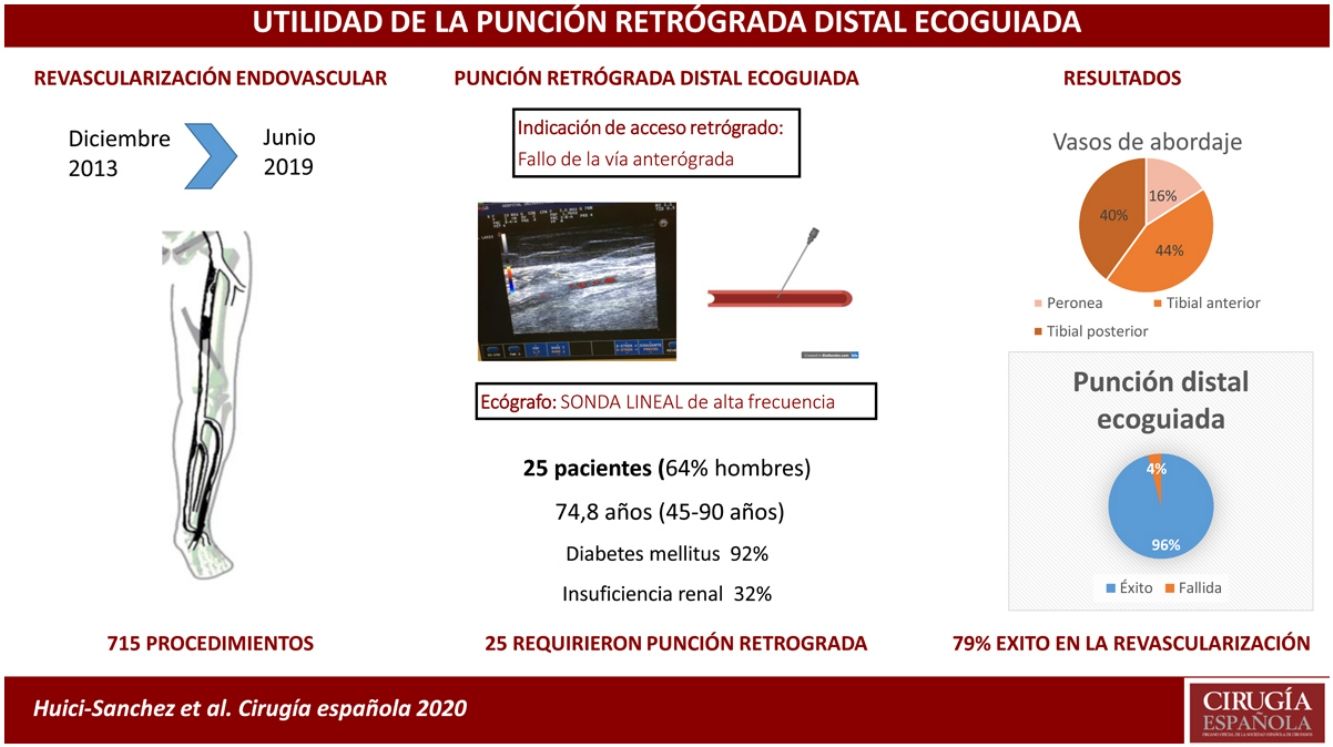
Retrograde access performed guided by fluoroscopy or ultrasound. We aimed to analyze the usefulness of ultrasound in retrograde access in patients with critical limb ischemia.
MethodsObservational analytical study. From December 2013 to June 2019. We included all retrograde accesses that were guided by ultrasound. Our register assesses demographic and clinical data, the vessel used as retrograde access, the procedure performed, the amount of contrast agent used and time of fluoroscopy, access failure, and local complications.
ResultsOn 715 procedures performed, was used ultrasound-guided retrograde access in 25 patients (64% men). The mean age was 74.8 years (45–90), with 92% of diabetics and 32% of chronic renal failure. Two patients with Rutherford stage 4 and 23 with stage 5–6. In 24 (96%) patients the ultrasound-guided puncture was successful, while in one (4%) of them, it was not possible to enter the target vessel. After the punch, was achieved the technical success of revascularization in 19 (79.2%) patients, with 5 (20.8%) in whom did not the arterial injury was not overcome. The arteries used as retrograde access were: anterior tibial 11, posterior tibial 10, and peroneal in 4. The mean of contrast used was 63 mL (9–100 mL) with an average time of 43 min (15–76 min). Complications related did not observe in retrograde access.
ConclusionsUltrasound-guided retrograde distal access is an effective method that may use as a bailout method in those endovascular procedures in which it is not possible to cross the lesion anterogradely.
La punción retrógrada se puede realizar guiada mediante fluoroscopia o ecografía. Nuestro objetivo fue analizar la utilidad de la ecografía en la punción retrógrada distal de las extremidades inferiores.
MétodosEstudio analítico observacional de diciembre 2013 a junio 2019. Se incluyeron todos los accesos retrógrados distales que fueron realizados guiados ecográficamente. Se analizaron datos demográficos y clínicos, vaso utilizado como acceso retrógrado, procedimiento realizado, cantidad de contraste usada y tiempo de escopia, fallo en el acceso, y complicaciones locales.
ResultadosDe 715 procedimientos, se utilizó el acceso retrógrado ecoguiado en 25 pacientes (64% hombres). La edad media fue de 74,8años (45–90), con un 92% de diabéticos y un 32% de insuficiencia renal crónica. La clínica inicial era estadio 4 de Rutherford en 2 pacientes, y estadios 5-6 en los restantes 23 pacientes. En 24 (96%) pacientes la punción ecoguiada fue satisfactoria, mientras que en un caso (4%) no se consiguió entrar en el vaso diana. Posteriormente a la punción, el éxito técnico de la revascularización fue conseguido en 19 (79,2%) pacientes, con 5(20,8%) en los que no se consiguió superar la lesión. Las arterias utilizadas como acceso retrógrado fueron: tibial anterior 11, tibial posterior 10 y peronea en 4. Se utilizó una media de 63 mL (9–100 mL) de contraste con un tiempo medio de escopia de 43 minutos (15–76 min). No se observaron complicaciones relacionadas con el acceso retrógrado.
ConclusiónesEl acceso retrógrado distal ecoguiado es un método seguro y efectivo, que supone un buen recurso en aquellos procedimientos endovasculares en los que no es posible su realización vía anterógrada.
Critical lower limb ischaemia is a growing health problem causing high morbidity and mortality in the population1. Endovascular treatment for revascularisation is currently the first choice in most patients2. It is traditionally performed by proximal access to the lesion and its antegrade catheterisation, usually through a puncture of the common femoral artery, however, in 20%–40% of patients with chronic occlusive lesions it is not possible to cross the lesion by this route3. To overcome this problem, we use various recanalisation or re-entry devices, and retrograde access, i.e., puncturing the artery distal to the lesion and recanalising the lesion in the reverse direction of flow. Retrograde puncture of the arteries at the level of the ankle was first described by Iyer et al. in 19904, and since then several published case series have shown it to be an effective alternative. Retrograde puncture can be performed under fluoroscopic or ultrasound guidance. The benefits of ultrasound are the absence of irradiation and the possibility of assessing the calibre and less calcified areas of the vessel to be punctured.
The aim of this study is to analyse the usefulness of ultrasound-guided puncture in the distal retrograde approach used for chronic ischaemia of the lower extremities.
MethodStudy design: Retrospective analytical observational study in the vascular surgery department of a tertiary hospital, a referral centre for an area of 1,300,000 inhabitants.
Inclusion criteria: All patients were included who underwent revascularisation surgery using the endovascular technique of the lower limbs with criteria of critical ischaemia and requiring distal retrograde access performed by ultrasound.
Indication for retrograde access: Failed revascularisation from the antegrade route via the femoral artery.
Exclusion criteria: Patients in whom data could not be collected from computer records due to loss to follow-up.
Data collection: Demographic data were compiled prospectively in a database. Demographic information, vascular risk factors and pathological history of interest were collected. The distal artery used as retrograde access, the amount of contrast used, and the time of fluoroscopy were recorded. Echo-Doppler velocities were performed at follow-up to assess the patency of the procedure.
Primary variables analysed: Technical success, local complications related to the puncture and patency at one, six and 12 months.
Secondary variables analysed: Types of endovascular procedures performed (simple angioplasty [PTA], medical PTA or stenting). The clinical progression, limb salvage rate and mortality of the sample were assessed.
Definitions- •
Critical ischaemia: Patient with lower limb peripheral artery disease associated with pain at rest and/or trophic lesions (Rutherford categories 4, 5 and 6).
- •
Percutaneous vascular access: Accessing the arterial lumen by needle puncture followed by placement of a guidewire inside the needle, after which the needle is removed, and the guidewire remains as a guide (Seldinger technique).
- •
PTA: Dilatation of the target artery using a balloon.
- •
Technical success in our series: Defined as any puncture that ends with the introducer inside the true lumen of the distal vessel.
- •
Revascularisation success: Being able to cross the lesion via retrograde access and achieve revascularisation.
- •
Ultra-low-profile balloon: A balloon with an inflation diameter of 1.5–3 mm, useful for small calibre vessels such as the tibial and fibular arteries.
Statistical analysis: The extracted data were stored and processed in a Microsoft Access® relational database. The quantitative and categorical variables were tabulated. SPSS v.19.0 for Windows® was used to evaluate the data.
Ethics committee: Study approved by our centre’s research ethics committee with reference number: PR458/20.
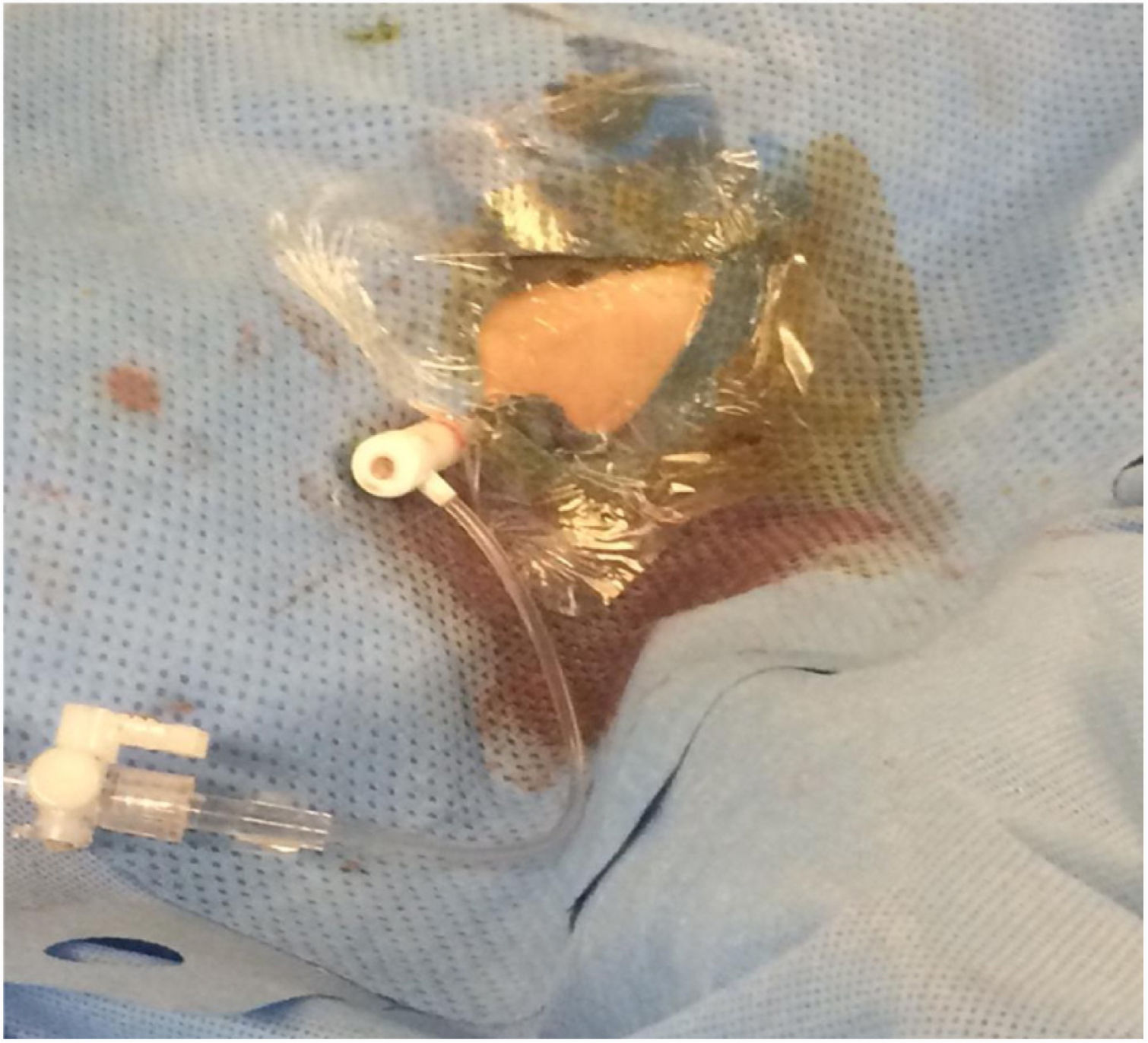
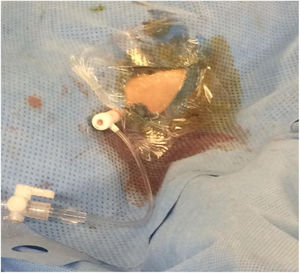
Retrograde puncture techniqueAll the patients underwent sciatic-popliteal neurological block of the affected leg by anaesthesia with Ropivacaine .5%, 10 mL. A medium-high frequency linear probe of a portable ultrasound machine (ESAOTE mylab25, ESAOTE SPA) with LA523 probe was used (Figs. 1 and 2); analysing the morphology and condition of the distal vessel wall that was considered the most suitable for the retrograde approach. Patency of the vessel was corroborated and the area with the least calcification was located for puncture.
Vascular access was achieved using a 4 F micropuncture kit (Cook Medical, Bloomington, Ind). This kit contains a 4 cm 21 G echogenic needle, a .018″ guidewire, a 2.9 Fr, 7 cm microintroducer and a haemostatic valve. Once the micro-introducer was in place (Fig. 3), a .018-inch guidewire was introduced through the retrograde access and advanced proximally with the aid of a support catheter (Cook Medical CXI®). Once past the lesion, the distal guidewire was “captured” until it was exited through the proximal introducer. Thus, maximum, and secure support was achieved in the true arterial lumen. The PTA and/or stenting procedure was performed via the antegrade route in all cases.
Haemostasis technique for retrograde accessOn completion of the intervention, haemostasis was usually performed by manual compression. Another technique was to inflate a low-profile balloon catheter at low pressures at the puncture site for three to five minutes. For this, once the distal introducer and the other distal devices were removed, the guidewire was passed distal to the puncture site and a balloon with a diameter equivalent to the lumen of the punctured vessel was inflated. If balloon haemostasis was not effective, manual compression of the puncture site was applied for 10 min and non-circumferential compression was applied for 12 h. Balloon haemostasis allowed us to keep the lumen of the punctured distal vessel patent.
ResultsOf 715 endovascular procedures performed from December 2013 to June 2019, distal echogenic retrograde access was used in 25 patients (3.49%). Their mean age was 74.8 years (45–90). Table 1 summarises the demographic and clinical characteristics of our population.
Demographic and clinical data.
| n = 25 | |
|---|---|
| Sex | |
| Male | 16 (64%) |
| Female | 9 (36%) |
| Risk factors | |
| Arterial hypertension | 23 (92%) |
| Diabetes mellitus | 23 (92%) |
| Dyslipidaemia | 20 (80%) |
| Renal failure | 8 (32%) |
| Ischaemic heart disease | 8 (32%) |
| COPD | 8 (32%) |
| Clinical category | |
| Rutherford 4 | 2 (8%) |
| Rutherford 5 | 20 (80%) |
| Rutherford 6 | 3 (12%) |
COPD: chronic obstructive pulmonary disease.
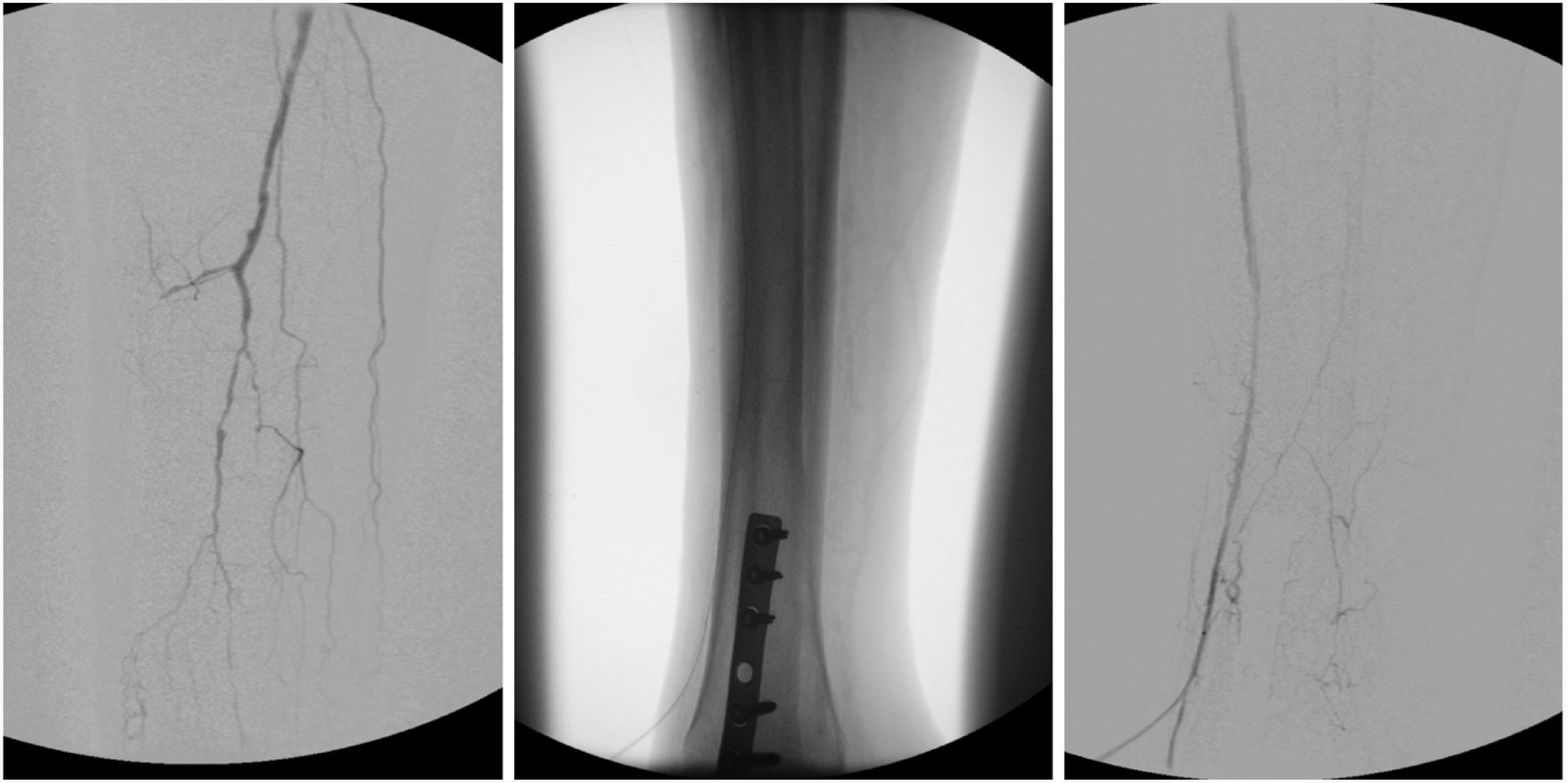
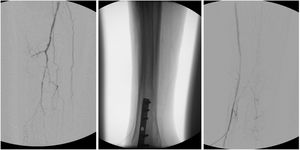
The arteries used as retrograde access were anterior tibial in 11 cases (44%), posterior tibial in 10 (40%), and fibular in four (16%) (Fig. 4).
A mean of 63 mL (9–100) of contrast was used, with a mean fluoroscopy time of 43 min (15–76).
The technical success rate of ultrasound-guided puncture was 96%; one procedure failed to correctly puncture the target vessel. Of the 24 cases in which correct puncture was achieved, a total of 19 (79.2%) were successful using the revascularisation technique, with five (20.8%) accesses in which it was not possible to cross the lesion. No access-related complications were observed.
Table 2 details the endovascular procedures performed, and the sector treated.
The mean duration of follow-up was 18 ± 17.9 months. The patency of the procedures at 1, 6 and 12 months was 100%, 78.5%, and 71.4%, respectively. Clinical improvement was observed in 64% of the patients at one year. None of the limb-spared subjects at follow-up required distal bypass surgery.
The limb salvage rate was 88% and 80% at six and 12 months, respectively. In all cases, the cause of limb loss was superinfection of trophic lesions.
Mortality in the series was 12% (three patients), with the cause of death unrelated to critical ischaemia or the retrograde puncture. One individual died of gastrointestinal haemorrhage at 30 days, another due to pneumonia at three months, and the third of sepsis secondary to urinary tract failure (UTI) at six months after the procedure. In none of the cases was a post-mortem study performed.
DiscussionUltrasound-guided retrograde puncture is a technique with a high technical success rate, avoiding irradiation of the surgeon and the patient during the procedure and achieving a high limb salvage rate in complex arterial lesions. It is a good tool in individuals in whom it has not been possible to cross the lesion by the antegrade route; in line with other published series3,5.
The increasing complexity of arterial lesions increases the rates of failure to cross the lesions, which has resulted in the development of alternatives to treat chronic lower limb ischaemia, such as re-entry devices or retrograde puncture5,6. One of the benefits of retrograde punctures is that it is easier to cross the target lesion according to the type of lesion presented by the patient. Therefore, the chronic total occlusion crossing approach based on plaque morphology (CTOP) classification was created by Saab et al. according to which type I lesions would be easily crossed using the antegrade approach, while types II–IV would benefit from the addition of a retrograde approach7. In our series this classification was not analysed as the decision for retrograde puncture was not based on the morphology of the occlusion but on intraoperative clinical need. Another benefit of this technique could be a lower cost compared to recanalisation or re-entry devices. Two re-entry devices were compared; each Outback LTD device costs approximately euro1,500 and each Pioneer catheter euro2,600, the latter also requires an intravascular ultrasound (IVUS) machine8. In the retrograde approach, the additional cost is only that of the microintroducer, and some groups even report using this technique without a microintroducer, using only the support catheter9. Our group advocates the use of the micro-introducer because it is possible to use ultra-low profile balloons if necessary. However, a cost-effectiveness study is appropriate for comparison with other devices.
In our series, the success rate of distal ultrasound-guided puncture, and thus access to the vessel useful to undertake the procedure, was 96%. The 2016 prospective multicentre study by Walker reports an access failure rate of 6.6%, but does not specify success in ultrasound-guided puncture9. Once distal access was achieved, most of our technical failures were associated with an inability to re-enter the true lumen, in most cases due to vessel calcification. The technical success rate of retrograde interventions in our sample (79%) is similar to the range reported in the literature, between 67% and 100%, where technical success rate was defined as the ability to cross the lesion retrogradely and complete the revascularisation procedure10. This great variability in technical success rates could be because there is no standardised protocol for retrograde interventions and because it is a technique that requires a learning curve due to its technical complexity. Shishehbor and Chenier11 propose an algorithm with a time limit (10 min) to cross the lesion, and if not possible, they opt for retrograde access. In the literature, this technique has been used mainly after failed antegrade access and no specific comparison has been made between ultrasound-guided or fluoroscopic puncture5,12, therefore, to date, and to our knowledge, this is the first study to report data specific to the ultrasound-guided technique.
Complication rates for the retrograde approach range from 1.0% to 12.5%, most of which are minor and do not require intervention13. In our series, there are no puncture-related complications, possibly due to the use of echo-Doppler, which makes it possible to decide which segment of the distal vessel is most suitable for puncture compared to fluoroscopic techniques that do not allow a thorough assessment of the puncture site. The safety profile of this procedure has prompted several authors to use distal retrograde access as a primary procedure in patients with morbid obesity or other contraindications or difficulties for antegrade access14. However, in our experience, this is not a common practice, as antegrade access is achieved in most patients. Occlusion of the retrograde access vessel is one of the major complications to consider and prevent, especially if it is the only outflow trunk. Techniques have been suggested to reduce this risk, such as the use of intra-arterial vasodilators to minimise vasospasm, and access without introducer placement or open vessel dissection with direct vessel puncture. In our opinion, the correct assessment of the vessel at the puncture site is essential to avoid injury to the vessel15. As the vessels are small in diameter, ultrasound monitoring allows visualisation when intraluminal, and finding the least damaged area, which is not possible with fluoroscopy. It is important to note that the success of the procedure is not only down to the puncture, the anaesthetist must also be involved, since the sciatic nerve block, which is performed in all cases, not only ensures patient comfort but also favours distal vasodilatation, avoiding vasospasm related to the puncture and placement of the microintroducer.
ConclusionWe conclude that ultrasound-guided distal retrograde access is an effective and safe method that achieves a high percentage of limb salvage in endovascular procedures that cannot be performed via the antegrade route. The use of ultrasound for puncture and agreeing a time limit for complex lesions would help to reduce contrast exposure to the patient and radiation exposure to the surgeon and the patient.
The limitations of our study are that it is a retrospective study of prospectively collected data, with the risk of bias associated with a non-randomised study, and the low number of cases collected, which reduces its external validity.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Huici-Sanchez M, Martí-Mestre FJ, Martinez-Rico C, Espinar-Garcia E, Jiménez-Guiu X, Romera-Villegas A, et al. Utilidad de la ecografía en la punción retrógrada distal en la isquemia crítica de extremidades inferiores. Cir Esp. 2022;100:431–436.