Subjects with prediabetes, defined as impaired fasting blood glucose (IFG), have an increased cardiovascular risk. The main objective of the study is to establish whether prediabetes is associated with the presence of subclinical atherosclerotic plaque (pATS) regardless of age, sex, arterial hypertension and other cardiovascular risk factores.
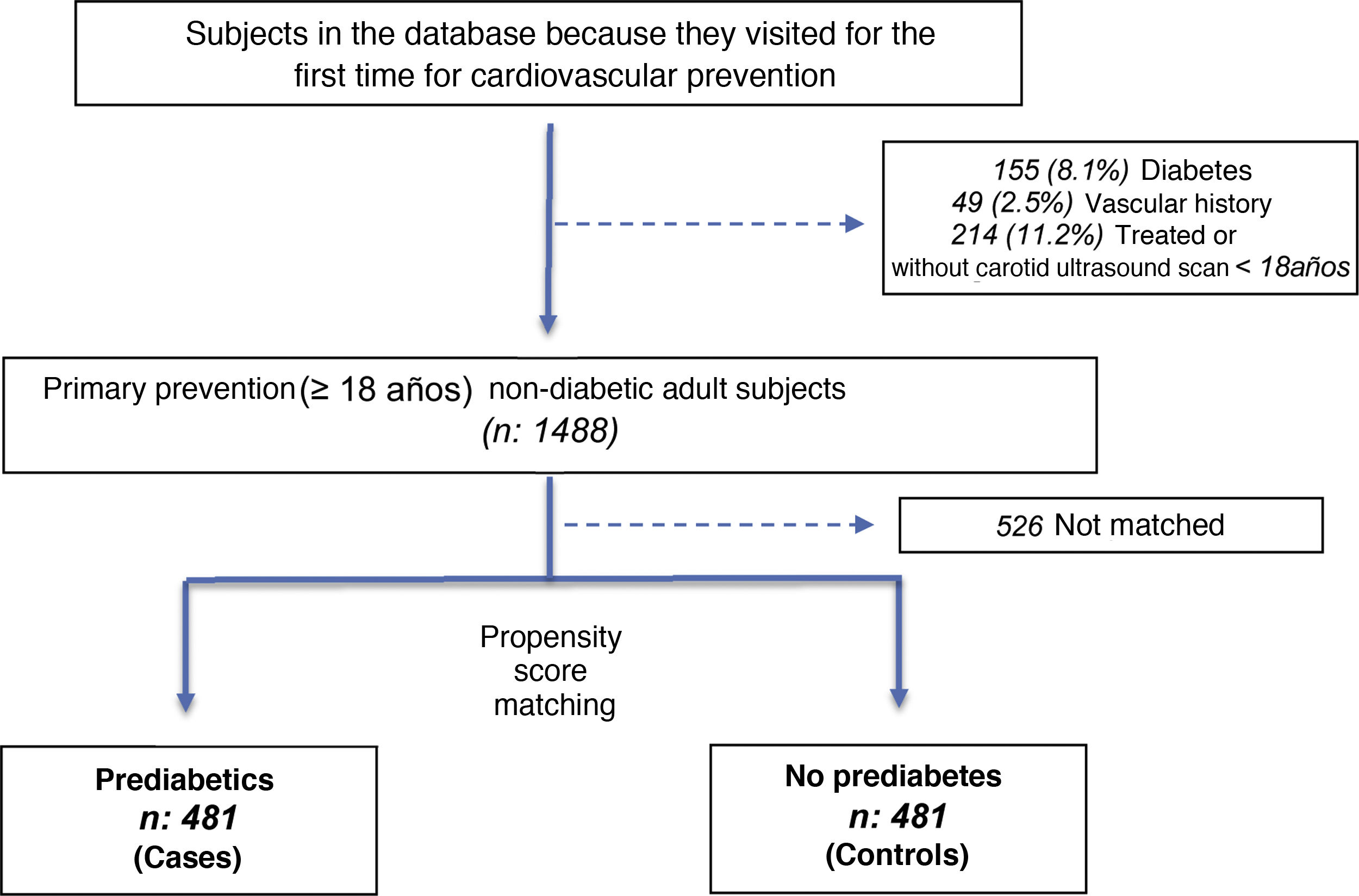
Material and methodsObservational study with propensity score matching (PSM). We included 481 subjects with prediabetes (according to the criteria of the American Diabetes Association) and 481 controls matched for age, sex, and hypertension. Subjects with coronary artery disease and/or peripheral vascular disease and/or diabetes were excluded. pATS was defined as the presence of plaque detected by carotid doppler ultrasound.
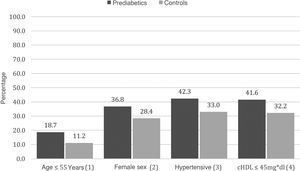
ResultsThe prevalence of pATS was 34.7% in prediabetic subjects compared to 28.8% in controls. The adjusted odds ratio (OR) after controlling for age, sex, hypertension, and HDL-C was 1.29 (95% CI: 1.12–1.48; P < .001). The prevalence of pATS was 42.3% in hypertensive prediabetic subjects compared to 32.9% in controls (OR: 1.49; CI: 1.05–2.12; P: .02). We also observed higher pATS (18.7%) in younger subjects (≤55 years) compared to controls (11.1%) of the same age (OR: 1.83; CI: 1.05–3.2; P: .03).
ConclusionSubjects with prediabetes were associated with a higher prevalence of pATS. The possibility (“Odds”) of presenting subclinical atherosclerosis was 29% higher in subjects with prediabetes after adjusting for age, sex, hypertension and HDL-C.
Los sujetos con prediabetes, definida como glucemia alterada en ayunas (IFG), tienen un riesgo cardiovascular aumentado. El objetivo principal del estudio es establecer si la prediabetes se asocia con la presencia de placa ateroesclerótica subclínica (pATS) en forma independiente de la edad, sexo, hipertensión arterial y otros factores de riesgo cardiovascular.
Materiales y métodosEstudio observacional apareado por puntaje de propensión (PSM). Se incluyeron 481 sujetos con prediabetes (según los criterios de la Asociación Americana de Diabetes-ADA) y 481 controles apareados por edad, sexo e hipertensión arterial. Se excluyeron sujetos con enfermedad coronaria y/o vascular periférica y/o diabetes. La pATS fue definida como la presencia de placa detectada por ecografía doppler carotidea.
ResultadosLa prevalencia de pATS fue de 34.7% en los sujetos prediabéticos comparado con 28.8% en los controles. El “odds ratio” (OR) ajustado tras realizar el control por edad, sexo, hipertensión arterial y cHDL fue de 1.29 (IC95%: 1.12–1.48; P < .001). La prevalencia de pATS fue de 42.3% en los sujetos prediabéticos hipertensos comparada con 32.9% en los controles (OR: 1.49; IC: 1.05–2.12; P: .02). También observamos mayor pATS (18.7%) en los sujetos más jóvenes (≤55 años) comparada con los controles (11.1%) de igual edad (OR: 1.83; IC: 1.05–3.2; P: .03).
ConclusionesLos sujetos con prediabetes se asociaron con mayor prevalencia de pATS. La posibilidad (“Odds”) de presentar ateroesclerosis subclínica fue 29% mayor en los sujetos con prediabetes tras ajustar por edad, sexo, hipertensión arterial y cHDL.
The prevalence of diabetes in individuals over the age of 20 years in Latin America amounts to 8%–10%, and it is increasing.1 This growth may have been favoured by diet, obesity and the sedentary lifestyle observed in our region.1
The majority of patients with diabetes go through an asymptomatic prediabetes period which is characterized by impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT).2 Furthermore, prediabetes will progress into symptomatic type 2 diabetes mellitus (DM2) in approximately 25% of subjects within 3–5 years.3
Diabetes and prediabetes have an increasing economic impact on health systems, so that it is of key importance of prepare strategies to improve the detection, prevention and treatment of the disease and its complications.4
The worldwide prevalence of prediabetes varies according to the definition and value of the cut-off point selected for IFG or glucose intolerance.3,5 The lower limit set by the American Diabetes Association (ADA) and recommended by the European Society of Cardiology (ESC) guides and the European Association for the Study of Diabetes (EASD), leads to far higher rates of prevalence than those defined by WHO guides.2,3 In a cohort of non-diabetic adults without a history of myocardial infarct, changing the lower threshold of the IFG from 110 to 100 mg/dl led to an increase in the prevalence of prediabetes from 19.8% up to 34.6%.6 In this study, 34.6% had prediabetes and 19.4% only had IFG; 5.4% only had IGT and 9.8% had IFG or IGT.6
During the prediabetes period a series of changes occur which favour the development of atherosclerosis, including lipid profile alterations, endothelial dysfunction and inflammatory changes which favour the early development of atherosclerosis.7 Multiple studies of patients with prediabetes, defined as IFG, show that the risk of cardiovascular events, coronary disease, cerebrovascular accident and/or cardiovascular and total mortality increases.8
The association between carotid artery intima media thickness and HbA1c in individuals without diabetes has been widely studied. In the MESA study which included 5121 participants, this association was proven to exist after adjusting for cardiovascular risk factors.9 Nevertheless, few clinical studies have analysed the association between prediabetes and the presence of atherosclerotic plaque, possibly because of the difficulty which arises due to the presence of multiple confusion factors in this population. Nor is it clear whether subgroups of patients with prediabetes and a higher prevalence of atherosclerosis exist, as a result of which they would benefit more from early intervention.
The core aim of this study is to establish whether prediabetes is associated with the presence of subclinical atherosclerotic plaque (SATp) independently of age, sex, arterial hypertension (AHT) and other potential cardiovascular risk factors which may function as confusion factors.
MethodsStudy design and populationThis study has a cross-sectional observational design with propensity score matching (PSM). The inclusion criteria were: 1) adults ≥18 years; 2) prediabetes (according to ADA criteria), defined as IFG with glycaemia values from 100 to 125 mg/dl and HbA1c < 6.5%; 3) no lipid-lowering or antidiabetic treatment in the previous 6 months and 4) first time visit to the cardiovascular prevention department of our hospitals. Subjects with coronary and/or peripheral vascular disease and/or diabetes (defined as a history of treated diabetes or glycaemia ≥126 mg/dl or HbA1c ≥ 6.5%). The data source was a prospective consecutive registry of the cardiovascular prevention department in our hospital. A control group of individuals without prediabetes was selected from the same database using PSM, with identical inclusion - exclusion criteria and similar age, sex, and AHT. Initial matching took place based on age, sex and AHT, as these are confusion factors that predict atherosclerotic plaque in our primary prevention population. Other confusion factors were selected in 2 stages later from the classic risk factors by logistic regression analysis, followed by analysis of subgroups (see statistical analysis).
VariablesThe demographic data, variables of interest and cardiovascular risk factors were taken from the prospective and consecutive registry of the cardiovascular prevention department of our hospital and the clinical histories of the subjects.
The following definitions of cardiovascular risk factors were used: AHT when arterial pressure was ≥140/90 mmHg or if the patient was receiving treatment or had a history of AHT. Smoking was restricted to a history of smoking in the past year, and ex-smoking was not considered due to the lack of a historical record of this variable. The continuous variables were categorized for analysis of subgroups and the calculation of the adjusted odds ratio (OR). The following categories were included: age (≤55 and >55 years); cholesterol associated with LDL (c-LDL < 160 and ≥160 mg/dl); cholesterol associated with HDL (HDL-c ≤ 45 and >45 mg/dl) and triglycerides (TG ≤ 150 and >150 mg/dl). These categories were selected on the basis of traditional cut-off points (for c-LDL and TG) and on previous data in our population on the optimum cut-off point (age and HDL-c).
Subclinical atherosclerosis was defined as the presence of one of more atherosclerotic plaques detected by carotid ultrasound-Doppler scan (SATp) using the criteria of the ARIC10 study, which takes into account 2 of the following 3 criteria: a) Increase of the thickness of the intima-media >1.5; b) Abnormal shape (protrusion into the open span, loss of wall alignment), and c) abnormal texture. Laboratory biochemical analysis and ultrasound carotid vascular assessment were undertaken in the central laboratory and the cardiovascular ultrasound scan department of our institution.
The prevalence of SATp was also studied according to the following subgroups: age, sex, AHT, current smoking, family history of early coronary disease, c-LDL, HDL-c and TG.
Insulin resistance was evaluated using the glucose insulin index (HOMA-IR). A consecutive subgroup of cases and controls were subjected to ultrasensitive reactive protein C determination (usRPC). This determination was not carried out in all of the patients as it ceased to be performed during the last 18 months of the registration due to administrative reasons.
Ethical aspectsThe protocol of this study was approved beforehand by the Ethics Committee of our institution, and it is registered in the PRIISA.BA clinical studies database (number 4852) of the government of the city of Buenos Aires. The study was undertaken respecting the local regulations for observational studies (resolution 1480/2011 of the National Ministry of Health) and according to good pharmacological-epidemiological good practice. As it is a retrospective study and the data source is secondary no written informed consent was required, according to the exceptions listed in the local regulations for observational studies.
Statistical analysisThe size of the sample was calculated based on an estimate of the prevalence in our population of SATp of 40% in prediabetic subjects, and of 30% in the control group. Estimations are based on the prevalence of SATp in high-risk subjects in our primary prevention populations and the findings of studies similar to ours.11–13 A sample of 354 subjects per group (708 in total) would give as 80% power to detect an absolute difference of 10% in the prevalence of SATp according to Doppler ultrasound carotid scan, with a confidence interval of 95% (CI 95%). The control group was selected by PSM using the best neighbour method with 1:1 matching. The additional material contains a description of how the matching was performed. CI at 95% were calculated using the exact method. Inferential statistics were used for the basal and subgroups analyses, applying the Student’s t-test or the Mann-Whitney U test and the Chi-squared test or Fisher’s exact test for continuous or categorical variables, respectively, as appropriate.
The final adjustment model includes the 3 confusion variables defined in the protocol for matching (age, sex and AHT) due to their relevance as predictors of SATp in our population. Other confusion factors are also included after they had been selected from the classical risk factors in two stages. They were first selected using logistic regression in the total population, and then by association analysis of SATp in prediabetic individuals versus controls within the different subgroups of confusion factors selected by logistic regression. A cut-off point of P < .1 was used to select additional confusion factors in logistic regression as well as in the subsequent analysis of subgroups. The adjusted OR of the association between prediabetes and SATp was calculated using the Cochran-Mantel-Haenszel method, controlled by the strata used in matching and additional confusion factors. The adjusted OR was analysed after checking the homogeneity of the strata using Woolf’s test. Version 3.5.0. of the CRAN® statistical programme was used, and the level of significance was set at 5%.
ResultsOf the total number of 1488 subjects, 481 (32.3%) cases with prediabetes were included, as were 481 controls without prediabetes. They were matched for age, sex and the presence of AHT, and then included in the database during a 36-month period that ended in January 2018. The reason they visited was a routine cardiovascular check-up (Fig. 1).
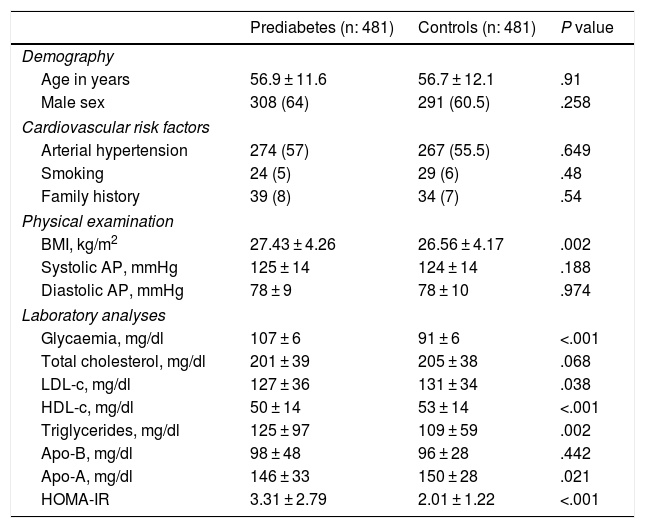
Characteristics of the populationBefore matching the prediabetic patients were characterised by being at higher cardiovascular risk, as they tended to be older, male, with AHT and low HDL-c, high TG and a high prevalence of SATp in comparison with the patients without prediabetes (Appendix B, Table S1 in the additional material). After matching, the cases and controls had similar characteristics in terms of age, sex and the prevalence of AHT, and the patients with prediabetes had a higher body mass index, greater insulin resistance and higher levels of TG, together with lower levels of HDL-c and c-LDL in comparison with the controls (Table 1).
Characteristics of the subjects.
| Prediabetes (n: 481) | Controls (n: 481) | P value | |
|---|---|---|---|
| Demography | |||
| Age in years | 56.9 ± 11.6 | 56.7 ± 12.1 | .91 |
| Male sex | 308 (64) | 291 (60.5) | .258 |
| Cardiovascular risk factors | |||
| Arterial hypertension | 274 (57) | 267 (55.5) | .649 |
| Smoking | 24 (5) | 29 (6) | .48 |
| Family history | 39 (8) | 34 (7) | .54 |
| Physical examination | |||
| BMI, kg/m2 | 27.43 ± 4.26 | 26.56 ± 4.17 | .002 |
| Systolic AP, mmHg | 125 ± 14 | 124 ± 14 | .188 |
| Diastolic AP, mmHg | 78 ± 9 | 78 ± 10 | .974 |
| Laboratory analyses | |||
| Glycaemia, mg/dl | 107 ± 6 | 91 ± 6 | <.001 |
| Total cholesterol, mg/dl | 201 ± 39 | 205 ± 38 | .068 |
| LDL-c, mg/dl | 127 ± 36 | 131 ± 34 | .038 |
| HDL-c, mg/dl | 50 ± 14 | 53 ± 14 | <.001 |
| Triglycerides, mg/dl | 125 ± 97 | 109 ± 59 | .002 |
| Apo-B, mg/dl | 98 ± 48 | 96 ± 28 | .442 |
| Apo-A, mg/dl | 146 ± 33 | 150 ± 28 | .021 |
| HOMA-IR | 3.31 ± 2.79 | 2.01 ± 1.22 | <.001 |
Continuous variables are expressed as an average ± standard deviation; categorical variables are expressed as n (%).
Apo-A: apolipoprotein A; Apo-B: apolipoprotein B; HDL-c: cholesterol bound to HDL; LDL-c: cholesterol bound to LDL; HOMA-IR: insulin resistance score; BMI: body mass index; AP: arterial pressure.
The usRPC was measured in 228 cases and 243 controls. It was higher in the group of patients with prediabetes (average ± SD: 3.37 ± 12.66 mg/dl; median and quartile -Q1/Q3: 1.55 and 0.8/3.37 mg/dl) compared with the control group (average ± SD: 2.04 ± 2.93 mg/dl; median and Q1/Q3: 1.2 and 0.6/2.45 mg/dl); P: .026.
Analysis of the confusion factors associated with atherosclerotic plaqueThe additional confusion factors associated with atherosclerotic plaque were selected from among the classic risk factors, and they were studied in 2 steps for subsequent inclusion in the final model for analysis. Logistical regression analysis was applied in the first step to the total population (cases and controls) to study the potential association between different risk factors and atherosclerotic plaque in the study population. The 2 additional risk factors selected after logistic regression were current smoking and HDL-c (≤45 and >45 mg/dl) (Appendix B, Table S2 in the additional material). The second step consisted of analysis of the subgroups of the prediabetic patients versus the controls, studying the association between the risk factors used in matching (age, sex and AHT) and the risk factors selected in the logistic regression (current smoking and HDL-c), with atherosclerotic plaque (Appendix B, Table S3 and Fig. S2 in the additional material).
After these analyses HDL-c (≤45 and >45 mg/dl) was selected as an additional confusion factor together with the variables used in matching (age, sex and AHT) associated with the presence of plaque and prediabetes for inclusion in the final model. All of these variables were associated with a higher prevalence of plaque in prediabetic patients in comparison with the controls, with a value of P < .1, so that they were selected for the final model (Appendix B, Table S3 and Fig. S2 in the additional material).
Prevalence of atherosclerotic plaqueThe prevalence of SATp amounted to 34.7% (167/481) in the prediabetic patients, compared to 28.8% (139/481) in the controls. The adjusted OR (Cochran-Mantel-Haenzel) after checking for age, sex, AHT and HDL-c was 1.29 (CI 95%: 1.12–1.48; P < .001) (Fig. 2).
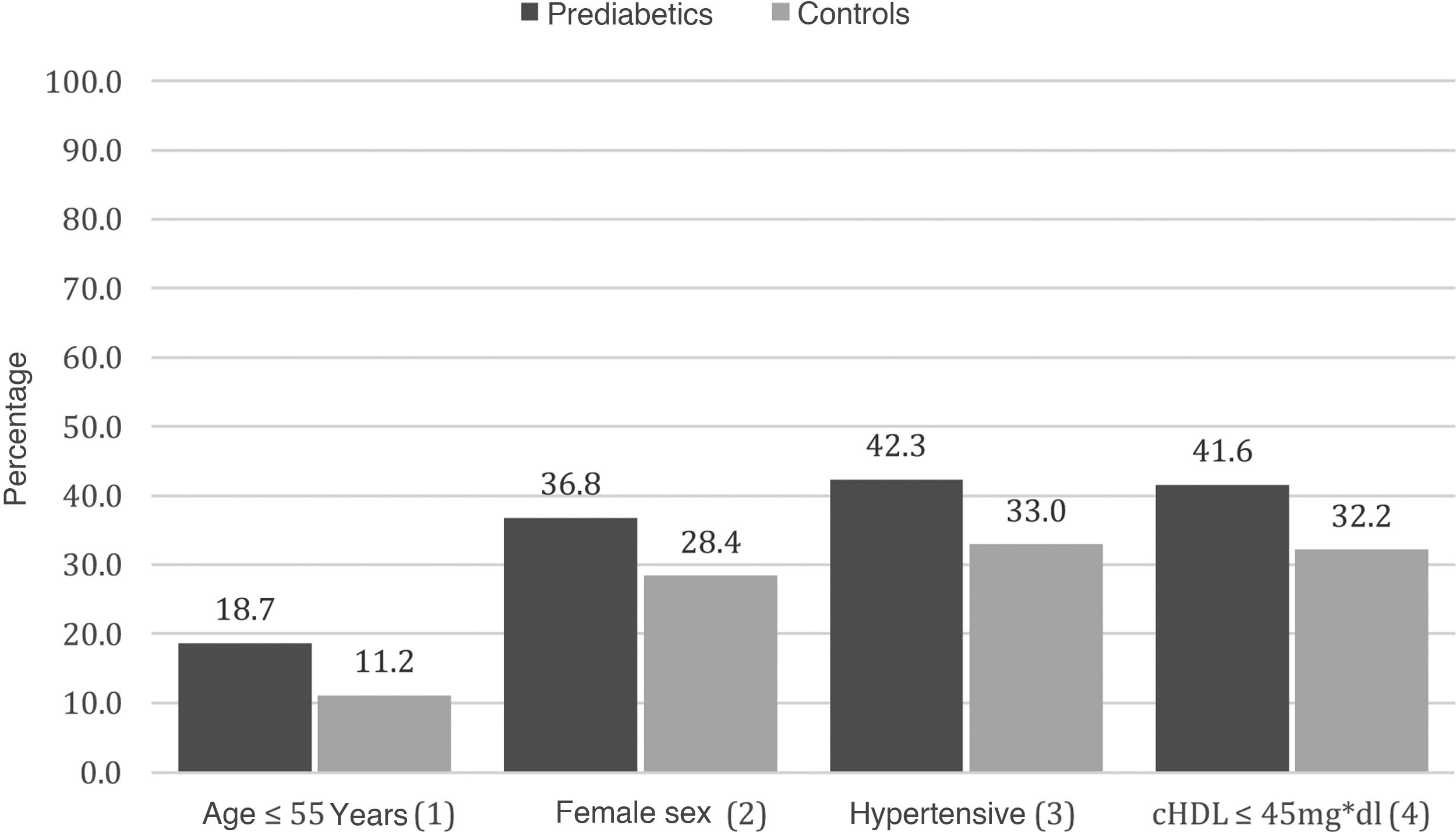
In the analysis of subgroups, a higher prevalence of SATp was found in the subgroups with younger prediabetic subjects (≤55 years) and in the hypertensive subjects, in comparison with the controls (Appendix B, Table S3 and Figs. 2 and S2 in the additional material). The prevalence of SATp was 18.7% in the younger prediabetic patients, compared with 11.1% in the controls with a similar age (OR: 1.83; CI 95%: 1.05–3.2; P: .03). The prevalence of SATp was 42.3% in the prediabetic patients with hypertension, compared to 32.9% in the hypertensive controls (OR: 1.49; CI 95%: 1.05–2.12; P: .02) (Appendix B, Table S3 and Figs. 2 and S2 in the additional material).
SATp tended to be higher in the prediabetic patients with HDL-c ≤ 45 mg/dl, in comparison with the controls with similar levels of HDL-c, 41.9 and 32.2%, respectively (OR: 1.52; CI 95%: 0.98–2.36; P: .06). Furthermore, a tendency was observed for SATp to be higher in female prediabetic patients compared to the controls, at 18.7 and 11.2%, respectively (OR: 1.48; CI 95%: 0.95–2.3; P: .08) (Appendix B, Table S3 and Figs. 2 and S2 in the additional material).
DiscussionThis study confirmed the higher prevalence of SATp in subjects defined as prediabetic compared with the control group, after adjusting for potential cardiovascular risk factors (age, sex, AHT and HDL-c).
The adjusted OR of 1.29 (CI 95%: 1.12–1.48) is consistent with the ILERVAS and SPREDIA-2 studies.12,13 The ILERVAS study included 2269 patients who were prediabetic according to ADA criteria, with basal characteristics that were very similar to those of our population, and 4419 controls in 30 primary care centres in Spain.12 This study found a higher prevalence of SATp in prediabetic patients (49.3%) in comparison with the control group (43.5%). This higher prevalence was due to the carotid territory (OR: 1.27; CI 95%: 1.14–1.40; P < .001).12 The association of HbA1c levels with SATp remained significant even after adjustment for age, sex and cardiovascular risk factors.12 SPREDIA-2 is a population-based epidemiological study undertaken in Spain that selected a random sample in the population of 1457 adults, of whom 850 had prediabetes and 349 were controls.13 The SPREDIA-2 study found a higher prevalence of SATp in prediabetic patients (45.1%) compared to the control group (34.2%). After adjusting for age, sex and cardiovascular risk factors the OR was 1.31 (CI 95%: 1.01–1.69).13
Our study complements the observations of ILERVAS and SPREDIA-2, as although its findings were similar, they arose in a lower-risk Argentine population and it had an observational design with PSM and a final estimation of the OR adjusted according to cardiovascular risk factors. We believe that, although it is a cross-sectional study, its design characteristics (propensity score matching) improve its internal validity and level of evidence.
Analysis of the subgroups showed a higher prevalence of SATp in the hypertensive participants and the younger ones. The association of SATp with classic risk factors such as hypertension and high glycaemia levels has been described well in patients with metabolic syndrome.14 The increased effect of prediabetes on the coronary calcification score in the younger population was observed beforehand in age-stratified studies.15 The INTERHEART study found that higher levels of HbA1c were associated with a 19% higher probability (CI 95%: 14–23) of acute myocardial infarct after adjusting for all of the risk covariables.16 This association was the strongest in the youngest patients.16 These findings may indicate that atherosclerotic processes are possibly more likely to be detected at an early age due to the lower prevalence of other confusion factors in a younger population.17 A tendency that was not significant was also observed in our study for plaque to be more present in women and subjects with low HDL-c. In previous studies prediabetic women have been associated with a higher coronary calcification score8 and increased cardiovascular risk.18,19
The subjects with prediabetes in our study were associated with a higher insulin resistance score and inflammatory activity. Insulin resistance is associated with atherogenic dyslipidaemia (low levels of HDL-c, a predominance of small dense LDL-c particles and high TG), endothelial dysfunction, inflammation and alteration of fibrinolysis, all of which are factors associated with higher risk of cardiovascular disease.20–23 This may imply that glycide metabolism alterations due to insulin resistance accelerate the atherosclerotic process, leading to increased cardiovascular risk.8,14–23
In the knowledge that the presence of subclinical atherosclerosis has been linked to an increase in the risk of cardiovascular events10,24–26 and that patients with prediabetes are characterized by having multiple risk factors, insulin resistance and atherogenic dyslipidaemia, certain clinical implications may be drawn from our work. As the guides recommend, a high level of alert should exist to ensure early changes to healthy lifestyle habits (reducing calorie intake, a Mediterranean diet and regular moderate to intense exercise), while aggressively controlling cardiovascular risk factors such as hypertension and smoking.2 Given the high prevalence of SATp in this population, we believe that it could benefit from a simple study such as carotid Doppler ultrasound scan, to detect the presence of atherosclerotic plaque at an early stage and control dyslipidaemia and other cardiovascular risk factors more aggressively.27
LimitationsOur study has several limitations, and these should be pointed out. As it is an observational study it is unable to establish any causality. The observational nature of the study exposes it to multiple distortions, among which we underline the ones arising from the selection of the subjects and the recording of the different variables studied in medical registries. Our work contains a sub-register of active smoking that is surely associated with a problem in the data gathering for this variable, so that the influence of this variable on the final model cannot be ruled out. The population of study participants is composed of low-risk young individuals who visit our hospital for a routine cardiovascular assessment, so that they cannot be representative of the general population of our or any other country.
ConclusionsThis study found an association between prediabetes and a higher prevalence of SATp. This meant that the possibility of having subclinical atherosclerosis was 29% higher in subjects with prediabetes in comparison with the controls, following adjustment for age, sex, AHT and HDL-c. Hypertensive patients and those under the age of 55 years were the subgroups where the strongest association with SATp was found. We believe that these findings should lead to an early stratification of risk, to detect the subjects who require more aggressive interventions against cardiovascular risk factors.
FinancingThis work received no financing.
AuthorshipAll of the authors took part in data generation and in the revision of this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Fernando Botto for reviewing this manuscript.
Please cite this article as: Bozzo R, Rey R, Manente D, Zeballos C, Rostan M, Vitagliano L, et al. Asociación de placa ateroesclerótica y prediabetes. Estudio observacional con apareamiento por puntaje de propensión. Clin Investig Arterioscler. 2022;34:122–129.