Lifestyle is a complex concept that includes aspects external to ourselves that can modulate and influence our health. The knowledge of the relationship between lifestyle and cardiovascular risk does not attain the level of evidence achieved with clinical trials with drugs, because clinical studies are scarce and mainly of observational nature, albeit based on large cohorts. Nutritional epidemiology has the added difficulty of being based mostly on subjective dietary recall methods to ascertain nutrient and food intake over time, with the additional problems of incomplete data collection, variable measurements of adherence due to seasonal and geographical differences in food composition, and the changing eating behaviour that human beings have over time.
The purpose of this document is to carry out an updated and hierarchical review of the relationship between lifestyle and cardiovascular disease based on current evidence, paying attention to three aspects that are of great pathogenic importance and are directly modifiable: physical activity, tobacco consumption, and diet. With this, we intend to update the knowledge on this relationship, construct evidence-based recommendations, and provide a simple tool for clinical practice especially directed to health professionals involved in the care of people at cardiovascular risk, defining simple and easy strategies for individuals who receive advice for the primary and secondary prevention of cardiovascular diseases.
El estilo de vida es un concepto complejo que incluye los aspectos externos a nosotros mismos que pueden modular e influir en nuestra salud. Los conocimientos sobre la relación entre el estilo de vida y el riesgo cardiovascular están lejos de proporcionar los niveles de evidencia que se han conseguido con los ensayos clínicos con fármacos, debido a que los estudios son escasos, fundamentalmente de tipo observacional y en grandes cohortes, con la dificultad añadida de la no existencia de métodos seguros para conocer con precisión la ingesta diaria o lo largo de tiempo, así como la dificultad en la recogida de datos y en la medición de la adherencia debido a diferencias en la composición de los alimentos en distintas épocas y a la conducta alimentaria cambiante que posee el ser humano a lo largo del tiempo.
En este documento nos hemos propuesto llevar a cabo una revisión actualizada y jerarquizada en base a las evidencias actuales, prestando atención a tres aspectos que tienen gran importancia patogénica y que podemos modificar directamente: la actividad física, el consumo de tabaco y el patrón de alimentación. Con ello pretendemos actualizar los nuevos conocimientos sobre su relación con el riesgo cardiovascular aportando evidencias útiles, constituyendo una herramienta sencilla dirigida especialmente a todos los profesionales de la salud implicados en el cuidado de personas con riesgo cardiovascular para trasladarlos a la práctica clínica, definiendo unas líneas de actuación sencillas y fáciles para ser transmitidas a las personas que reciban un consejo para la prevención primaria y secundaria de las enfermedades cardiovasculares.
With advances in knowledge about human biology, the complexity of chronic disease pathogenesis has become evident. However, we know that health depends not only on scientific and technological advances, but also on the growing importance of intelligence and effort to make the right decisions regarding lifestyle at a personal and social level. Hence the importance of offering people clear, safe and practical advice that they can use as a tool to improve their health. Lifestyle is a complex concept that includes external aspects which can modify and influence our health. These aspects include level of education, the social environment in which people live, the physical environment (including quality of water and air), personal health practices (including diet and physical activity), healthy development during childhood and the quality of healthcare services. This document addresses three aspects of great pathogenic importance that we can directly modify, namely: physical activity, smoking and eating pattern. With this, we intend to provide updated information on their relationship with cardiovascular risk and provide doctors with a simple tool that can be used to apply such information in clinical practice, by defining simple and easy lines of action to be applied with people receiving cardiovascular disease prevention advice.
Awareness of the relationship between lifestyle and cardiovascular risk is far from providing the levels of evidence that have been achieved with clinical trials with drugs. Although very useful, interventional studies on clinical primary endpoints are generally scarce. One example is the PREDIMED study,1 one of the most relevant clinical trials on the link between nutrition and cardiovascular risk. However, in most cases, such studies are not available so we have to rely on observational studies, especially large cohort studies. On the other hand, exploring the usefulness of diet in cardiovascular disease prevention has many weaknesses, especially when compared with drug studies. There are no safe methods for accurately determining what a person eats each day, year after year, due to the difficulty of collecting data, differences in food composition in different periods, the frequently changing behaviour of human beings over time, lack of tools to guarantee adherence, etc. However, to study the relationship between lifestyle and cardiovascular risk, we have access to very valuable information which is not available in pharmacological trials. This includes information provided by historical tradition, which allows us to understand the long-term impact of the lifestyle of different populations on health. We also have an ever-increasing number of studies with clinical trial designs investigating the relationship between lifestyle and multiple surrogate markers of cardiovascular risk. Some of these are of a clinical nature, such as body weight or blood pressure, while others are biochemical, such as lipid fractions, glucose metabolism, proinflammatory state or oxidative stress, which are very useful reflections of overall health and cardiovascular risk.
The objective of this document is to provide an updated review aimed at providing useful evidence organised into levels, although it is important to recognise that it is difficult to base such recommendations on the usual categories of clinical evidence. Nevertheless, we have developed recommendations using clinical trials, if available, observational studies on clinical evidence or surrogate markers and expert consensus. In summary, this document outlines three types of recommendations: Evidence A, based on clinical trials and meta-analyses incorporating quality criteria; Evidence B, based on prospective cohort studies and case-control studies; and Evidence C, based on expert consensus and opinion or extensive clinical practice. Such recommendations have been incorporated into each of the corresponding chapters, supported by applicable references. Finally, this document is aimed at all health professionals involved in the care of people at risk of cardiovascular disease so that they can help their patients, as the behaviours and recommendations outlined are useful in both the primary and secondary prevention of cardiovascular diseases (CVD).
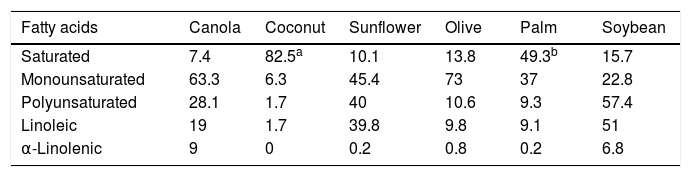
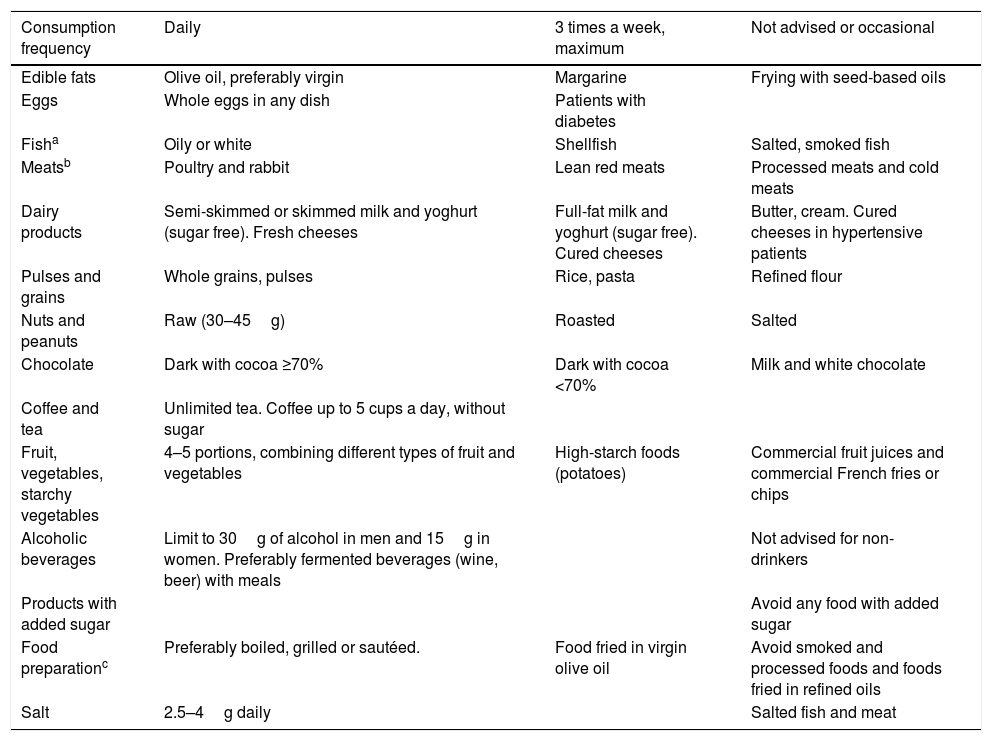
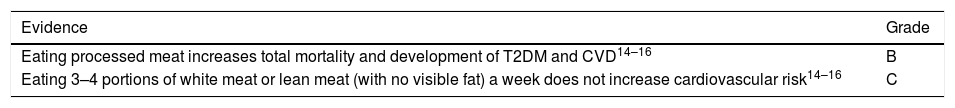
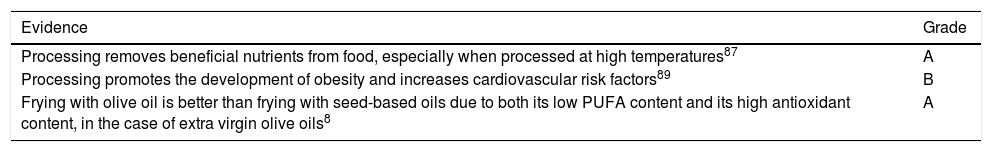
Food and cardiovascular riskEdible fatsOilsBy definition, oils contain 100% fat in the form of triglycerides, although the fatty acid composition varies greatly depending on the type of oil. These foods are made from oilseeds, such as corn, sunflower, rapeseed and soybean, or from fruits such as coconut, palm kernel and olive, and are used daily for cooking by large segments of the world's population, representing a significant energy source for consumers. Some oils, such as coconut and palm oil, are very high in saturated fatty acids (SFA), while others, such as canola (a variety of rapeseed), olive and high-oleic sunflower oil, contain very high proportions of monounsaturated fatty acids (MUFA). Soybean and sunflower oils are rich in n-6 polyunsaturated fatty acids (PUFA), while canola oil contains 10% n-3 PUFA (α-linolenic acid, plant-based omega-3) and soybean oil contains around 7% (Table 1). Oils produced by simply grinding most seeds and fruits are not suitable for consumption. To be edible and suitable for consumption, they must be refined using physical or chemical methods, including extraction, bleaching and deodorisation, procedures which retain the lipophilic molecules associated with the fat fraction, such as vitamin E and phytosterols, but which lose major hydrophilic components, such as polyphenols. Virgin olive oil, which is simply cold pressed and is therefore a pure olive juice, is notably different from other cooking oils since it contains very bioactive phenolic compounds, especially oleuropein and hydroxytyrosol.2
Mean fatty acid content in common cooking oils (grams per 100g).
| Fatty acids | Canola | Coconut | Sunflower | Olive | Palm | Soybean |
|---|---|---|---|---|---|---|
| Saturated | 7.4 | 82.5a | 10.1 | 13.8 | 49.3b | 15.7 |
| Monounsaturated | 63.3 | 6.3 | 45.4 | 73 | 37 | 22.8 |
| Polyunsaturated | 28.1 | 1.7 | 40 | 10.6 | 9.3 | 57.4 |
| Linoleic | 19 | 1.7 | 39.8 | 9.8 | 9.1 | 51 |
| α-Linolenic | 9 | 0 | 0.2 | 0.8 | 0.2 | 6.8 |
Mainly palmitic acid (C16:0).
Source: US Department of Agriculture Nutrient Database [consulted 10 July 2017]. Available at: http://ndb.nal.usda.gov/ndb/foods/list.
It has been known for some time that consuming SFA increases total cholesterol and low-density lipoprotein cholesterol (LDL-C), which leads to an increased risk of cardiovascular disease, while MUFA and PUFA have the opposite effect.3 Most clinical studies defining the lipid effects of different fatty acids used oils with different fatty acid compositions as the main source of fat. It is remarkable therefore, with surprisingly few exceptions, that there is little epidemiological or clinical trial-based evidence relating to the effects of different oils on the incidence of cardiovascular events. There are no data at all on canola oil, except for its beneficial effects on lipids, which is predictable based on its fatty acid composition. There are also no data on the cardiovascular risk of SFA-rich coconut oil, the consumption of which increases LDL-C, or soybean and sunflower oils, which, based on their unsaturated fatty acid composition, have the effect of reducing LDL-C when compared with SFA-rich oils. There is, however, at least one epidemiological study that suggests that palm oil is bad for cardiovascular health. The study in question is a case-control study on myocardial infarction (MI) conducted in Costa Rica, which observed an association between palm oil use and a higher risk of MI in comparison with soybean oil use.4
Olive oil stands out from other oils, not only because it has an affordable virgin variety, but because its cardioprotective properties and other healthy effects have been evaluated in numerous cohort studies and clinical trials, with endpoints of both intermediate markers and major cardiovascular events. It is a paradigmatic component of the Mediterranean diet that determines that this dietary pattern is much higher in fat (vegetable fat) than other healthy diets. The fat fraction mainly comprises the MUFA oleic acid (C18:1n-9), with small amounts of tocopherols and phytosterols. Virgin olive oil also contains very bioactive polyphenols, which are largely responsible for the health benefits of its consumption.2 When swapped for SFA or carbohydrates, MUFA reduce LDL-C and increase high-density lipoprotein cholesterol (HDL-C), thereby reducing the total cholesterol:HDL cholesterol ratio,3 as has been shown in various clinical trials with olive oil. There is also evidence of olive oil and its polyphenols having beneficial effects on endothelial function, inflammation and oxidation of LDL.2 A recent meta-analysis of 32 cohort studies linking MUFA exposure (of both plant and animal origin), olive oil, oleic acid and MUFA:SFA ratio to different health variables indicated that olive oil, but not MUFA, was associated with a risk reduction for all-cause mortality, with a relative risk (RR) of 0.77 (95% confidence interval [CI], 0.71–0.84), cardiovascular events (RR: 0.72; 95% CI: 0.57–0.91 and stroke (RR: 0.60; 95% CI: 0.47–0.77) when comparing the top and bottom thirds of the consumption distribution.5
Since extra virgin olive oil was one of the key foods supplemented in one of the arms of the PREDIMED controlled clinical trial, evaluating the effects of the Mediterranean diet on primary prevention of cardiovascular disease in high-risk individuals, first-level scientific evidence is available on the healthy effects of this oil. Therefore, after dietary intervention for 5years, the main results showed that participants assigned to the Mediterranean diet supplemented with virgin olive oil experienced a mean reduction of 30% in major cardiovascular events,1 apart from other beneficial effects on the risk of type 2 diabetes mellitus (T2DM), metabolic syndrome, hypertension (HTN), atrial fibrillation and others.6
MargarinesThese foods are water-in-oil emulsions that are stable and spreadable with a pleasant mouthfeel. They are produced by transforming a liquid food, such as oil, into an easily spreadable semi-solid. In the past, this was achieved by partial hydrogenation of unsaturated oils (converting double bonds of fatty acids to single bonds, i.e. creating SFA), which also created trans fatty acids (TFA). Scientific evidence that came to light in the 1990s relating to the harmful impact of TFA on lipids and cardiovascular risk led to a notable change in margarine manufacture, using more healthy starting materials (unsaturated vegetable oils such as soybean, sunflower or canola) in combination with technologies allowing the production of low-SFA products with practically no TGA (transesterification instead of hydrogenation) plus a higher content of essential n-6 (linoleic acid) and n-3 (α-linolenic acid) fatty acids.7 The nutritional composition of modern margarines is variable in terms of the proportion of fat to water, which ranges between 20% and 80% depending on the fat and energy content. They contain up to 50% PUFA, of which 10–20% are n-3 with only 20–25% SFA and <1% TFA. The current process used for manufacturing margarines allows vitamin E linked to the fat fraction of the original oil to be preserved and they also tend to be fortified with vitamins A and D. Since they are produced from seed oils, margarines and other common spreadable fats, such as mayonnaise, may be an important source of n-6 (linoleic acid) and n-3 (α-linolenic acid) PUFA for consumers, especially in Spain, where the intake of these essential fatty acids is fairly low.7
Levels of evidence for edible fats and cardiovascular risk
| Evidence | Grade |
|---|---|
| Virgin olive oil is the only cooking fat that effectively helps prevent cardiovascular diseases1 | B |
Recommendations
Based on the composition and cardiometabolic effects of common vegetable oils, there is little doubt that virgin olive oil is the most healthy and daily use is therefore recommended for both cooking and for drizzling over cooked foods. If the consumer wishes to use oils that are high in PUFA, such as canola, soybean and sunflower oil, these must be used cold as a dressing and not for cooking or frying since heat stress causes oxygen free radical-mediated auto-oxidation of the PUFA, generating aldehydes, lipopolysaccharides and other proinflammatory and atherogenic molecules.8 Virgin olive oil, however, stands up well to frying temperatures since it is low in PUFA and rich in antioxidants. Due to their high PUFA content, margarines must also not be used for cooking or frying, only for spreading.
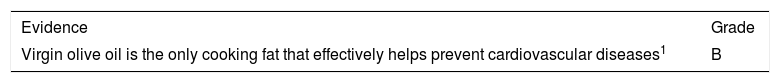
EggsUse of eggs, especially chicken eggs (fried in olive oil, scrambled, in potato frittata or on salads), is part of the Mediterranean gastronomic culture. The main component of eggs is ovalbumin, a protein of high biological value that contains all the essential amino acids, minerals (selenium, phosphorus, iodine and zinc), vitamins (A, D, B2, B12, pantothenic acid and niacin) and other carotenoids, such as lutein and its isomer zeaxanthin, which are important for retinal structure and function. In addition to their function as coenzymes, fat-soluble vitamins (A and D) and carotenoids have notable antioxidant and anti-inflammatory properties, with potential anti-atherogenic mechanisms. Eggs are also an important source of choline, an essential nutrient involved in the formation of cell membranes, and pregnant women must have an adequate dietary intake of choline since a lack of this nutrient can cause neural tube defects in the foetus.
Fat accounts for 11% of the edible portion of an egg. It is found in the yolk and basically comprises triglycerides and cholesterol, containing some 200–230mg of cholesterol per unit (350–385mg/100g). With regards to fatty acid composition, most are unsaturated, 5g/100g MUFA and 1.2g/100g PUFA, including α-linolenic acid, with only 3g/100g SFA. Due to their high cholesterol content, eggs have traditionally been associated with elevated total cholesterol and LDL-C levels and this is one of the reasons why egg intake is limited in dietary recommendations for cardiovascular disease prevention. However, clinical studies have shown that rises are minor, even more so in the context of low-SFA diets, although there is notable interindividual variability in response. Eggs also cause a slight increase in HDL-C and promote the development of large, less atherogenic LDL particles.9
Prospective studies do not support the idea that egg intake is associated with the development of coronary heart disease (CHD) and even suggest that eating one egg a day reduces the risk of stroke by 12%.10 Therefore, there seems to be no reason to restrict egg intake based on the view of reducing CVD.11 On this basis, the USDA Scientific Report of the 2015 Dietary Guidelines Advisory Committee does not limit dietary cholesterol intake when the main source is eggs.12 A recent meta-analysis of prospective studies also concluded that egg consumption increases the risk of T2DM in US cohorts, but not in European and Asian cohorts,13 perhaps because of ecological differences in food patterns and eating habits.
Levels of evidence for egg intake and cardiovascular risk
| Evidence | Grade |
|---|---|
| Both the healthy general population and people with high-risk factors (prior CHD or T2DM) can consume up to one egg a day without increasing their cardiovascular risk10,11,13 | B |
Recommendations
Although different nutritional guidelines include conflicting egg intake and health recommendations, current scientific evidence suggests that their consumption is not harmful in the context of a healthy diet. Both the healthy general population and people with high cardiovascular risk factors (prior CHD or T2DM) can consume up to one egg a day without affecting their cardiometabolic health.
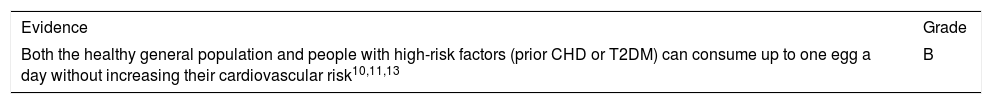
MeatLike fish and eggs, meat is a rich source of high biological value protein, which, whether red or processed, has a relatively high content of SFA, palmitic acid (C16:0) and stearic acid (C18:0). It also contains cholesterol, B-group vitamins and minerals, such as iron, potassium, phosphorus and zinc. The fat content in different types of meat is variable and is lower in white meat (chicken, turkey and rabbit) than in red meat and lower in pork than in veal or lamb. The fat content is also highly influenced by its anatomical origin, with pork loin containing less fat than ribs or bacon. In lamb, the fat content is lower in leg meat than in chops, and in veal skirt or flank steak the fat content is four times as much as in sirloin. Another determining factor is the type of animal feed used, which modifies both the quantity and quality of fat. There is less intramuscular fat in grass-fed cattle than in grain-fed cattle, but the quality of fat also varies from one species to another since there are less diet-induced changes in ruminants than in animals with one stomach, such as pigs and poultry, because microbial activity in the rumen converts unsaturated fatty acids from the diet into SFA. Lean pork contains a high percentage of oleic acid, which accounts for 44% of the total fatty acids in white pig fat and 49% in Iberian pigs, both fed with grain. The highest content (55%) is observed in acorn-fed Iberian pigs (which gives a higher concentration of unsaturated fat in their diet). Recent evidence shows only a slight link between the consumption of unprocessed red meat and the risk of CHD, stroke, T2DM or total and cardiovascular mortality.14–16 Red meat also has little effect on lipid profile or blood pressure. There is, however, a consistent relationship between processed meat and CVD and total mortality. Red and processed meat have a similar SFA and cholesterol content, which indicates that these differences are attributable to other components, such as TFA or the fact that processed meat contains much more sodium and potentially harmful molecules, including nitrites and nitrates.7
Levels of evidence for meat and cardiovascular risk
Recommendations
Unprocessed meat should be eaten in moderation, 3–4 times a week. Lean and white meat are preferable and all visible fat should be removed before cooking. Processed meat and meat by-products are not recommended and should only be eaten occasionally.
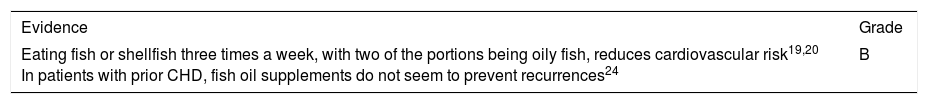
Fish and shellfishThese foods are the main dietary sources of long-chain n-3 PUFA, including eicosapentaenoic acid (EPA, C20:5n-3) and docosahexaenoic acid (DHA, C22:6n-3).9 They are especially abundant in oily fish (sardine, anchovy, tuna, herring, mackerel, salmon, trout, etc.), while white fish (cod, hake, monkfish, sole, megrim, etc.) contain a much lower concentration. These fatty acids accumulate in the liver of the fish and cod liver is the usual source for n-3 PUFA-rich fish oil. Such fatty acids are generally more abundant in wild fish than in farmed fish, depending on the type of food they are given and also on the season, as fish have a higher fat content in summer.
Available evidence on fish and marine n-3 PUFA comes mainly from epidemiological studies. One meta-analysis of 16 cohort studies with n=422,786 observations, focusing on fatty acids from dietary intake and the risk of CVD, showed a significant benefit of EPA/DHA intake (RR: 0.87; 95% CI: 0.78–0.97).17 Likewise, a consortium of 19 observational studies from 16 countries found that concentrations of EPA/DHA in plasma or adipose tissue (biomarkers of EPA/DHA intake) were associated with a lower incidence of fatal CVD and myocardial infarction on comparing quintile 5 and quintile 1.18 In another meta-analysis of data from 19 cohorts, increasing intake of any type of fish by two portions a week was associated with a slight decrease in cardiovascular risk, especially a decrease in ischaemic stroke.19 An analysis of eight prospective studies also showed a 5% reduction in acute myocardial infarction risk with each additional 100-g serving of fish per week.20
An important aspect to consider is the presence of other nutrients (amino acids such as taurine, selenium, iodine, vitamin D and choline), besides n-3 PUFA, in fish, which may contribute to the improvement in cardiovascular health observed with fish consumption. Concerns have been raised over the presence of pollutants (such as methylmercury, dioxins and polychlorinated biphenyls) in predatory fish and the safety of their consumption, but the benefit of such consumption seems to outweigh the potential risks.21 Mercury derivatives found in seas and oceans get into the food chain, reaching a higher concentration in larger fish and predatory fish, such as sharks, mackerel, swordfish and bluefin tuna. In theory, pollutants found in this type of fish can affect foetal development, which is why it is traditionally recommended that children and women of child-bearing age, especially pregnant and breastfeeding women, avoid consuming such fish.12 However, given that n-3 PUFA from fish, especially DHA, are essential for development of the foetal nervous system, breastfeeding women are advised to eat smaller fish. In one analysis of around 12,000 pregnant women, children born to mothers who consumed less than two portions of fish a week had a lower performance in intelligence, behaviour and development tests than those born to mothers who ate fish at least twice a week.22 Therefore, the benefit of consuming fish seems to significantly outweigh the potential risk of pollutants, which are more abundant in fish such as mackerel, swordfish, bluefin tuna and shark.
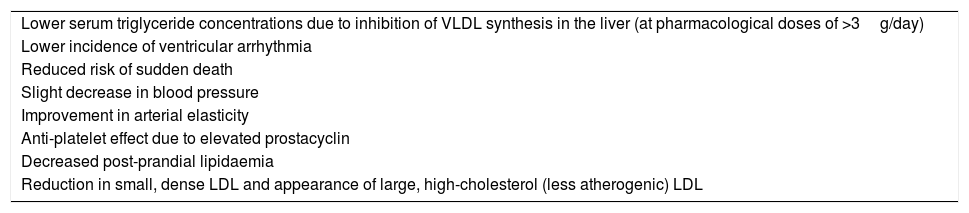
The benefits of fish consumption, especially oily fish, are attributable to their high n-3 PUFA content, which induces multiple favourable biological effects, summarised in Table 2. A reduced risk of fatal myocardial infarction and sudden cardiac death has generally been described in primary prevention. Nevertheless, in the latest meta-analyses of epidemiological observations and randomised clinical trials, in high-risk patients or secondary prevention, a lower risk of total mortality, myocardial infarction or stroke has not been confirmed. These results have been partly attributed to better treatment of all risk factors in these patients, in which there is little margin for additional preventive effects of n-3 PUFA.7 In one recent document of recommendations, the American Heart Association (AHA)23 indicates, based on findings from clinical studies, that in patients with prior CHD, marine n-3 PUFA supplements (1g/day) may reduce the risk of fatal relapse, possibly by reducing sudden cardiac death, but not the risk of non-fatal recurrence, and it therefore concludes that treatment with n-3 PUFA is reasonable in the secondary prevention of CHD. However, a recent meta-analysis of 10 large randomised clinical trials with around 78,000 participants concluded that n-3 PUFA supplements (about 1g/day) has no significant effect on fatal or non-fatal CHD or other vascular events.24 The latest evidence, therefore, does not support the administration of fish oil supplements to patients with CHD.
Beneficial effects of n-3 PUFA on the cardiovascular system.
| Lower serum triglyceride concentrations due to inhibition of VLDL synthesis in the liver (at pharmacological doses of >3g/day) |
| Lower incidence of ventricular arrhythmia |
| Reduced risk of sudden death |
| Slight decrease in blood pressure |
| Improvement in arterial elasticity |
| Anti-platelet effect due to elevated prostacyclin |
| Decreased post-prandial lipidaemia |
| Reduction in small, dense LDL and appearance of large, high-cholesterol (less atherogenic) LDL |
Levels of evidence for fish and cardiovascular risk
Recommendations
Encouraging people to eat fish is an important component of lifestyle modifications to prevent CVD. A significant benefit could be obtained by simply swapping meat for fish as the main dish. A good recommendation for reducing cardiovascular risk would be to eat fish or shellfish at least three times a week, with two portions being oily fish. Pregnant women and children should avoid bluefin tuna, dogfish, swordfish and mackerel.
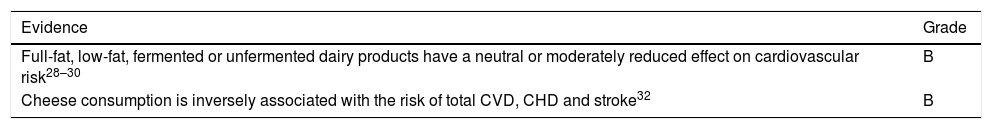
Dairy productsMilk and dairy products provide various nutrients, including proteins, fats (especially saturated), carbohydrates and minerals, such as potassium, phosphorus, magnesium and calcium. In addition to being the most important dietary source of calcium, dairy products provide micronutrients, such as vitamin D, a deficiency of which has been associated with various pathologies, ranging from mental health problems to cancer, although the only clear scientific evidence is that linking it to osteoporosis. With regards to calcium, a meta-analysis of data from 12 cohort studies shows a U-shaped association between calcium intake and cardiovascular mortality. The greatest benefit is obtained with an intake of 800mg/day, with gradual increases in risk at intakes both above and below 800mg/day.25 Another potential benefit of dairy products is the presence of vasoactive peptides, which have an anti-hypertensive effect due to inhibition of angiotensin-converting enzyme, for which evidence is still limited.26 Various epidemiological studies have also concluded that plasma concentrations of pentadecanoic acid (C15:0) and heptadecanoic acid (C17:0), specific SFA of milk, are associated with a reduced risk of CHD and T2DM,27 an example of how the whole food (in this case milk) is once again more relevant to cardiovascular risk than its isolated nutrients (in this case SFA).
Studying the association between dairy products and health is complicated given the large number of available products, ranging from whole milk to fermented milk and including different kinds of yoghurt and milks with very different fat contents. Dairy products are considered to have little influence on cholesterolaemia, although their consumption is associated with a lower risk of hypertension according to the results of two meta-analyses, and there is evidence suggesting that they do not increase cardiovascular risk. Furthermore, one recent meta-analysis shows an inverse relationship between total dairy intake and the risk of CVD and stroke, while no relationship is shown for CHD.28 However, another meta-analysis of 31 cohort studies found an inverse association between low-fat dairy intake and the risk of CHD, with a neutral association with full-fat dairy products.29 A consistent inverse relationship has also been found between total dairy intake and the risk of stroke, especially with low-fat dairy products.30 In the case of T2DM, intake of such dairy products may reduce its incidence, although it is important to take into account the presence of added sugars in many such products, which could counteract this protection. Yoghurt consumption promotes favourable alterations in the microbiota of obese and diabetic individuals, with improved glycaemic response and insulin resistance. Yoghurt also increases the concentration of glucagon-like peptide (GLP)-1, which has an anorexigenic effect, and may play a role in its protective effects on obesity and T2DM. There is moderate-quality evidence supporting a neutral association between yoghurt consumption and the risk of CVD (CHD and stroke),29,30 although, after reviewing the results of five meta-analyses, higher yoghurt consumption appears to be associated with a significantly lower risk of T2DM.30 Furthermore, the relationship between total fermented dairy consumption and the risk of CVD is based on low-quality studies that cannot be used to reach clear conclusions.31
Cheese consumption does not alter lipid profile, as may be expected due to its high SFA content. Fermented cheeses contain andrastin, a fungal metabolite with cholesterol-lowering properties since it inhibits farnesyltransferase, an enzyme that modulates cholesterol synthesis. The aforementioned meta-analysis by Drouin-Chartier et al.30 suggests that cheese consumption is inversely related to T2DM risk. A recent meta-analysis of 15 prospective studies32 also found that, compared with low cheese consumption, high cheese consumption was associated with a 10–14% reduction in the risk of total CVD, CHD and stroke. There was also a U-shaped association between cheese consumption and CVD, with the largest reduction in risk observed at a cheese intake of approximately 40g/day. Furthermore, cured cheeses contain significant amounts of salt and are therefore not recommended in hypertensive patients.
Although dietary recommendations for cardiovascular disease prevention prefer the consumption of low-fat dairy products, moderate- to high-quality evidence suggests that the total intake of dairy products, cheese and yoghurt has a neutral effect on the risk of CVD and we can therefore state that, regardless of its fat content, consumption of such foods does not increase cardiovascular risk. However, there is high-quality evidence associating low-fat dairy and yoghurt consumption with a reduced risk of T2DM, although this relationship has also been observed to a lesser extent with total dairy and cheese intake.30 More studies are required to compare the impact of low-fat dairy intake and full-fat dairy intake with CVD. The heterogeneity of dairy products can make it difficult to reach a conclusion since benefits attributable to dairy products are generally different for each specific dairy product.
Levels of evidence for dairy products and cardiovascular risk
Recommendations
It is recommended that individuals eat at least two servings of dairy products (milk, fermented milk, yoghurt, cheese, etc.) a day, especially due to their important nutritional role in calcium metabolism and their high content of high biological value protein. Restricting dairy intake does not seem to be an appropriate strategy for reducing cardiovascular risk, although regular consumption of dairy products containing added sugars and cured cheese by hypertensive individuals is not recommended. To prevent cardiovascular disease, reduced consumption of concentrated milk fat, such as butter and cream, is recommended.
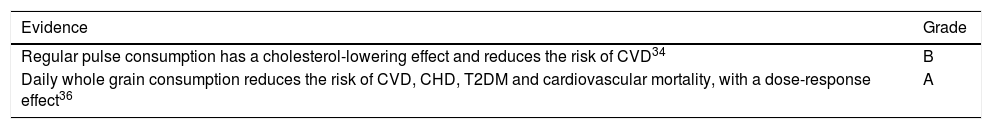
Pulses and grainsThese foods are seeds with a high calorie density. They have complex matrices with a very high content of nutrients and phytochemicals, aimed at sustaining future plant growth and protecting its DNA, thus allowing perpetuation of the species. The most common pulses eaten in Spain are lentils, beans, chickpeas and peas, followed by broad beans and soya beans. Their main components are starch, a complex carbohydrate (15–27%) with a high fibre content, and proteins (5–9%), which have a lower biological value than proteins from animal sources since they do not contain all the essential amino acids, such as methionine. They have a very low fat content (0–2.5%) and contain micronutrients such as a high content of B-group vitamins, folic acid, calcium, potassium and non-heme iron. They also contain bioactive phytochemicals, such as phytosterols and saponins, which reduce cholesterol absorption in the intestines, and strong polyphenol-type antioxidants.33 With regards to the role of pulses in cardiovascular disease prevention, a recent meta-analysis of prospective studies showed that consumption of 100g of pulses (4 times/week) was associated with a 14% decrease in CHD risk, with no obvious effect on the risk of stroke or T2DM.34 The cardioprotective effect of pulses is partly due to their cholesterol-lowering effect, with reductions in total cholesterol (7.2%), LDL (6.2%) and triglycerides (16.6%) following consumption of one daily serving, according to a meta-analysis of clinical studies. However, data regarding the presumed blood pressure-lowering effect of pulses are not very convincing.35 These foods have a low glycaemic index and reduce postprandial blood glucose and insulin levels, justifying promotion of their consumption in diabetic patients, although there is no clear evidence that they reduce the incidence of T2DM. Clinical studies with pulse diets have shown that pulse consumption for six weeks is associated with lower body weight and waist circumference than control diets, which may be due to their satiating effect, modulating short-term food intake as occurs with nuts.
The most common grains in our diet are wheat, rice and corn, followed by oats and then smaller amounts of barley and rye. Grains are rich in complex carbohydrates (65–75% of their total weight), with moderate levels of proteins (3–16%), which are biologically incomplete due to lacking lysine and, in the case of corn, tryptophan. Grains also have a low fat content (1–6.5%, mainly unsaturated) and, like other seeds, whole grains are rich in B-group vitamins, vitamin E, minerals (potassium, calcium, magnesium, phosphorus, iron, zinc and silicon) and other phytochemicals with antioxidant properties (polyphenols). Whole grains contain all three parts of the grain (bran, endosperm and germ) in the same proportion as the original grain seed. During refining processes, the bran and germ are removed, which reduces the health benefit of the grains since they maintain their starch content but lose part of the proteins and most vitamins, minerals and phytochemicals. Consumption of whole grains has been associated with a lower cardiovascular risk, as indicated in a meta-analysis of observational studies in which the daily dose of 48–80g was associated with around a 20% reduction in the risk of CHD, stroke and cardiovascular mortality. Mortality from cancer, T2DM and other causes was also reduced. These studies suggest the existence of a dose-response effect since a higher consumption was associated with a higher reduction in the risk of CVD mortality (26–36%).36 Another recent meta-analysis concluded that there is an inverse association between whole grain intake and T2DM occurrence, with a dose-response relationship and a 20% reduction in the T2DM risk after consuming three daily servings of 45g.37 However, various clinical studies have demonstrated modest benefits of whole grains in terms of glycaemic control and total and LDL cholesterol. Of particular interest is the effect of beta-glucan on lipid metabolism, as recognised in a recent meta-analysis in which oat and barley consumption (>3g/day) reduced LDL-C by 12mg/dl.35
An essential component of whole grains is dietary fibre, which is responsible for some of the beneficial effects of regular whole grain consumption. It comprises carbohydrates that are resistant to digestion and absorption in the small intestine, with complete or partial fermentation in the colon. It has a heterogeneous chemical composition (polysaccharides, oligosaccharides, lignin and associated plant substances) and can be soluble or insoluble in water. It is widely found in whole grains (fibre found in wheat and corn is mainly insoluble, while that in oats and barley is mainly soluble), but is also found in pulses and nuts.33 Whole grains contain up to 20g/100g of insoluble fibre, which effectively relieves constipation and regulates bowel transit, while the soluble form promotes lower glycaemic responses, helping to achieve better blood glucose and insulin control. Both forms of fibre help control body weight by increasing satiety. They are also essential for maintaining the balance of gut microbiota, as discussed in the corresponding section. Quinoa is a pseudocereal that is known for being one of the few plant foods to contain all essential amino acids in its protein, which accounts for about 20% of its weight. Quinoa has a lower glycaemic index, helps control body weight due to its satiating effect and is gluten free, meaning it is suitable for coeliac patients.
Levels of evidence for pulses, grains and cardiovascular risk
Recommendations
To promote cardiovascular health and help reduce cholesterolaemia, one serving of pulses at least four times a week is recommended. The recommended consumption of whole grains is 4 servings/day, including bread with all meals, pasta 2–3 times/week and rice 2–3 times/week. Our wise custom of combining grains and pulses in the same meal (e.g. rice with lentils) is interesting as this completes the amino acids that are missing from each food type, resulting in a complete mix of high biological value proteins.
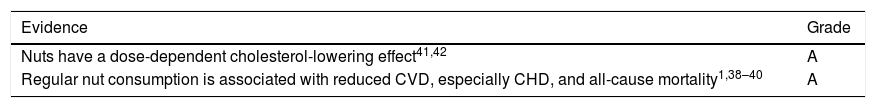
NutsNuts (almonds, hazelnuts, walnuts, pistachios, cashews, macadamias, pine nuts, etc.) are unusual seeds due to their high fat content, which tends to exceed 50% of the energy they contain. Their fat content primarily comprises unsaturated fatty acids, either oleic acid-type MUFA (in almonds, hazelnuts and other nuts) or n-6 (linoleic acid) and n-3 PUFA, such as α-linolenic acid (found in walnuts), with a very low SFA content. Although peanuts are actually pulses/legumes and not tree nuts, they are similar in composition and high unsaturated fatty acid content to nuts, both from a nutritional point of view and in terms of biological effects. Apart from their high fat content, nuts, like all seeds, contain large amounts of fibre, antioxidants, potassium, calcium, magnesium and numerous phytochemical compounds with strong biological activity. These are largely found in the pellicle, or inner skin, which is why raw, unpeeled nuts that have not been roasted are recommended.38
People began to be interested in nuts as a result of epidemiological evidence showing that regular consumption reduced the risk of CHD, a protective effect that includes all-cause mortality, total CVD, CVD mortality, CHD mortality and sudden cardiac death, according to a recent meta-analysis.39 A later meta-analysis analysed additional prospective studies associating nut consumption with various pathologies, which reached similar conclusions, with the addition of a beneficial effect on mortality from diabetes, cancer, respiratory disease and infectious disease.40 Nut consumption has also been associated with a lower risk of diabetes and hypertension.38 The PREDIMED study on the primary prevention of cardiovascular disease has provided first-level scientific evidence on the benefit of nut consumption, showing a 30% reduction in the incidence of CVD (myocardial infarction, stroke or death from cardiovascular disease) after 5years assigned to a Mediterranean diet supplemented with either extra virgin olive oil or nuts (30g per day: 15g of walnuts, 7.5g of almonds and 7.5g of hazelnuts) in high-risk individuals.1
The cardioprotective effect may be partly due to the effects of nuts on lipid levels. Many short and medium-term dietary intervention trials have effectively demonstrated, both in healthy volunteers and in patients with hypercholesterolaemia, that daily consumption of a reasonable quantity of nuts has a clear and consistent cholesterol-lowering effect.41 The nuts studied the most are almonds and walnuts, although positive results have also been published for studies using other types of nuts, such as peanuts, and therefore the cholesterol-lowering effect can be considered common to all types. The reduction in total cholesterol and LDL-C varies between 5% and 15% with a daily intake of 30–75g and is related to baseline measurements, i.e. the higher the baseline cholesterol, the more effective the reduction. The reduction also depends on body mass index with thin individuals responding better than obese people. Nuts do not produce significant changes in HDL-C, while triglycerides are only reduced if they are high at baseline, not in individuals with normal triglyceride levels.41 It must be noted that the cholesterol-lowering effect has been observed on comparing nut diets with other healthy diets, such as the Mediterranean or Japanese diet. A recent meta-analysis of 61 clinical trials concluded that each daily serving (around 30g) of nuts lowers total cholesterol and LDL by an average of 5mg/dl, apoB 4mg/dl (more so in diabetics than in individuals who do not have diabetes) and triglycerides 2mg/dl.42 No significant effect on blood pressure was detected in this meta-analysis.
A maximum reduction in cholesterol of 10% is equivalent to a 20% decrease in coronary risk, which is lower than that observed (around 34%) in epidemiological studies with nuts, suggesting that nuts may have a cardioprotective effect as well as lipid-lowering activity. In comparison with a Mediterranean diet, a nut-rich diet has been shown to reverse endothelial dysfunction associated with hypercholesterolaemia, independently of cholesterol reduction, and also to reduce inflammation.38 This beneficial effect of nuts may be due to both their α-linolenic acid and their arginine or antioxidant content.
Since nuts have a very high fat content and are high in calories, there is a concern that regular consumption may be associated with undue weight gain. There is currently plenty of evidence from clinical trials suggesting that nuts, when added to your usual diet (with no recommendations to cut out other foods to reduce calorie intake) or when used to replace another source of dietary fat, do not induce weight gain. The main explanation for this apparent contradiction is the high satiating effect of nuts, meaning that, whether eaten during the day or as an appetiser, the calories consumed are offset by reducing the amount of food consumed during the next meal.43 Also, part of the fat (up to 20%) is not absorbed by the gut since it is contained in the nut cell membranes, aiding defaecation.
Levels of evidence for the relationship between nuts and cardiovascular risk
Recommendations
Regular consumption (daily or at least three times a week) of a handful of nuts (equivalent to one 30-g serving) is highly recommended for cholesterol control and overall health. These should be eaten raw and unpeeled (not roasted or salted), if possible, since most of the antioxidants are found in the inner skin. To maintain the satiating effect and avoid weight gain, nuts should be eaten during the day, not as a dessert after dinner. This recommendation applies to all individuals of any age (from 5years onwards). The only contraindication is in the event of an uncommon nut allergy (peanut allergy in children is the most common).
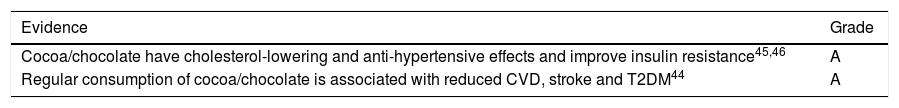
Cocoa and chocolateLike other seeds, cocoa contains many beneficial nutrients and phytochemical compounds. Its main by-product for consumption is chocolate, of which there are many varieties containing different ingredients. Dark chocolate contains a higher proportion of cocoa and less milk and sugar. Its composition includes 45–60% complex carbohydrates, 30–40% fat and up to 7% proteins, in addition to abundant potassium and magnesium, phytosterols and polyphenols from the flavonoid family.33 Although a large part of the fat in cocoa is SFA, stearic acid predominates, which has no cholesterol-raising effect. The results of 14 prospective studies, with data from more than 500,000 participants, analysed in a recent meta-analysis have associated increased consumption of any type of chocolate with a lower incidence of CHD, stroke and T2DM, concluding in a dose-response analysis that the maximum benefit is obtained when consuming 2–3 servings/week of 30g of chocolate.44 Numerous clinical trials have been conducted with dark chocolate or similar products to evaluate their effect on cardiometabolic risk variables, the results of which have also been added to the meta-analysis, consistently showing improvements in endothelial function and reductions in blood pressure and cholesterolaemia, with increased HDL-C. Improved glycaemic control and insulin resistance has also been described. As with other nutritional or pharmacological interventions, beneficial effects of chocolate have been observed to be greater in the presence of cardiovascular risk factors.45 A more recent meta-analysis confirmed the beneficial effects of cocoa on these risk biomarkers and also indicated reductions in inflammatory molecules and endothelial activation.46 It must be noted that some of these clinical trials have used isolated flavonoids of cocoa instead of chocolate, with the same beneficial effect observed on blood pressure and endothelial function, showing that these phytochemicals, which promote nitric oxide synthesis, are a major bioactive component of cocoa.47 Despite their high energy content, there is no evidence that regular dark chocolate consumption makes you fat, probably due to having a satiating effect similar to nuts.
Levels of evidence for the relationship between cocoa/chocolate and cardiovascular risk
Recommendations
Each individual can consume as much dark chocolate as they like on a daily basis to reduce cardiovascular risk as part of a healthy diet. There is no fear of dark chocolate consumption causing undue weight gains, although it should be consumed during the day and not at night after dinner since the satiating effect can then not be offset by eating less at the next meal.
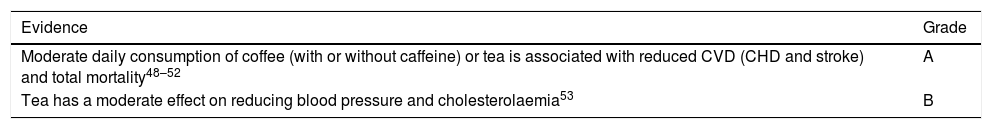
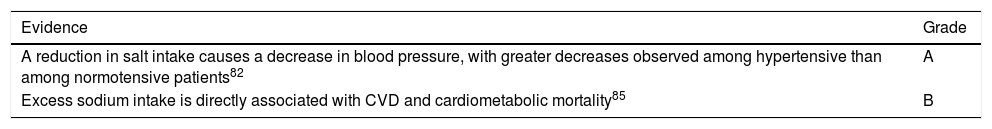
Coffee and teaCoffee and tea are two of the most consumed beverages around the world and are rich in biologically active polyphenols, such as antioxidants and anti-inflammatories, which give them their characteristic bitter taste. Brewed coffee maintains high concentrations of potassium and polyphenols (mainly chlorogenic acid) from the original beans, as well as caffeine, an alkaloid with stimulant properties. Coffee has been studied extensively in prospective studies in relation to the incidence of CVD and T2DM. A meta-analysis of 36 studies detected a non-linear inverse relationship (U-shaped curve) between coffee consumption and CVD, with a greater risk reduction (15%) with moderate consumption of between three and five cups/day and a similar protective effect for CHD and stroke, but no apparent effect with consumption of more than five cups/day or decaffeinated coffee.48 Long-term coffee consumption, including decaffeinated coffee, has also been associated with a moderately reduced risk of metabolic syndrome and T2DM and a lower risk of cardiovascular or all-cause mortality.49 The results of two large prospective studies have recently been published confirming an inverse relationship between coffee consumption and all-cause and cause-specific mortality.50,51 Coffee can acutely increase blood pressure, but there is no evidence that chronic coffee consumption stimulates the onset of HTN, and it has even been associated with a lower risk of HTN in some studies. Unfiltered coffee contains cafestol, a diterpene that increases cholesterol, but this is not the case with filtered or instant coffee.33
Tea infusions are rich in polyphenols from the flavonoid family, specifically catechins. To produce black tea, leaves from the Camellia sinensis plant are oxidised in a climate-controlled environment, while green tea is made from whole, intact leaves. Regular consumption of both varieties of tea has been linked to better cardiovascular health, with a 20–25% reduction in the incidence of CVD, both CHD and stroke, and total and cardiac mortality for every three cups of tea/day according to the latest meta-analysis of prospective studies, although results were heterogeneous.52 Evidence from randomised clinical trials also shows that daily consumption of both varieties of tea moderately reduces blood pressure and total and LDL cholesterol.53
Levels of evidence for the relationship between coffee and tea and cardiovascular risk
Recommendations
Regular consumption of up to five cups of coffee (filtered or instant, regular or decaffeinated) or tea (green or black) a day is beneficial for cardiovascular health. Tea also reduces cholesterolaemia. Both beverages are therefore recommended for healthy individuals and people with cardiovascular risk factors. These beverages are low in calories, unless sugar is added, which must be limited or omitted by people who are overweight, have T2DM or atherogenic dyslipidaemia.
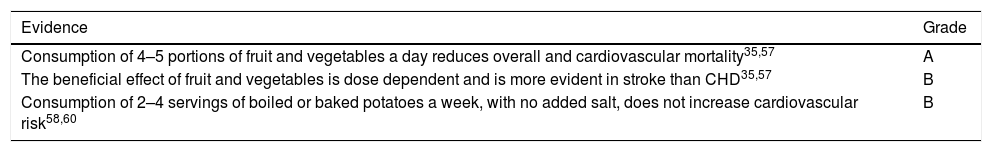
Vegetables, fruits and tubersLeafy vegetables, mushrooms, green vegetables and fruit all have a high water content (70–90%) and are low in calories, predominantly due to their carbohydrate content, which is higher in fruit. However, they have a low fat content, containing predominantly unsaturated fats with a few exceptions, such as olives and avocados, which contain 15% fat in the form of MUFA, and coconut, with 33% fat, predominantly SFA. As a result of fruit preservation procedures, their energy and carbohydrate content (especially sugars) can be increased, as is the case with plums, raisins and dried figs, and especially jams and preserves.
These foods also contain similar amounts of fibre and other biocomponents with multiple health functions, such as phenolic compounds and vitamins A, C and E, which have useful antioxidant effects for cardiovascular protection and other ageing-related processes. These foods are widely available and are eaten in different ways, such as in salads, stews and typical Spanish dishes, such as gazpacho, salmorejo (cold tomato soup) or sofrito (Spanish sauce), which is the base ingredient of many cooked dishes. It is important to recognise that culinary preparation can affect the bioavailability of different components found in these foods, sometimes increasing and sometimes reducing their content, as is the case with antioxidants. According to one meta-analysis, parboiling, boiling, roasting, microwaving and pressure cooking can reduce the concentration of phenolic compounds by up to 50%. Whenever possible, it is therefore advisable to eat these foods raw as part of a Mediterranean diet.54 One common and ill-advised habit is the consumption of industrial fruit juices instead of freshly squeezed juices. Although they may retain certain properties of the original fruit, their fibre content and part of their natural antioxidants are lost, while the calorie density is often increased due to added sugars. They are therefore not recommended since they are more like sugary soft drinks than original freshly squeezed juice. However, freshly squeezed juices are also less complete than the original fruit because, although they still contain most of the fruit's nutrients, including antioxidants, the essential fibre content is lost as it is left behind in the juicer.55
With regards to epidemiological evidence, a recent meta-analysis of 95 observational studies concluded that fruit and vegetable consumption reduces the risk of CVD.56 Consumption of one daily serving of both reduced all-cause and cardiovascular mortality by between 2% and 8%, in a dose-dependent fashion, and, therefore, a higher benefit is expected with a higher number of servings. Thus, 200g a day of fruit and vegetables reduced the relative risk by 8% for CHD, 16% for stroke, 3% for cancer and 10% for all-cause mortality.56 In the PREDIMED study, participants who consumed nine or more portions of fruit and vegetables a day were seen to experience a 40% reduction in CVD compared with those who consumed five or less portions a day.57 All epidemiological evidence suggests that fruit and vegetable consumption is associated with greater protection from stroke than CHD. The underlying reason for this could be that all plant-based foods have a low sodium and high potassium and magnesium content, which helps reduce blood pressure.35 Their effect on other cardiovascular risk factors, however, is not clear. Also, no controlled clinical trials have been conducted to evaluate the effect of fruit and vegetables on clinical events of CVD. The high fibre, antioxidant and mineral content of fruit and vegetables are thought to have a beneficial effect on multiple atherogenesis-related mechanisms. Moreover, there is no doubt that these products are the centre of any healthy and balanced eating pattern, both in healthy individuals and in those with any level of cardiovascular risk.
Tubers (potatoes, cassava, sweet potatoes, yam and beetroot) are thickened underground stems where nutrients are stored. They contain a high percentage of water (77%) and complex carbohydrates, specifically starch (18%), with a low protein (2.5%) and very low fat (0.2%) content and a high glycaemic index. They also contain mostly soluble fibre (2g/100g) and various minerals, such as potassium, iron, phosphorus, calcium, magnesium and zinc. Their vitamin content, which is found mainly in the skin, is low and is largely lost during storage and cooking. In specific terms, a baked potato contains 80 calories/100g, which is similar to all other tubers, but this calorie content can triple when fried or added to stews. Beetroot contains less calories (46g/100g), while sweet potato has a high beta-carotene and folic acid content. It has been suggested that tubers help control blood pressure due to their potassium content, but there is not sufficient scientific evidence to support this hypothesis. Instead, the results from three large US cohort studies have shown an association between the consumption of four or more servings of potatoes a week (boiled or baked) and the development of hypertension, which increases with French fries or chips.58 Nevertheless, this presumed harmful effect of potatoes may be due to the fact that potatoes tend to be prepared using unhealthy fats in the US. According to a recent analysis of the PREDIMED and SUN cohorts, there seems to be no association between potato intake and blood pressure or incidence of hypertension in Spain, which is due to the fact that potatoes in the Spanish diet are consumed with vegetables or pulses and olive oil.59 A recent meta-analysis of observational studies found no association between potato intake and the risk of obesity, T2DM and CVD, except in the case of French fries or chips, which increases the risk of T2DM.60 Replacing potatoes with an equal quantity of whole grains as the main source of carbohydrates reduced the risk of incident T2DM by 18–20%.
Levels of evidence for the relationship between fruit, vegetable and tuber consumption and cardiovascular risk
| Evidence | Grade |
|---|---|
| Consumption of 4–5 portions of fruit and vegetables a day reduces overall and cardiovascular mortality35,57 | A |
| The beneficial effect of fruit and vegetables is dose dependent and is more evident in stroke than CHD35,57 | B |
| Consumption of 2–4 servings of boiled or baked potatoes a week, with no added salt, does not increase cardiovascular risk58,60 | B |
Recommendations
Based on existing data, nutritionists and scientists unanimously agree that fruit and vegetables (including leafy vegetables) are necessary components of any healthy diet due to their broad spectrum of benefits, including reduced rates of CVD and cause-specific mortality. Fortunately, these foods are common ingredients in traditional Spanish cuisine and, given that their benefit is dose dependent, it is recommended that at least five portions of fruit and vegetables are eaten every day. Intake must be varied, with these foods added to both raw and cooked dishes, and it is important to avoid dishes to which sugars have been added during culinary or industrial preparation. With regards to tubers, moderate consumption of 2–4 servings a week is recommended, preferably roasted or boiled. Consumption of commercially processed potatoes, especially French fries or chips with added salt, must be limited.
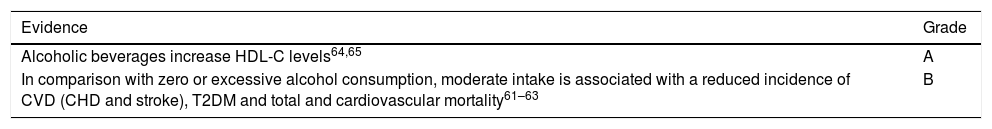
Alcoholic beveragesAlcoholic beverages are any drinks that contain ethanol (ethyl alcohol). According to their preparation, such beverages are divided into those produced by fermentation, such as wine, beer or cider, whose alcoholic content is not more than 15°, and those obtained by distillation, such as spirits (whisky, cognac, gin, vodka or rum) and fruit, herb or spice-flavoured liqueurs (alcohol between 20 and 60°). Numerous epidemiological studies indicate that moderate alcohol consumption reduces total and especially cardiovascular mortality61 plus the incidence of cardiovascular complications such as myocardial infarction, stroke and peripheral artery disease.62 There is also epidemiological evidence showing that moderate alcohol consumption reduces the risk of T2DM.63 Various meta-analyses of cohort studies have observed that maximum is achieved when intake is around 20g of ethanol a day, with approximately a 20% CVD risk reduction. To date, no randomised clinical trials have been conducted to assess the effects of moderate alcohol intake on endpoints such as mortality or incidence of major cardiovascular complications. However, numerous randomised interventional trials have analysed the effects of moderate alcohol consumption and different alcoholic beverages on vascular risk factors.64
Although many studies, including two systematic reviews, have indicated that the type of alcoholic beverage is not a determining factor since they attribute the protective effect of these beverages to their ethanol content, more recent meta-analyses have concluded that the protective effect of fermented beverages (wine and beer) is greater than that of spirits and liqueurs. In this context, numerous clinical trials have analysed the short-term effects of different types of beverages on cardiovascular risk factors.64,65 All have concluded that ethanol significantly increases HDL-C, improves glucose metabolism and reduces fibrinogen, but fermented beverages seem to have a greater effect on atherosclerosis-related oxidative stress and inflammatory parameters due to their higher polyphenol content. Consumption of alcohol-free wine and beer also has a protective effect on reducing blood pressure and increasing endothelial cells and circulating progenitor cells, which are involved in regeneration of the vascular endothelium. It must be noted that only one randomised clinical trial conducted in Israel has assessed the effect of long-term, moderate wine intake on cardiovascular risk factors.66 In this study, three groups of well-controlled diabetics were randomly assigned to receive 150ml of red wine, 150ml of white wine or 150ml of water daily for 2years. Those participants who received red wine experienced increases in HDL-C and apoA1 levels and both groups that received wine showed greater insulin sensitivity, but only when they were slow alcohol metabolisers.
Levels of evidence for moderate alcohol consumption and cardiovascular risk
Recommendations
Alcohol must always be consumed with meals and as part of a healthy diet, such as the Mediterranean diet. Recommended amounts are also different for men and women since women are more sensitive to the effects of alcohol. Optimum consumption would be 2–3 glasses a day for men (maximum 30g alcohol a day) and 1–2 glasses a day for women (15g a day). Men over the age of 65 should also not drink more than 20g of alcohol a day.
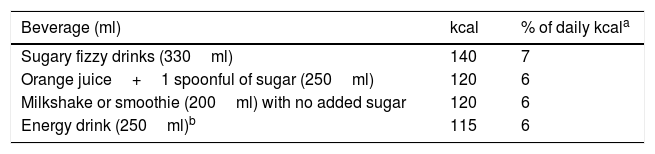
Sugar-sweetened beveragesThe amount of simple carbohydrates (sugars: sucrose, glucose, fructose and lactose) consumed as part of the Western diet (both visible and invisible) tends to be higher than the recommended amount (<10% of daily energy intake, which is equivalent to approximately 25g for men and 20g for women).67 Unlike fats, these nutrients have low satiation and high palatability, promoting passive and continuous overconsumption. They are abundant components of modern-day diets since they are found in multiple products, ranging from sauces to dairy products and cereal-based foods, among others. They are especially common in drinks, particularly artificial fruit juices and sugary soft drinks (Table 3). It is important to remember that health issues attributable to sugar refer to those caused by artificial addition of sugar to foods and not to any sugars naturally found in food. In the latter case, sugar is accompanied by healthy nutrients and biocomponents that balance out the potential harmful effect caused by calorie intake, which could be linked to being overweight and obese.
There is increased concern over the presence of these sources of empty calories in everyday food items and it is estimated that their consumption was associated with 184,000 deaths worldwide in 2010 due to promoting obesity and related diseases, such as CVD, CHD and cancer.68 The results of reviews and meta-analyses consistently indicate that sugar-sweetened beverages increase cardiometabolic risk, including visceral obesity and metabolic syndrome and components thereof, such as glucose intolerance and T2DM, HTN and atherogenic dyslipidaemia.69 A recent meta-analysis of seven prospective studies with 308,420 participants indicated an increased risk of stroke and myocardial infarction with increased consumption of sugar-sweetened beverages.70
Substitution of sugar-sweetened beverages with healthier alternatives among the general population is an enormous challenge. More than 50% of Americans consume at least one sugar-sweetened beverage a day, with 178 excess calories/day in men and 118 in women. Repetitive consumption of such beverages creates a habit which makes it hard to return to drinking water as your main source of fluids since you become used to the additional pleasure of the flavour of sugar-sweetened beverages. In practice, and whenever it is hard for a patient to replace such beverages with water, the swap can be made easier by drinking sweetened drinks containing low-calorie sweeteners. One randomised clinical trial in children specifically comparing daily intake of one sugar-sweetened beverage (104kcal) with a similar beverage containing low-calorie sweeteners showed that these drinks led to less weight gain and adiposity at 18months.71 Although the effects of such low-calorie beverages on health are not well known, it is thought that their use may help reduce calorie intake due to sugar-sweetened beverages. In the USA, proposals have been drafted to include warnings on the bottles of products with a high sugar content regarding potential harmful effects, similar to those found on tobacco packaging, although such proposals have not yet been introduced. In this context, improved education may be the best option for reducing consumption of sugar-sweetened beverages, although increased taxes on such beverages is also a good idea.
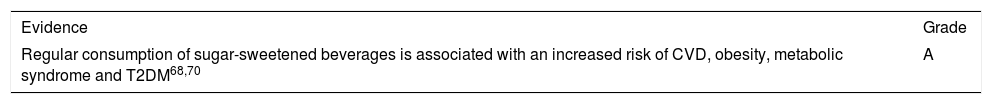
Levels of evidence for the relationship between sugar-sweetened beverages and cardiovascular risk
| Evidence | Grade |
|---|---|
| Regular consumption of sugar-sweetened beverages is associated with an increased risk of CVD, obesity, metabolic syndrome and T2DM68,70 | A |
Recommendations
Sugar-sweetened beverages form part of many individuals’ everyday diet worldwide and may account for up to 20% of their daily calorie intake. Replacing this type of beverage with water is a very important step towards reducing energy intake and the risk of obesity, T2DM and related diseases. If a patient does not accept this advice, beverages with artificial sweeteners may be recommended as so far there is no first-level scientific evidence regarding their harmfulness.
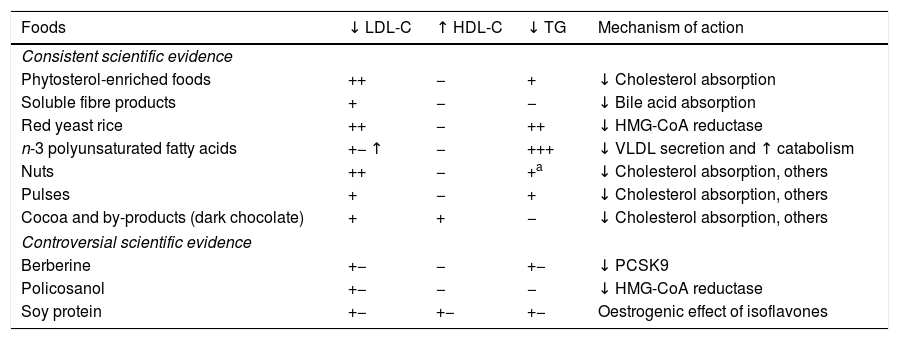
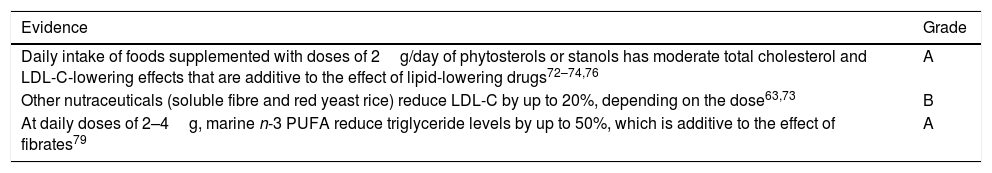
Functional foods and nutraceuticals in cardiovascular risk preventionIn the presence of dyslipidaemia, in addition to recommending a heart-healthy diet, it is important to consider introducing functional foods or nutraceuticals with lipid-lowering effects. These are foods that contain a component (nutritive or non-nutritive) that has a measurable, selective effect on one or more biological functions while providing a health benefit beyond basic nutrition. The composition of such foods, which are often processed, is changed by removing (e.g. skimmed milk), adding (e.g. milk with phytosterols) or substituting (e.g. milk with dairy fat replaced with vegetable fat) a component. However, it is clear that we can also call natural foods with cholesterol-lowering properties, such as nuts, pulses, whole grains and dark chocolate (see corresponding sections), “functional foods”. With regards to nutraceuticals marketed as lipid-lowering products, there is abundant scientific evidence on the efficacy and safety of some of these products. However, other products have controversial effects and require further study, as indicated in the 2016 European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) Guidelines for the Management of Dyslipidaemias72 and recent reviews.73,74
Functional foods with recognised beneficial effectsNutraceuticals that have proven to be effective in controlling hypercholesterolaemia include plant sterols or phytosterols, soluble fibre and red yeast rice (monacolin). Marine n-3 PUFA also have triglyceride-lowering effects at pharmacological doses. It must be noted that these four functional foods have cardiovascular health claims approved both by the US Food and Drug Administration and the European Food Safety Authority.
Plant sterols. These are natural compounds that are extracted from plant matter and added to foods, especially dairy products or spreadable fats, and are typical examples of a nutraceutical. Phytosterols play a structural role in the membranes of plant cells, equivalent to that of cholesterol in animal cells, and are most abundant in seeds and seed-based oils. Their chemical structure differs from that of cholesterol due to the presence of side chains. Stanols, which are less abundant in nature than sterols, are saturated sterols, i.e. they have no double bonds in the sterol ring. These structural modifications mean that these molecules are more hydrophobic than cholesterol and therefore are absorbed less from the intestine and interfere with cholesterol absorption in the lumen. Reduced absorption means that less cholesterol reaches the liver, which has two compensatory effects: increased cholesterol synthesis and increased LDL receptor expression. The net effect is lower serum LDL-C levels.72–75 There is abundant scientific evidence from controlled clinical trials showing that consumption of 1.5–4g/day of phytosterols/stanols reduces cholesterolaemia by 5–15%, with a mean reduction of 10%.76 This occurs, even if the diet is low in cholesterol, because bile transports large amounts of cholesterol to the intestines and reabsorption is blocked by phytosterols. The cholesterol-lowering effect is dose dependent up to 4–5g/day but the recommended dose tends to be 2g/day. Efficacy is associated with baseline cholesterolaemia so cholesterol is reduced more when starting levels are higher. Triglyceride levels are also lowered modestly if they are high. The cholesterol-lowering efficacy, which is similar for sterols and stanols, has been proven in children, adults and the elderly, in patients with moderate or severe hypercholesterolaemia, in patients with and without diabetes and in patients with and without CVD. Numerous studies have shown the efficacy of phytosterols in patients treated with statins, in whom the LDL-lowering effect is additive. Although fewer studies are available, phytosterols also appear to be effective in combined therapies with ezetimibe or fibrates.75 Administration of sterols or stanols at the indicated doses is harmless. Since these compounds are poorly absorbed and are rapidly excreted into bile, the risk of accumulation in the body is very low. Absorption of fat-soluble vitamins and carotenoids from the intestines requires micellar solubilisation and transport, like cholesterol, and, therefore, there is a potential sterol/stanol interference effect. A recent meta-analysis of 41 clinical trials observed a reduction in plasma concentrations of carotenes, lycopene and other fat-soluble vitamins, while remaining within normal ranges, and there are therefore no negative clinical implications.77 Since beta-carotene is a precursor for vitamin A, in situations requiring higher vitamin A intake, such as childhood, consumption of natural sources of beta-carotene, such as carotenoid-rich fruit and vegetables, is advised.
Soluble fibre. Dietary fibre is the portion of plant-derived foods that cannot broken down by the human gut. Almost by definition, a fibre-rich diet is healthy due to containing abundant plant-derived foods. There are two types of dietary fibre: water-soluble and insoluble fibre, although only the first is metabolically active, especially viscous soluble fibre. This is due to the fact that it forms a gel in water, which increases the viscosity of the meal bolus in the intestine, delaying absorption of nutrients, including cholesterol, while also fixing bile acids, thereby increasing catabolism of cholesterol in a similar way to anion-exchange resins. This explains their cholesterol-lowering effect, which has been recognised for several decades. Fermentation of fibre in the large intestine also results in the formation of short-chain fatty acids, with a trophic action on colonic mucosa. There are several products that are high in soluble fibre that have been marketed for their metabolic effects and that have proven to be effective in lowering cholesterol levels in scientific studies. These include β-glucan (from oats or barley), guar gum (guar bean extract), pectin (from fruit), glucomannan (Amorphophallus konjac plant extract), psyllium (Plantago ovata extract) and hydroxypropyl methylcellulose (modified cellulose fibre). Depending on the product, daily doses range from 3 to 30g and reduce LDL-C by 10–15%, with no changes in triglycerides or HDL-C. In many cases, soluble fibre intake also has beneficial effects on glycaemic control and body weight.75
Red yeast rice (monacolin). Rice fermented with red Monascus purpureus yeast has been used for years as a food colouring and as a traditional remedy in Chinese medicine. The main metabolite found in red yeast rice is monacolin K, which is chemically similar to lovastatin and capable of reducing total cholesterol and LDL-C concentrations by inhibiting HMG-CoA reductase activity. According to a meta-analysis of 13 clinical trials, daily administration of red yeast rice products containing 10mg of monacolin significantly reduces LDL-C (0.87mmol/l mean) and triglycerides (0.23mmol/l) but has no effect on HDL-C.78 The monacolin content is highly variable in different products, which are considered drugs in the USA and supplements in the European Union, and, given that the active ingredient is a statin, red yeast rice can cause similar muscle symptoms in statin-intolerant individuals.73
n-3 polyunsaturated fatty acids At pharmacological doses of 2–4g/day, marine n-3 PUFA are as effective as fibrates in lowering triglycerides and have no side effects, especially in the case of pharmacological-grade fish oil products, which are free from heavy metal-type fish oil pollutants. Like fibrates, n-3 PUFA are PPAR-α ligands that reduce synthesis and secretion of very-low-density lipoprotein (VLDL) by the liver while accelerating VLDL catabolism by stimulating lipoprotein lipase expression. However, reduced fatty acid synthesis involves independent mechanisms, showing that their triglyceride-lowering effect is complementary to that of fibrates. The efficacy of n-3 PUFA in the reduction of triglyceride levels has been demonstrated in monotherapy and combined therapy with statins. In cases of severe hypertriglyceridaemia (HTG) due to chylomicronaemia syndrome, the effect of n-3 PUFA is added to the effect of fibrates, achieving additional reductions in triglycerides by up to 50% and minimising the risk of pancreatitis.79 Reductions in triglyceride levels due to n-3 PUFA have been shown to be associated with mild or moderate increases in LDL-C, although this is of limited importance since such increases involve large, less atherogenic LDL particles. Also, in cases of HTG, it is better to use non-HDL cholesterol to measure atherogenic lipoproteins.
Functional foods with debatable efficacyThis section looks at a series of products with potential lipid-lowering activity that have not yet been studied in detail or that have been studied but with confusing results. One such product is berberine, an isoquinoline alkaloid extracted from plants and used in traditional Chinese medicine. In experimental studies, high doses of berberine reduce cholesterolaemia by reducing PCSK9 expression and lowering circulating PCSK9 levels. Clinical trials and meta-analyses of such trials have been conducted in China, with heterogeneous results and 20–25% reductions in LDL and 13–30% reductions in triglycerides. A beneficial effect on diabetes and non-alcoholic steatohepatitis has also been described. Studies with a high level of scientific rigour are required to determine whether berberine is in fact useful for controlling dyslipidaemia. Policosanol is a natural mixture of long-chain aliphatic alcohols extracted primarily from sugar cane that has a mild inhibitory effect on HMG-CoA reductase. Its cholesterol-lowering effect has been reported in clinical trials conducted in Cuba, but these results have not been reproduced in good-quality clinical trials conducted elsewhere and their efficacy in treating dyslipidaemia is therefore debatable. Soy protein can be used to replace animal protein and may therefore reduce LDL-C concentrations. Various meta-analyses examining the effects of soy protein or soy isoflavone (characteristic soy phytoestrogens) intake on lipid profile have been conducted. Most of these analyses have observed a slight effect at doses of 25–50g/day, with reduced triglyceride and increased HDL-C levels in some studies. The mechanism of action may be due to the oestrogenic effect of isoflavones. Nevertheless, the reduction in lipid levels is mainly attributable to the replacement of animal protein with plant protein and the resulting reduction in SFA and cholesterol intake. In addition to the functional foods mentioned above, as already indicated in the corresponding sections, regular consumption of a handful of nuts, a portion of pulses or a portion of dark chocolate, apart from being associated with a lower incidence of CVD, has a consistent LDL-lowering effect and these are therefore clearly natural functional foods for the treatment of dyslipidaemias and cardiovascular risk. Lipid-modifying properties of other types of food, such as green tea, garlic concentrate, artichoke leaf extract, algae such as spirulina, hawthorn berries and resveratrol, have also been described.73,74 However, there are contradictory results or insufficient information for most of these products.
Supplement and nutraceutical combination productsSeveral well-controlled clinical trials examining the lipid effects of a supplement containing red yeast rice (200mg, corresponding to 3mg monacolin), policosanol (10mg), berberine (500mg) and folic acid (0.2mg), the antioxidant astaxanthin (0.5mg) and coenzyme Q10 (2mg), have been conducted. A recent review of these trials concluded that daily administration of a dose of this supplement is well tolerated, reduces LDL-C by 15–30% and has no effect on triglycerides and HDL-C.75 This cholesterol-lowering effect is similar to that of low doses of statins and somewhat higher than that of ezetimibe. An improvement in insulin sensitivity has also been described. Since the nutraceuticals sector is an important expanding market, clinical results for other combinations have also been described and published, but such data are still preliminary. This issue has recently been reviewed in depth.73
Portfolio dietSeveral foods with cholesterol-lowering properties can be used in combination in this diet designed for therapeutic purposes. Recognition that isolated consumption of generous portions of seeds reduces cholesterol by 5% or more, functional foods with phytosterols lower cholesterol by a further 10% and changing from a Western diet to a healthy low-SFA and cholesterol diet can help achieve similar reductions in cholesterol suggests that combining these foods may reduce LDL-C levels by 30%, which is similar to reductions obtained with first-generation statins. This concept was tested in controlled metabolic studies in which participants received all foods and the given combination of foods (referred to as “portfolio” by investigators) was compared with 20mg of lovastatin following a crossover design with 4-week periods. During the diet phase, participants followed a strict vegetarian diet with the addition of soy protein (pulses), grains and vegetables with a high soluble fibre content, almonds and margarine with added phytosterols, achieving a mean LDL reduction of 30%, which is similar to the 33% reduction achieved with the statin.80
Levels of evidence for nutraceuticals and cardiovascular risk
| Evidence | Grade |
|---|---|
| Daily intake of foods supplemented with doses of 2g/day of phytosterols or stanols has moderate total cholesterol and LDL-C-lowering effects that are additive to the effect of lipid-lowering drugs72–74,76 | A |
| Other nutraceuticals (soluble fibre and red yeast rice) reduce LDL-C by up to 20%, depending on the dose63,73 | B |
| At daily doses of 2–4g, marine n-3 PUFA reduce triglyceride levels by up to 50%, which is additive to the effect of fibrates79 | A |
Recommendations
Together with appropriate lifestyle changes, the use of nutraceuticals with known efficacy and safety, shown by way of cholesterol reductions (Table 4), is advised both for individuals with high cholesterol levels who have a low overall cardiovascular risk and do not need pharmacological treatment, and for individuals with high cardiovascular risk who are drug intolerant or who, after receiving statin treatment, have not achieved therapeutic LDL-C target levels. The fact that there is a lack of efficacy studies on clinical events with nutraceuticals, with the notable exception of nuts supplementing a Mediterranean diet in the PREDIMED study,1 must be taken into account. As with the portfolio diet, the use of several lipid-modifying nutraceuticals may help lower cholesterol levels to levels similar to those achieved with low doses of statins. However, n-3 PUFA at doses of 2–4g/day are a highly effective and harmless alternative to fibrates for reducing triglyceride levels, either as monotherapy in cases of isolated HTG or in combination with statins in cases of combined hyperlipidaemia. Fibrates and n-3 PUFA also have complementary effects and their combined use is therefore very useful in the treatment of severe HTG. To conclude, although nutraceuticals do not replace the use of lipid-lowering drugs, they can be added to therapies to increase the number of patients with well-controlled lipid profiles. They also help reduce drug doses and minimise the likelihood of adverse effects. They may be especially beneficial for patients with moderately high cholesterol levels and a low overall risk who do not wish to take drugs or who have had side effects with treatment.
Functional foods with effects on lipid profile. Effects and mechanisms of action.
| Foods | ↓ LDL-C | ↑ HDL-C | ↓ TG | Mechanism of action |
|---|---|---|---|---|
| Consistent scientific evidence | ||||
| Phytosterol-enriched foods | ++ | − | + | ↓ Cholesterol absorption |
| Soluble fibre products | + | − | − | ↓ Bile acid absorption |
| Red yeast rice | ++ | − | ++ | ↓ HMG-CoA reductase |
| n-3 polyunsaturated fatty acids | +− ↑ | − | +++ | ↓ VLDL secretion and ↑ catabolism |
| Nuts | ++ | − | +a | ↓ Cholesterol absorption, others |
| Pulses | + | − | + | ↓ Cholesterol absorption, others |
| Cocoa and by-products (dark chocolate) | + | + | − | ↓ Cholesterol absorption, others |
| Controversial scientific evidence | ||||
| Berberine | +− | − | +− | ↓ PCSK9 |
| Policosanol | +− | − | − | ↓ HMG-CoA reductase |
| Soy protein | +− | +− | +− | Oestrogenic effect of isoflavones |
Sodium is an essential mineral that plays an important role in regulating the osmolarity of most extracellular fluids and is vital for cellular homeostasis. Like other minerals, such as calcium, vitamin D and hormones like thyroxine, sodium has a J-shaped curve relative to its physiological function and therefore both sodium deficiency and excess sodium have detrimental effects on cell physiology. Numerous epidemiological studies have shown a direct association between excess salt (sodium) intake and the development of negative health consequences, including HTN, kidney disease, obesity and cardiovascular morbidity and mortality. Likewise, excess sodium intake during adolescence has been shown to be associated with a significant increase in blood pressure in men between the ages of 18 and 25, but not in women, suggesting that this effect may be sex dependent. According to evidence obtained from systematic reviews on the cardiovascular benefits of reducing salt intake, since 2013, the World Health Organization (WHO) has recommended keeping sodium intake to less than 2g/day (equivalent to approximately 5g of salt) for adults, with lower figures for children.81 Nevertheless, despite recommendations made by different organisations and scientific societies to reduce dietary salt intake, such intake remains high, with mean levels of 9g/day, making it one of the main risk factors for HTN and CVD.
It is currently well established that there is a direct, linear relationship between high sodium intake and blood pressure, especially within high ranges. A recent systematic review of 185 clinical trials comparing high-salt and low-salt diets concluded with a high level of evidence that reduction of salt intake is a very effective measure to reduce blood pressure, especially among the hypertensive population.82 However, the impact of low sodium intake on cardiovascular mortality is still a controversial topic.83 As already mentioned, some authors have observed an increase in cardiovascular risk with a sodium intake of 2.3g/day or lower, thereby suggesting a U-shaped or J-shaped curve between salt intake and cardiovascular risk. Possible pathophysiological mechanisms responsible for potential harmful effects of excess salt reduction include activation of the renin-angiotensin-aldosterone system and a higher predisposition to insulin resistance.83 However, recent results of the Trial of Hypertension Prevention (TOHP) cohort study, analysing the relationship between sodium intake and all-cause mortality over 20years in 2974 participants, confirm an increased risk of mortality with high salt intake and a direct, linear relationship with total mortality, even at the lowest levels of sodium intake.84 Moreover, a recent, large epidemiological study in the United States suggests that excess sodium intake is the leading risk factor responsible for mortality due to cardiometabolic diseases (CHD, stroke and T2DM) among 10 dietary factors.85 Since there is insufficient evidence to be able to clearly state whether reducing dietary sodium intake to less than 2.3g/day is detrimental or not, the most sound advice would be to reduce intake to between 2.5 and 4g/day as this is the healthiest range in which variations in sodium intake are not associated with higher mortality.81
Finally, another relevant issue is individual changes in blood pressure with increased salt intake, which may increase greatly in some individuals and very little in others. This heterogeneity means individuals can be classified as salt sensitive or salt resistant, respectively. This suggests that salt-sensitive individuals have a hypersensitive renin-angiotensin system so that maintained salt intake induces renal vasoconstriction and increased tubular sodium reabsorption, causing increases in blood pressure. Salt sensitivity progressively increases with age, is more common in hypertensive individuals and is more prevalent in blacks (74%). It is suggested that salt sensitivity has a genetic cause, but there are insufficient data to attribute such sensitivity to variations in known genes. Knowing whether an individual is salt sensitive or salt resistant is clinically relevant since salt sensitivity is a powerful, independent risk factor for cardiovascular morbidity and mortality, like HTN.86 Diagnosis requires repeated measurements of blood pressure response after periods of salt overload and salt restriction. However, the best public health strategy is to reduce population-wide salt intake.
Levels of evidence for salt consumption and cardiovascular risk
Recommendations
A low-salt diet (<5g/day) should be recommended population wide, especially for hypertensive patients and their relatives. Remember that the sodium content of food must be multiplied by 2.5 to calculate the amount of total salt. Particularly effective measures for reducing salt intake are to limit consumption of foods with a high salt content, such as precooked, tinned and salted foods, cold meats and fizzy drinks. An alternative to salt is to use lemon juice, herbs or garlic. It should also be remembered that, for many people, bread is the main dietary source of sodium and therefore low-salt varieties should be recommended. It is also useful to identify salt-sensitive patients (changes in blood pressure after diets with and without salt) due to their inherent high risk of CVD.
Food processingProcessing is the process by which raw foods are made suitable for consumption or storage using procedures to improve their palatability, nutrient value, preservation and safety. Such processing is common for most types of food consumed today and includes any action that starts with food preparation and finishes with the food being cooked. On cutting or chopping foods, tissues are damaged and enzymes and substrates that are normally separated by membranes are brought into contact, inducing oxidation reactions, such as browning of many types of fruit and vegetables, especially apples, mushrooms, aubergines, etc. It also promotes glucosinolate breakdown reactions which generate isothiocyanates, compounds with anti-tumour properties. On cutting foods, tissues are also exposed to oxygen in the air, which promotes lipid oxidation and rancidity due to spontaneous reactions and loss of moisture.87 There are many food preparation and preservation methods available, although the most common are the cold storage or heating and dehydration. Other methods are also used to greater or lesser degrees, such as fermentation, salting, curing, pickling, smoking or preservation in high sugar concentrations. The type of packaging used can also affect the quality of the food. The most common forms of food processing are discussed below.
Use of cold or heatProcedures that use cold to preserve foods include refrigeration, freezing and industrial methods such as deep freezing. These are the most effective methods of food preservation since lowering the temperature of a food decreases the rate of deterioration by delaying microbial growth or inactivating enzymes responsible for deterioration. Nutrient losses are limited and depend on factors such as temperature reached, duration and subsequent storage, with the advantage that the organoleptic properties of food are not really affected. After thawing, there is a significant loss in vitamin C content. Some industrial procedures, such as freeze drying, preserve nutritional properties, even those of vitamins, with minimal impact. One of the major drawbacks of such procedures is that, after freezing, fat tends to become rancid quicker. Heating, however, denatures proteins, destroying the enzymatic and metabolic activity of microorganisms, although this greatly changes the food, which may paradoxically be beneficial or harmful for nutrient value. Moist-heat, frying or dry-heat treatments can be used. Moist-heat methods include braising, boiling, steaming, pressure steaming and poaching. Frying methods include sautéing, pan-frying and deep-fat frying, while roasting, grilling and baking are examples of dry-heat methods. The aforementioned technologies can also be combined, such as in mixed cooking, which includes stews, casseroles and barbecues. However, more innovative and popular techniques, such as microwaving, ultra-high-temperature (UHT) processing and pasteurisation, allow faster, hotter heating, with less changes in nutrient value. In terms of the more traditional systems, cooking in water causes a loss of vitamins, minerals and other water-soluble bioactive compounds, although steaming causes much less loss than boiling. In some cases, the application of heat results in beneficial changes to food. Examples of this include cooking eggs, which destroys avidin, a protein that prevents absorption of biotin; cooking tomatoes, which makes lycopene more bioavailable; and cooking pulses, which helps remove potentially toxic components, such as lectins. Cooking denatures proteins and causes a loss of essential amino acids. With frying or dry-heat techniques, the temperatures reached are higher than those reached when cooking in water, which results in a greater loss of some heat-sensitive nutrients, such as thiamine. High temperatures, such as those reached when frying, cause a loss of beneficial compounds (e.g. antioxidants) or generate harmful products (e.g. carcinogenic acrylamide), although with a good frying technique, a protective skin is produced on the surface of the food that decreases deterioration and retains a higher proportion of nutrients. Nevertheless, this process is complex since it also causes the so-called Maillard reaction, whereby proteins and carbohydrates combine to give food its characteristic golden-brown colour, and can lead to the generation of antioxidant compounds, such as reductones. The use of oils for frying promotes their breakdown, which is greater in the case of oils that are less resistant to oxidation. Therefore, the worst oils for frying are PUFA-rich, seed-based oils which are oxidised by oxygen radicals, with the generation of hydroperoxides and other pro-inflammatory and atherogenic molecules.87 Olive oil, however, is resistant to frying due to both its low PUFA content and its high antioxidant content, in the case of extra virgin olive oils.8 Frying also progressively destroys omega-3 PUFA, which are characteristic of fish and have multiple health benefits.
FermentationYeasts, fungi or specific bacteria are used in fermentation to give the food the desired flavour and texture, as is the case with leavened bread and alcoholic beverages. Another type of fermentation is carried out by bacteria that produce lactic acid, as occurs with yoghurt, gherkins and some meat products, such as cold meats. This increases the shelf life and safety of foods, modifying their texture and flavour. It must be noted that fermentation can enhance the nutrient value of foods since microorganisms produce essential amino acids, fatty acids and vitamins that are absorbed. Microbial activity can also reduce the content of undesirable components, as occurs with lactic acid bacteria that ferment bread, and eliminate phytates, which improves the bioavailability of minerals such as calcium, iron, zinc and magnesium. Nevertheless, some types of protein fermentation can generate toxic compounds, such as biogenic amines or nitrosamines.
Other proceduresSalting involves adding salt to reduce the water activity of foods, preventing microbial growth. It is mainly used to preserve meat and fish, with examples including salted fish and salt-cured meat. Similar preservation effects can be achieved by adding sugar or by altering pH with the addition of acids, such as vinegar in pickles. In the case of pickles, salting is combined with fermentation and the addition of vinegar. This method is used primarily to preserve vegetables (e.g. cauliflower, cucumber, pepper, onion and olives) and fish (e.g. herring). Curing is mainly used for fish and meat and involves adding combinations of salt, sugar and sometimes nitrates or nitrites to foods. In addition to preventing bacterial growth, this gives the meat an attractive pink colour, as can be observed with ham. It must be noted that regular and excessive consumption of these foods is not recommended because nitrogen compounds may generate carcinogenic nitrosamines. Smoking is also sometimes used when curing foods.
Backed by a large number of references, the WHO issued a statement in October 2015 on the consumption of red meat and processed meat and the risk of cancer.88 In its statement it defined red meat as all types of mammalian muscle meat, such as beef, veal, pork, lamb, horse and goat, while it considered processed meat to be meat that has been transformed through salting, curing, fermentation, smoking or other processes to enhance flavour or improve preservation. Most processed meats contain pork or beef, but processed meats may also contain other red meats, poultry, offal or meat by-products such as blood. The relationship between red meat intake and the risk of cancer is not very clear, but their preparation at high temperatures encourages the production of carcinogenic products, such as heterocyclic aromatic amines and, in the case of smoking, polycyclic aromatic hydrocarbons. The relationship between processed meats and the risk of bowel and stomach cancer is much clearer because their preparation encourages the generation of such products.
Some processing techniques may increase the nutrient value of foods. This is the case of plastification of durum wheat for production of pasta, in which a protective layer is generated that delays hydration and starch gelatinisation during cooking, reducing the glycaemic index of the food. With regards to packaging, its function is to prevent oxidation and loss of nutrients and slow down maturing processes so that the food can be preserved for longer, especially at low O2 or high CO2 concentrations. Packaging is increasingly involving the use of food additives, which are natural or artificial substances added for a specific technical purpose, such as preservatives, stabilisers, anti-caking agents and packaging gases. These products are not ingredients and there is not always enough information about their long-term effect on health. To summarise, food processing involves the addition of components or the generation of components that may increase cardiovascular risk.89
Levels of evidence for processed foods and cardiovascular risk
| Evidence | Grade |
|---|---|
| Processing removes beneficial nutrients from food, especially when processed at high temperatures87 | A |
| Processing promotes the development of obesity and increases cardiovascular risk factors89 | B |
| Frying with olive oil is better than frying with seed-based oils due to both its low PUFA content and its high antioxidant content, in the case of extra virgin olive oils8 | A |
Recommendations
Food processing is becoming more widely used. There are certain procedures that help maintain the nutrient value of foods, while others promote food deterioration and generate harmful products. It is therefore best to choose fresh or minimally processed frozen foods, avoiding the consumption of foods that have been subjected to high temperatures and especially processed meats. However, foods containing added salt, nitrates, sugars and fats should not be consumed because there is a high risk that these may be partially hydrogenated and rich in TFA. Olive oil, and preferably virgin olive oil, should always be used for frying instead of seed-based oils as these are denatured with heat stress, resulting in potentially harmful products.
Healthy eating and lifestyle modelsMediterranean dietMost clinical trials comparing diet with health have investigated the effects of macro/micronutrients and, less frequently, the effects of whole foods. This spurs debates surrounding the interpretation of results because the diet is not based on isolated nutrients or foods but on complex mixtures of ingredients. However, multiple personal and cultural factors condition each person to have their own eating habits. Nevertheless, populations that live in the same cultural and geographical environment are influenced by circumstances that homogenise their preference for certain foods based on the availability of foods. Therefore, each geographical environment has traditionally formed a reasonably common dietary pattern that depends greatly on the current availability of any type of product obtained from remote places. In our environment, the main dietary pattern has been the Mediterranean diet, characterised by abundant vegetables, fruit, pulses and nuts, moderate amounts of fish, poultry, fermented dairy products (yoghurt and cheese) and wine (with meals), and little meat and meat by-products, processed foods in general, sweets and sugar-sweetened beverages. There is plenty of evidence showing the health benefits of this diet, especially with regards to CVD prevention, with evidence obtained from observational and interventional clinical trials. A recent review of evidence from 13 meta-analyses of observational trials and 16 meta-analyses of randomised clinical trials, including almost 13 million participants, robustly shows, with limited heterogeneity between studies, that a greater adherence to the Mediterranean diet reduces overall mortality, CVD, coronary heart disease, myocardial infarction, overall incidence of cancer, neurodegenerative diseases and diabetes.90 Of all the trials considered, the PREDIMED study was probably the one of the highest quality, and which is of particular value for the Spanish population as it was conducted entirely in Spain.1 This trial showed that a Mediterranean diet, supplemented with extra virgin olive oil or nuts, compared with recommendations to reduce all types of dietary fat, reduced the incidence of CVD by around 30% after 5 years of follow-up. First-level evidence provided by the PREDIMED study has been converted into recommendations by various societies, such as the AHA, American College of Cardiology (ACC) and European Society of Cardiology (ESC), which consider the Mediterranean diet to be a healthy dietary pattern for cardiovascular prevention, although they also recognise that its favourable effect only has a modest impact on intermediate risk factors.91
Since it is a well known dietary pattern in Spain, the Mediterranean diet is the easiest to promote and recommend among the Spanish population, which makes recommendations by healthcare professionals easier. Nevertheless, its precise definition is not exempt from difficulties, especially in view of cultural differences in different cities and towns along the Mediterranean coast. The person who proposed the most widely accepted definition was Walter Willett,92 an author who identified the Mediterranean dietary pattern from food habits typical of Crete and southern Italy in the 1960s. The success of his proposal includes its pyramid shape, which is both practical and easy to understand. A group of nutritionists from Mediterranean countries reinterpreted this pyramid by adding Mediterranean lifestyle components, such as biodiversity and sustainability of the foods consumed, cooking practices, regular physical exercise, adequate rest and sitting down to eat with family or friends.93 Recently, Davis et al.94 have reviewed existing literature and refined the definition of the main characteristics of the Mediterranean diet, including the number of servings of key foods per day, essential grams of key foods/food groups, and major nutrient and bioactive phytochemical content. The aim is to obtain a common working definition, improving on the different score systems that tend to be based more on foods than on nutrients.
DASH dietThe DASH (Dietary Approaches to Stop Hypertension) diet95 is a dietary plan that emphasises the intake of fruit, vegetables, pulses, whole grains and nuts and reductions in high-SFA foods, such as meats and whole-fat dairy products, and also sweets and sugar-sweetened beverages. This dietary pattern, which is rich in complex carbohydrates, has been shown to be particularly useful for controlling blood pressure, and is even more effective when associated with a reduction in sodium intake.96 In addition to systolic and diastolic blood pressure, DASH-type diets are also associated with a reduction in total and LDL cholesterol, but not triglycerides.97 A recent meta-analysis of prospective studies indicates that high scores with a DASH-type diet are associated with a significant reduction in chronic diseases, including CVD, DM, cancer, neurodegenerative diseases and total mortality.98 Due to their beneficial effects on cardiovascular risk factors, the AHA recommends DASH-type diets and Mediterranean and vegetarian diets to meet the dietary and lifestyle guidelines for cardiovascular prevention.99
Vegan/vegetarian diet100This diet is based on excluding foods of animal origin. There are various vegetarian eating patterns, ranging from vegan diets, which completely exclude all animal products, to lacto-ovo-vegetarian or pescatarian diets, which allow consumption of those foods that give the diets their name. One risk of vegetarian diets, especially the strictest diets, is vitamin B12 deficiency since this vitamin is found in meat, fish or milk, and therefore supplements must be taken on a regular basis. On the other hand, such diets include zero intake of animal fats and cholesterol and may therefore be beneficial for controlling lipid levels, obesity and HTN. They also have a higher fibre content than conventional diets. Various meta-analyses have corroborated that vegetarian/vegan diets can have a protective effect versus all-cause mortality and the incidence of CHD (up to 25%).101 Like the DASH diet and the Mediterranean diet, the AHA also recommends the vegetarian diet for meeting nutritional objectives for cardiovascular disease risk reduction.99
Alternate Healthy Eating IndexThe Alternate Healthy Eating Index (AHEI) was designed to assess adherence to the Dietary Guidelines for Americans. A higher intake of whole grains, vegetables, pulses, fruit and nuts and a moderate intake of total PUFA, n-3 PUFA and alcohol has a positive impact on the score, while red and processed meats, sugars, trans FA and sodium have a negative impact. Compliance was associated with a reduction in chronic disease risk (CVD, DM and cancer) in adult men and women.102 The AHEI therefore distinguished quality within food groups and acknowledged health benefits of unsaturated oils. The recent meta-analysis of observational studies by Schwingshackl and Hoffmann103 concluded that, like DASH-type diets, a high AHEI score was associated with protection from CVD and other chronic diseases and all-cause mortality. The studies strongly predicted chronic disease and risk of CVD.104 This indicates that, as in the case of the Mediterranean diet, improving the quality of the foods we eat reduces chronic disease risk.
Low-fat dietThis diet is based on restricted intake of fats, particularly saturated fats and cholesterol. In comparison with high-fat diets, these high-carbohydrate diets reduce total and LDL cholesterol by 10–20%, but can increase triglyceride levels if they are high in sugars. They are also useful for weight control given that a reduced fat intake leads to reduced calorie intake.103 Low-fat diets have been recommended for many years to prevent CVD, but despite the important outcome expectations of this dietary pattern, recommended especially in the US, one randomised trial of more than 48,000 post-menopausal women showed that it did not reduce the risk of CVD, including stroke and coronary heart disease.105 Today we can conclude that this dietary pattern is questionable and there is therefore no reason to recommend it.
Palaeolithic dietThis is based on the assumption that the ideal diet for humans is the same as that eaten by our Stone-Age ancestors. It is therefore a nutritional plan based on the ancient diet of wild plants and animals, with the consumption of large amounts of protein and fats obtained from foods such as meat or fish, and very few carbohydrates, such as those obtained from dairy products, fruit and vegetables. You should eat when hungry and stop when you are full, with no restrictions. Recent studies have shown a benefit in glycaemic control, especially among diabetic patients given a palaeolithic diet,106 although this alone does not mean it should be recommended as a way to improve cardiovascular risk. Also, it is practically impossible for most of the population to follow this diet.
Levels of evidence for healthy diets and cardiovascular risk
Recommendations
Different healthy diets, including the DASH, Mediterranean and vegetarian diets, have many components in common. They all recommend higher fruit, vegetable, pulse and fish intake with reduced or restricted meat and saturated fat intake. There is strong evidence that plant-based dietary patterns that are low in SFA, cholesterol and sodium and high in fibre, potassium and unsaturated fatty acids are beneficial and reduce expression of cardiovascular risk factors.99,103 Given the Mediterranean nature of our population, our recommendations are based on the Mediterranean diet. However, this diet is also perfectly aligned with the healthy diet proposal created by Harvard University (Healthy Eating Plate), which also offers positive, simple and easy to understand recommendations.107 In summary, any of the models chosen will include:
- 1.
Use of healthy oils, in our case virgin olive oil, for all purposes, which means avoiding trans fats and butter.
- 2.
As high a vegetable intake and as great a variety of vegetables as possible; vegetables should also be sourced locally if possible.
- 3.
Abundant fruit of all colours, also sourced locally, especially as your normal dessert.
- 4.
Beverages should preferably be water, tea or coffee, with no added sugar. Milk (1–2 glasses) and natural fruit juices (1 glass) should be consumed daily; industrial fruit juices and juices containing added sugar should be avoided.
- 5.
Grains and their by-products, such as pasta or bread, should preferably be wholegrain and consumed daily. Although the traditional Mediterranean diet has included refined rice and has also used refined flour to prepare pasta for decades, the ingredients of sofrito (sauce used as a base for many Spanish dishes) offset the glycaemic effect of the refined grains. Pulses should be consumed 2–3days a week and nuts 3days a week.
- 6.
Healthy proteins should be of both plant and animal origin. Healthy plant proteins include whole grains, pulses and nuts. Healthy animal proteins include milk, fish and poultry (with no visible fat), which can be consumed at different intervals, as indicated in the final table of this document. Animal fats and processed products, especially, should be avoided.
- 7.
Physical activity is a key factor of the traditional Mediterranean lifestyle and, therefore, daily activity is recommended, according to each person's age and physical circumstances.
Major advances in scientific knowledge and discoveries over the past decade have resulted in “precision” nutrition.108 This is based on nutrigenomics, which has shown that the human genome is sensitive to the dietary environment; single-nucleotide polymorphisms (SNPs) that interact with diet in patients at high cardiovascular risk (metabolic syndrome, diabetes, ischaemic heart disease, etc.) modify intermediate markers of the disease, such as systemic inflammation, lipid metabolism and glucose parameters, and even the risk of clinical events of CVD.109 In addition, genome-wide association (GWA) studies have played an important role in identifying new, previously unknown genetic variants that are of particular interest in CVD gene expression. Other genetic markers are also being studied, such as copy number variations (CNV) of DNA. Another area of interest that has also seen significant developments over recent years is nutritional epigenetics, which may help explain mechanisms that are not dependent on gene sequence by which nutrients and other environmental factors modify gene expression and disease development. A personalised dietary pattern may therefore delay or even reverse such epigenetic changes and, therefore, modify disease gene expression. Furthermore, in order to increase the consistency of our knowledge, multiple studies are being conducted to find out how nutrients regulate gene expression. These studies are based on transcriptomic, metabolomic, lipidomic and proteomic analyses which, together with the application of bioinformatics techniques, will allow all the necessary information to be entered into large mega-databases in order to design the diet that best suits each person. Finally, it is important to note the potential role of the relationship between alterations in circadian rhythm and CVD. Recent studies suggest that disruption or internal desynchronisation of circadian rhythms may contribute to clinical manifestations such as obesity, dyslipidaemia, HTN, T2DM and CVD. One interesting aspect is that circadian rhythms are modulated by genetic factors. Recent studies on clock gene polymorphisms and their interactions with diet may lead to the development of new chrono-nutrition-based therapies.110 Thus, chronobiological characterisation of the individual may also be useful for designing a suitable diet based on each person's genetic characteristics. Finally, it should be noted that some genetic chips that have been designed to reveal and even predict the genetic component of some diseases and their complications, and potential responses to certain nutrients and dietary patterns based on individual genetic study, are already available, although they do have certain limitations. Therefore, we believe that, although there is still a lot to be learned, precision nutrition is a cutting-edge approach that is already coming to light.
The human body should be viewed as a supraorganism based on the fact that it has a metagenome: its own genome and the genome of its microbiota, all the bacteria that reside on or within the body. The gut microbiota functions collectively as an organ, regulating multiple biological functions.111 Gut flora, however, is regulated very little by genetic factors but is affected by environmental factors, especially diet, which allows potential flora modifications with dietary changes. In this context, a relationship between metabolism of the choline fraction in dietary phosphatidylcholine (lecithin) and CVD has been demonstrated in recent years. This connection may be mediated by the gut microbiota, which uses choline to produce the metabolite trimethylamine (TMA), which the liver transforms into trimethylamine N-oxide (TMAO), a molecule that is considered to be pro-atherogenic, promoting insulin resistance and cholesterol accumulation in macrophages, forming foam cells that accumulate in arterial walls and promote atherosclerosis.112 Moreover, a recent study that included 4007 people has shown that gut microbiota plays an important role in the production of TMAO, linking higher circulating levels of this metabolite with a higher incidence of major cardiovascular events, which is independent of other classic cardiovascular risk factors.113 Likewise, a recent meta-analysis of observational studies concluded that high concentrations of circulating TMAO or its precursors are associated with increased CVD events and mortality after adjusting for other risk factors.114 However, the possibility that this metabolite may be a consequence and not a cause of CVD has recently been questioned.112 Gut microbiota has also been associated with lipid metabolism through different metabolic pathways, including short-chain fatty acids and bile acids, which regulate energy homeostasis through bile acid-activated nuclear receptors FXR (farnesoid X receptor) and TGR5. Finally, there are other mechanisms associated with the production of lipopolysaccharides and peptidoglycans that have been related to reverse cholesterol transport, hyperlipidaemia and vascular inflammation.
Multiple studies have confirmed the paradigm that gut microbiota can be manipulated through diet, with favourable changes associated particularly with fibre intake. In this context, data from recent studies suggest a benefit of restricted L-carnitine intake from foods, basically by limiting the consumption of red meats and meat by-products, since microbial metabolism of L-carnitine also promotes TMAO formation and the association of high serum concentrations of both molecules seems to be associated with CVD.114 This may explain the well-known role of meat and meat by-product consumption as a promoter of cardiovascular risk. In this context, limiting the intake of such foods to decrease circulating levels of TMAO would be an effective strategy for preventing CVD. However, betaine, another TMAO precursor, is found only in vegetables and its consumption is inversely associated with cardiovascular risk, which again questions the atherogenic effect of TMAO.112 Similarly, it has been confirmed that plant-rich diets promote the presence of microorganisms, such as Faecalibacterium prausnitzii, which produce butyrate, a short-chain fatty acid produced by polysaccharide metabolism that has beneficial local (nutrition of colonic mucosa with anti-tumorigenic actions) and systemic (protection from the risk of diabetes, obesity and atherosclerosis) effects. This change in microbiota has also been observed in obese people with a Mediterranean diet. Although this diet contains a high percentage of fat, such fat is unsaturated.115 This suggests that it is the quality and not the quantity of fat that may affect changes in microbiota. The ability of prebiotics, probiotics and faecal transplants to modify microbiota is known. Prebiotics increase the number of bifidobacteria, while probiotics have more extensive effects since, like the Mediterranean diet, they have direct effects or effects due to their ability to functionally stimulate resident flora. Therefore, there are data indicating that diet is able to prevent CVD by modifying gut microbiota, but studies specifically designed for this purpose, which provide clear scientific evidence and allow application in clinical practice, are required.
SummaryIn recent years, the concept of personalised nutrition has become more significant in the health sector. Identifying and promoting optimal diet and lifestyle for each individual based on his/her genetic traits may be fundamental when it comes to preventing and treating chronic diseases, particularly CVD.
Adherence to diet: strategies to improve adherenceThe concept of “adherence” recognises the patient's right to decide whether or not to follow recommendations and involves the patient's active participation in the treatment regimen. Adherence to a plan to modify dietary pattern requires enormous personal effort and good long-term outcomes are rare.116,117 Most people prefer medications to having to make the effort to change their habits and, therefore, any initiative demands sufficient motivation to be able to continue with recommendations in the long term. It is therefore important for people to decide to make lifestyle changes when they are in a positive place, with no symptoms of depression or stress.117
Strategies to improve adherence focus on five key pillars: (a) the patient; (b) the family; (c) the health team involved in the patient's treatment; (d) the healthcare system and the medical team; and (e) the dietary pattern recommended for the patient. Lack of adherence is due to failure of one, several or all of these pillars. Many of the concepts discussed below focus on adherence to drug treatment, but can be used in reference to adherence to diet. Strategies can be categorised as follows116–118:
- 1.
Simplified strategies. The aim of these strategies is to reduce unnecessary changes in the diet and to integrate changes without interfering with everyday activities. For example, efforts must be made to ensure that recommendations take into account tradition in the case of patients from other countries or cultures.
- 2.
Behavioural strategies. The aim of these strategies is to make the individual feel responsible for any changes made. This includes monitoring intake, following up on changes, with positive reinforcement (rewards for achieving goals and not blaming the patient for seeing no improvements), or reminding the patient of his/her next check-up appointment. For many of these initiatives, new technologies that can be downloaded onto smart phones, such as apps, may be useful.118
- 3.
Informative and educational strategies. The aim of these strategies is to encourage the individual to gain more knowledge on his/her risk of disease or on the disease itself, if he/she is already ill, on dietary treatment and on the importance of adherence to such treatment, thereby trying to give the patient more power.
- 4.
Social and family support strategies. The aim of these strategies is to ensure that the subject does not feel “abandoned”, and will include social support (e.g. home help programmes) and the involvement of family or friends (e.g. eating with the family, asking the family to eat the same diet as the individual). In the case of children, it is also necessary to have the school's cooperation, especially that of school canteen staff.
- 5.
Strategies aimed at healthcare professionals and healthcare administrators. The aim of these strategies is to use educational programmes to train healthcare professionals on communication techniques that can improve patient adherence and to encourage the involvement of the healthcare provider system to promote doctor/educator/nutritionist relationships with the individual (e.g. by providing subsequent visits or replacing “missed” visits).
- 6.
Combined strategies. Non-adherence is a complex, multi-factorial issue and therefore strategies must combine various measures simultaneously. A good example of a combined strategy was that used in the PREDIMED study, in which periodic individual and group meetings with dieticians were held along with behavioural sessions, provision of healthy food descriptions, shopping lists, menus and recipes, and gifts of healthy foods, such as extra virgin olive oil and nuts.1 The strategy of providing free food is, without a doubt, the best strategy for achieving adherence.
A Cochrane review of 38 dietary clinical trials published at the end of 2010119 identifies several potentially beneficial interventions for enhancing adherence: telephone follow-up, educational videos, incentivisation contracts with rewards for adherence, feedback using serial dietary surveys completed by the individual, nutritional tools (such as food swap lists or recipes) and combined and multiple interventions, as indicated in the PREDIMED study. The authors conclude that there is a need for further, long-term, good-quality studies using more standardised and validated measures of adherence to identify the interventions that should be used in practice to enhance adherence to dietary advice in the context of a variety of chronic diseases. These types of strategies are justified because studies in different populations, especially in patients with CVD or DM, have shown that greater adherence to healthy dietary changes promotes improvements in quality of life and control of the disease and its risk factors, reducing the number of hospitalisations, cardiovascular events and cardiovascular and all-cause mortality.120,121
Level of evidence for adherence to diet and cardiovascular risk
| Evidence | Grade |
|---|---|
| Improved adherence to diet reduces cardiovascular events and overall and cardiovascular mortality121 | A |
Summary
Adherence to dietary interventions is a complex issue with limited results due to multiple factors, personal or otherwise, that determine their success. Nevertheless, given that correct adherence has been shown to improve quality of life, disease and risk factor control, we must make the effort to achieve adherence among our patients.
Smoking and approaches to treating itIt is currently well established that smoking, even as few as 1–5 cigarettes a day, considerably increases the risk of CVD122 and the risk of other severe pathologies, such as various types of cancer. Therefore, all smokers should be advised to stop smoking since doctor advice alone has been shown to double the spontaneous quit rate, regardless of the patient's stage of quitting. However, such advice may be made more effective by providing self-help materials, specific tips, classes and telephone follow-up. As a practical measure, any patient wishing to stop smoking should receive effective treatment combining psychosocial and pharmacological interventions, with adequate follow-up.
Psychosocial intervention. This type of intervention has several goals: to help develop a plan to quit smoking by setting a quit date; and to give advice for resolving problems, including mechanisms to avoid or replace situations linked to the risk of going back to smoking, thereby preventing problems that are secondary to quitting, such as weight gain or anxiety.123
Pharmacological intervention. This involves recommending tobacco replacement products, such as nicotine, bupropion and varenicline.124 Nicotine use will depend on smoking habits. For moderate smokers, or individuals who smoke their first cigarette more than 30min after waking up, 2mg nicotine gum or the equivalent strength of nicotine patch should be recommended. For heavy smokers, or individuals who smoke their first cigarette within the first 30min of waking up, 4mg nicotine gum or the equivalent strength of nicotine patch should be recommended. Finally, in highly dependent patients, a nicotine nasal spray (2–3mg/h while awake, for 3months) should be prescribed. Given that the safety of nicotine replacement products immediately after a myocardial infarction has not been fully established, it is best to wait until the acute phase of the coronary event has passed before starting at a lower dose. The initial dose of bupropion treatment is one 150mg tablet in the morning for 6days. From day 7, one tablet should be taken in the morning and another 8h later. The individual should stop smoking during the second week of treatment. Side effects tend to be minor, although insomnia and anorexia stand out as the most common. A third drug, varenicline, should be started 1–2 weeks before the set quit date, starting with one 0.5mg tablet a day for 3days followed by 0.5mg twice daily for 4days. From week 2, 1mg must be taken twice daily until the end of treatment. Side effects are minor and include insomnia, nausea, headache and abnormal dreams, which go away on their own over time without having to discontinue treatment.
An important element is smoking cessation follow-up, which must be done every 4–6weeks, with subsequent follow-up at 6months. The purpose of this is to increase success rates, which will be higher with a combination of pharmacological measures and good psychological support. The drugs available have a similar success rate, although most studies suggest better outcomes with varenicline. Success rates tend to be below the proposed targets since, even in the best case scenario, with combined therapies and personalised support programmes, quitting success rates at 6months are no higher than 35%.125
Recommendations
Healthcare staff must always give smokers advice on how to quit smoking, including social and pharmacological intervention, which must be adapted to the patient's smoking habits.
Physical activityThe WHO considers physical activity to be any bodily movement produced by skeletal muscles that requires energy expenditure, with “physical activity” being different from “physical exercise”.126 Exercise is a subcategory of physical activity that is planned, structured, repetitive and purposeful in the sense that the improvement or maintenance of one or more components of physical fitness is the objective. In addition to exercise, physical activity includes other activities which involve bodily movement and are done as part of playing, working, active transportation, household chores or recreational activities.126,127
Regular and maintained physical activity offers protection from the onset of CVD with a dose-response relationship.126–128 However, from a cardiovascular point of view, moderate, regular and enjoyable aerobic activities are recommended for the general population.126,127 Moderate physical activity requires a moderate amount of effort, which noticeably accelerates the heart rate, while vigorous or intense activity requires a large amount of effort and causes rapid breathing and substantial increase in heart rate. There is a long list of potential activities, but the following examples may be recommended: walking, cycling, dancing, swimming, playing golf, gardening, walking the dog, etc. There are also other activities that can be considered exercise in the context of an increasingly sedentary lifestyle, such as walking to work or climbing the stairs. Also, to improve cardiovascular health, it is important to reduce the amount of time spent watching TV or playing video games.126
ObjectivesFor children and young people aged 5–17, physical activity includes play, games, sports, how they travel around, recreational activities, physical education or planned exercise, in the context of family, school and community activities. They should do at least 60min of moderate to vigorous-intensity physical activity daily, although physical activity for more than 60min daily will provide even greater health benefits.126 For adults over the age of 18, physical activity includes recreational or leisure-time activities, how they travel around (e.g. walking or cycling), occupational activities, household chores, play, games, sports or planned exercise, in the context of daily, family and community activities. They should do at least 150min of moderate-intensity aerobic physical activity throughout the week, or at least 75min of vigorous-intensity aerobic physical activity each week, or an equivalent combination of moderate- and vigorous-intensity activities.126,127 Aerobic activity should be performed in bouts of at least 10min duration.126–128 Adults and elderly people with reduced mobility should perform physical activity 3 or more days a week to improve balance and prevent falls.126 Muscle-strengthening exercises should therefore be introduced.126 When people cannot do the recommended amounts of physical activity due to prior chronic disease or functional limitation, they should try to be as physically active as their health allows since any physical activity is better than none.126,129
Exercise intensity can be calculated from various parameters, including126: maximum heart rate (MHR), which is easily obtained: MHR=220−age127; rating of perceived exertion (Borg scale, from 0 to 10)128; respiratory rate (talk test, exercise level that does not make talking impossible or difficult), and METs necessary to perform a physical activity (metabolic rate measurement unit which refers to an individual's rate of energy expenditure at rest).129 Any activity that keeps the heart rate at 65–75% MHR, that scores 5 or 6 on a scale of 0–10, that makes talking difficult but not impossible and that has an intensity of 3.0–5.9MET/min will be considered of moderate intensity.126,128 Vigorous-intensity physical activity is activity that keeps the heart rate at 75–85% MHR, that scores 7 or 8 on a scale of 0–10, that makes talking impossible and that has an intensity of 6.0 or more MET/min in adults and 7 or more in children and young people.126,128 A Spanish version of the Compendium of Physical Activities and the METs required to perform such activities is available on the Internet.130 Modern portable devices for measuring physical activity (pedometers, accelerometers or GPS systems) are effective because they encourage individuals with little or zero inclination to exercise to be more active. Thus, the 150min of moderate-intensity physical activity a week highlighted above for adults and elderly people converts to 7000–8000 steps/day, considering a cadence or speed of 100steps/min, while the cadence of vigorous-intensity physical activity would be 120steps/min.128,129 For children and young people aged 5–17, approximately 12,000 steps/day with a cadence of 120steps/min is recommended.128,129,131
Moderate and non-competitive physical activity is not contraindicated in stable ischaemic heart disease126 or controlled HTN and T2DM, which allow moderate or vigorous-intensity physical activity, unless the individual has proliferative retinopathy.126,127 Prior to starting a home-based exercise programme, an exercise stress test must be performed for any patient with prior CVD.127 Since asymptomatic CVD appears at a younger age, exercise tolerance tests should be done in all diabetic individuals, with both type 1 diabetes mellitus (T1DM) and T2DM, with any of the following characteristics: aged >35years, diabetes duration >15years (T1DM) or >10years (T2DM), microvascular complications (retinopathy, albuminuria or nephropathy), peripheral artery disease, presence of other cardiovascular risk factors or autonomic neuropathy.
How physical activity is prescribedBefore prescribing physical activity to adults, cardiovascular health and metabolic state should be evaluated127: personal and family history, physical examination before beginning to play sports, an ECG at rest and, in the event of prior stable CVD, a stress test. Prescribing sports to a young individual or allowing older healthy individuals to continue playing sports does not tend to pose any medical problems.127 However, before a sedentary adult begins any kind of physical activity, CVD must be ruled out, especially in the presence of associated risk factors (smoking, hypercholesterolaemia, hypertension, etc.).127 Sedentary individuals should start physical activity at a low intensity and duration, gradually increasing both.126 It takes several months for them to reach optimal fitness for their age, but the subjective feeling of improvement is evident within a few weeks. Safe training guidelines would be to start exercise (walking, cycling, etc.) for a period of just 10min, at a slow speed and on alternate days. This would represent some 2500–3000 steps a day, with a cadence of less than 100steps/h. This can then be increased by 5 or 10min each week up to 30–40min (7000–8000 steps a day, with a cadence of 100steps/h). After that, the ideal frequency would be at least 5days a week at an intensity of 65–85% of the theoretical maximum heart rate.
Level of evidence for physical activity and cardiovascular risk
| Evidence | Grade |
|---|---|
| Regular and maintained physical activity offers protection from the onset of cardiovascular diseases and improves risk factors127 | A |
Recommendations
Physical activity must be adapted to each person's individual situation, starting with the principle that something is better than nothing. Regular, moderate-intensity exercise is better than high-intensity exercise. The frequency of exercise is more important than intensity, so it is better to cycle, for example, 50km a week, at a rate of 30km a day (5days), than to cycle the same 50km at the weekend only. The frequency of exercise should be daily, but a minimum of 3–5 times a week is acceptable. It is also better to play sports in a group than alone, but it is not necessary to play as if it were a competition.
Conclusions for clinical practiceClinical research on the effects of lifestyle on general health and cardiovascular health, in particular, has grown exponentially over recent decades. The main reasons for this have included increasing evidence that an unfavourable lifestyle plays a major role in the development and progression of the most prevalent chronic diseases (CVD, diabetes, cancer, neurodegenerative diseases, etc.), and the fact that adherence to a healthy lifestyle can prevent such diseases, delay their onset or slow their progression. A large part of the scientific evidence comes from large long-term cohort studies and from the results of short-term, randomised clinical trials, usually involving small groups of participants. Taking the findings of the most recent meta-analyses as the main reference and with special emphasis on dietary patterns and main food groups, this document summarises evidence gathered on lifestyle components and their association with cardiovascular health, leading to recommendations to reduce cardiovascular risk. With regards to diet, the current paradigm in nutrition science states that the basic nutritional unit is not nutrients (e.g. fatty acids) but the foods that contain such nutrients (oils, nuts, dairy products, red or processed meats, etc.), since there are many nutrients within the food matrix that are capable of interacting synergistically or antagonistically with metabolic pathways that are determinants of health and disease. This is even more relevant for the vast variety of foods and nutrients consumed by humans as part of their regular diet and, over the past decade, the concept of dietary pattern has also been consolidated as the most appropriate concept for examining associations between nutrition and health or disease.
The edible fats section describes oils and margarines. Available evidence shows that polyphenol-rich, extra virgin olive oil has the most beneficial effects on health and that modern margarines contain no TFA but contain n-6 and n-3 PUFA. With regards to eggs, a food rich in nutrients and also in cholesterol, the most recent evidence suggests that consumption of up to one egg a day does not increase cardiovascular risk in general and can even reduce the risk of stroke. Evidence on meats indicates no cardiovascular risk with moderate consumption of white or red meats but an increased risk with processed meats (bacon, sausages, cold meats), which contain harmful additives, such as salt and nitrates. The latest evidence confirms that fish and shellfish, but not fish oil supplements, reduce cardiovascular risk. Regarding dairy products, it is recognised that these are a good source of healthy nutrients, apart from SFA, and that evidence on the association between dairy product consumption and CVD risk factors is not of high quality. However, it is suggested that total dairy product, cheese and yoghurt intake has a neutral or slightly beneficial effect on cardiovascular risk. Pulses and whole grains are seeds containing multiple healthy nutrients and there is moderate- to good-quality evidence that frequent consumption of these food types is associated with a reduction in risk factors and CVD. Nuts are also seeds that are rich in nutrients and, in this case, unsaturated fat. There is also a high level of evidence that frequent nut consumption reduces cholesterolaemia and CVD, especially CHD. Cocoa is another seed with abundant nutrients, and consumption of its main by-product, chocolate, reduces risk factors and is consistently associated with reduced CVD. Commonly consumed beverages, such as coffee (both normal and decaffeinated) and tea, have a very high polyphenol content and there is a high level of evidence that regular consumption is associated with reduced CVD. The consumption of fruit and vegetables is dose dependent and is associated with reduced CVD, more so for stroke than for CHD. Tuber consumption (especially potatoes) is not associated with an increase in cardiovascular risk, unless they are fried in poor-quality oils with added salt.
Consumption of any type of alcoholic beverage increases HDL-C and moderate intake, compared to zero or excessive consumption, is associated with a reduction in CVD and cardiovascular mortality. However, sugar-sweetened beverages are consistently associated with an increase in CVD and risk factors. Numerous functional foods (nutraceuticals) aimed at reducing cardiovascular risk, mainly by reducing cholesterol, have been marketed. There is lots of scientific evidence on the cholesterol-lowering efficacy of plant sterols and soluble fibre products, both of which act in the intestine; although it has not been studied in detail, monacolin, red yeast rice, also reduces cholesterol by producing a statin-like effect. There is also consistent evidence of the triglyceride-lowering effect of pharmacological doses of n-3 PUFA. With regards to salt, there is a high level of evidence that reduced intake lowers blood pressure. Excessive salt intake is thus associated with CVD and cardiometabolic mortality.
Numerous food processing techniques alter the nature of food, both due to loss of beneficial nutrients and the addition of harmful components, such as those added to processed meats. Unlike frying with olive oil, frying with polyunsaturated oils can generate compounds which are harmful for health. Several healthy dietary models are available, such as the Mediterranean diet, the DASH diet, the vegetarian diet and the Alternate Healthy Eating Index (AHEI), all of which are plant based, rich in complex carbohydrates and with limited whole-fat dairy products and meats. Data from large cohort studies and, in the case of the Mediterranean diet, the randomised PREDIMED clinical trial indicate that adherence to these four dietary patterns has a clear cardiovascular benefit. However, a low-fat diet is currently being questioned due to its low potential for cardiovascular protection. There is enough evidence to suggest that there is no standard model of healthy diet, but that biological response varies from one person to the next, especially due to individual differences in genome and microbiome. This is expected to soon lead to personalised and precision nutrition, whereby each person adopts the diet that is of personal benefit to them. One of the most complex issues regarding the relationship between people and their diet is adherence, which depends on very different factors, such as the patient, the family, the health team assigned to the patient and the health system itself. Given that it has been shown that adherence is important, in order to benefit from a healthy diet, the professional must be involved in implementing strategies to achieve adherence. Smoking, even small amounts, is an important cardiovascular risk factor; therefore, smokers should follow strategies for quitting, including both psychosocial and pharmacological intervention. Regular and maintained physical activity protects individuals from cardiovascular risk in a similar way to dietary behaviour. Physical activity recommendations should be personalised according to cardiovascular risk, previous activity and fitness, which should be evaluated before starting.
Recommended frequency of food consumptionTable 5 conveniently shows the recommended frequency of food consumption (food type and quantity) based on the information outlined in this document. These recommendations do not strictly adhere to the traditional Mediterranean diet pyramid since some are based on research results obtained after the traditional pyramid was developed, as mentioned previously in the text.
Frequency of food consumption.
| Consumption frequency | Daily | 3 times a week, maximum | Not advised or occasional |
|---|---|---|---|
| Edible fats | Olive oil, preferably virgin | Margarine | Frying with seed-based oils |
| Eggs | Whole eggs in any dish | Patients with diabetes | |
| Fisha | Oily or white | Shellfish | Salted, smoked fish |
| Meatsb | Poultry and rabbit | Lean red meats | Processed meats and cold meats |
| Dairy products | Semi-skimmed or skimmed milk and yoghurt (sugar free). Fresh cheeses | Full-fat milk and yoghurt (sugar free). Cured cheeses | Butter, cream. Cured cheeses in hypertensive patients |
| Pulses and grains | Whole grains, pulses | Rice, pasta | Refined flour |
| Nuts and peanuts | Raw (30–45g) | Roasted | Salted |
| Chocolate | Dark with cocoa ≥70% | Dark with cocoa <70% | Milk and white chocolate |
| Coffee and tea | Unlimited tea. Coffee up to 5 cups a day, without sugar | ||
| Fruit, vegetables, starchy vegetables | 4–5 portions, combining different types of fruit and vegetables | High-starch foods (potatoes) | Commercial fruit juices and commercial French fries or chips |
| Alcoholic beverages | Limit to 30g of alcohol in men and 15g in women. Preferably fermented beverages (wine, beer) with meals | Not advised for non-drinkers | |
| Products with added sugar | Avoid any food with added sugar | ||
| Food preparationc | Preferably boiled, grilled or sautéed. | Food fried in virgin olive oil | Avoid smoked and processed foods and foods fried in refined oils |
| Salt | 2.5–4g daily | Salted fish and meat |
ER has received remuneration for the preparation of didactic material and research grants through the California Walnut Commission and is an unpaid member of its Scientific Advisory Committee. FPJ, JLM, JDL and PPM have taken part in training activities funded by Patrimonio Comunal Olivarero, Spain.
Please cite this article as: Pérez-Jiménez F, Pascual V, Meco JF, Pérez Martínez P, Delgado Lista J, Domenech M, et al. Documento de recomendaciones de la SEA 2018. El estilo de vida en la prevención cardiovascular. Clín Investig Arterioscler. 2018;30:280–310.