SmartLab 2.0 is an innovative concept of multidisciplinary collaboration between the clinical laboratory and the diabetes day unit that was born with the aim of identifying patients at high cardiovascular risk who require priority attention, such as patients with atherogenic dyslipidemia, in order to create a cardiovascular prevention strategy.
ObjectiveImplementation in the Laboratory Information System (LIS) of an automated biochemical algorithm for the identification of patients with atherogenic dyslipidemia in routine analyses and priority referral to the diabetes day unit.
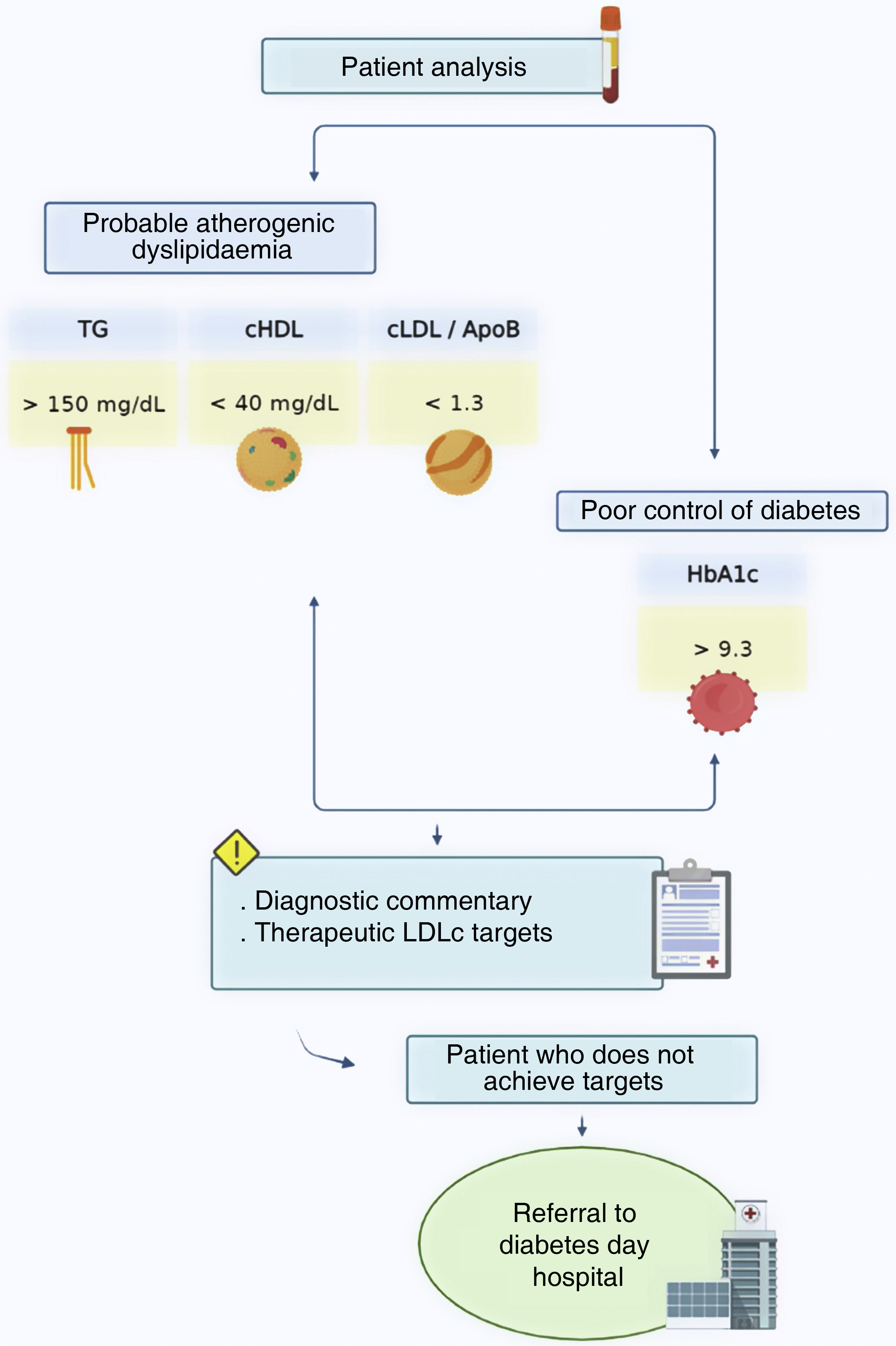
Material and methodsThe algorithm designed in the SIL was: HBA1c>9.3+TG>150mg/dl+HDLc<40mg/dl+LDL/ApoB<1.3. A comment was inserted alerting the requesting physician of the diagnosis of atherogenic dyslipidemia and priority referral was made from the laboratory to the diabetes day unit in the necessary cases.
ResultsIn the 1-year period, a total of 899 patients with HBA1c>7 and atherogenic dyslipidemia criteria were identified. Of these, 203 patients from primary care with HbA1c>9.3 were referred to the diabetes day hospital.
ConclusionsReinforcement of cardiovascular prevention is necessary at all levels. The clinical laboratory should play a fundamental role in the diagnosis of dyslipidemias. Early detection of patients at high cardiovascular risk is essential and collaboration between the different clinical units is fundamental to guarantee patient safety.
El SmartLab 2.0 es un concepto innovador de colaboración multidisciplinar entre el laboratorio clínico y la unidad de día de diabetes que nace con el objetivo de identificar a pacientes de alto riesgo cardiovascular que requieran una atención prioritaria, como son los pacientes que presentan dislipemia aterogénica, con el fin de crear una estrategia de prevención cardiovascular.
ObjetivoImplementación en el sistema informático de laboratorio (SIL) de un algoritmo bioquímico automatizado para la identificación en analíticas de rutina de pacientes con dislipemia aterogénica y derivación prioritaria a la unidad de día de diabetes.
Material y métodosSe diseñó en el SIL el algoritmo: HBA1c>9,3+TG>150mg/dl+cHDL<40 mg/dl+LDL/ApoB es<1,3. Se inserta un comentario alertando al médico peticionario del diagnóstico de dislipemia aterogénica y se procede a la derivación prioritaria desde el laboratorio a la unidad de día de diabetes en los casos necesarios.
ResultadosEn el periodo de un año se han identificado a un total de 899 pacientes con HBA1c>7 y criterio de dislipemia aterogénica. De ellos, 203 pacientes procedentes de atención primaria con HbA1c>9,3 se derivaron al hospital de día de diabetes.
ConclusionesEl refuerzo de la prevención cardiovascular es necesario a todos los niveles. El laboratorio clínico debe jugar un papel fundamental en el diagnóstico de las dislipemias. La detección temprana de los pacientes con alto riesgo cardiovascular es primordial y la colaboración entre las distintas unidades clínicas es fundamental para garantizar la seguridad del paciente.
Cardiovascular disease (CVD) is still the most common cause of death worldwide, vastly surpassing the number of deaths due to cancer.1 Furthermore, it is calculated that no less than 60 million years of potential life are lost due to CVD in Europe every year, showing the resulting high incidence of premature deaths.2
Atherosclerosis is considered to be a direct cause of CVD, and alterations in the normal concentrations of lipids and lipoproteins favour the appearance of atherosclerosis, so that dyslipidaemia is a major cardiovascular risk factor.3
One type of dyslipidaemia known as atherogenic dyslipidaemia is associated with especially high cardiovascular risk due to the individual and synergic action of its three main components: an increase in total triglycerides (TG), a fall in cholesterol bound to high density lipoproteins (HDLc) and the presence of small dense LDL particles.4 It is also usually accompanied by a rise in apolipoprotein B (ApoB), which is present in all non-HDL and therefore reflects the total number of lipoproteins associated with cardiovascular disease (LDL, residual particles and Lp[a]).5
Atherogenic dyslipidaemia is normally associated with different conditions and diseases, such as being overweight, obesity, diabetes mellitus and metabolic syndrome.6 Special mention should be made of diabetes, as it is estimated that up to 41% of diabetic patients in our country have atherogenic dyslipidaemia.7 Therefore, given that diabetes is considered to be a cardiovascular risk factor in itself, the combination of both of these entities multiplies the predisposition of these patients to suffer cardiovascular events. In fact, CVD is the main cause of morbimortality in type 2 diabetes mellitus.8 This is why early diagnosis and the use of corrective therapeutic measures is fundamental in such cases, to guarantee the health of these patients.
SmartLab 2.0 is an innovative concept for multidisciplinary cooperation between the clinical laboratory and the day diabetes unit. It aims to identify patients at high or very high cardiovascular risk who should receive priority attention, including those who have atherogenic dyslipidaemia. The ultimate aim is to create a cardiovascular prevention strategy in primary care. It is fundamentally based on the implementation of analytical warnings for doctors who have requested an analysis, by applying automatic computerized algorithms within the laboratory’s information system. These algorithms are reviewed and validated by the laboratory analyst, and the system also resolves electronic consultations, which are new valid tools for the consolidation of cardiovascular health strategies in n collaboration with the diabetes day unit.
The objective of this study was to implement an automated biochemical algorithm within the laboratory information system (LIS) for the identification within routine analyses of diabetic patients who fulfil the criteria for atherogenic dyslipidaemia, and the priority referral of the corresponding cases to the diabetes day unit, together with the creation of a specific electronic facility for this with primary care.
Material and methodsAn automated biochemical algorithm was implemented in the LIS, defined as glycated haemoglobin (HbA1c)>7+TG>150mg/dl+HDLc<40mg/dl+LDLc/ApoB<1.3 (a ratio below 1.3 is compatible with the presence of potentially atherogenic small dense LDL particles).9 The following legend is automatically inserted into any routine analysis that fulfils the four criteria, depending on the HbA1c value and highlighting the therapeutic targets according to patient risk.
If HbA1c>7Warning: “The patient has a lipid triad that indicates atherogenic dyslipidaemia: a high concentration of TG, low HDLc and the presence of small dense potentially atherogenic particles”.
According to 2019 European Society of Cardiology guidelines, the therapeutic targets in diabetic patients are:
- •
Very high-risk patients: SCORE>10%. Reduction of LDLc>50% respecting the basal value, and LDLc<55mg/dl.
- •
High risk patients: SCORE>5% y <10%. Reduction of LDLc>50% respecting the basal value, and LDLc<70mg/dl.
In this way all patients with possible atherogenic dyslipidaemia are characterized and marked in the LIS with their corresponding diagnostic remarks in the report on analysis, for the attention of the doctor who requested the analysis.
If HbA1c>9.3Given that HbA1c above certain levels has been found to multiply cardiovascular risk,10,11 agreement was reached with the diabetes day unit that, in the integrated care process for diabetes mellitus of the Board of Health of the Regional Government of Andalucía, a level above 9.3 was set for priority referral to the said unit.
In the validation procedure, the laboratory analyst reviews the analyses that fulfil the criteria for atherogenic dyslipidaemia and which have a result for HbA1c higher than 9.3. If these patients have not achieved the LDLc targets and come from primary care, as well as the warning about patients con HbA1c>7, they are recommended for priority referral to the diabetes day hospital or the possibility of e-consultation for atherogenic dyslipidaemia in the lipid laboratory. Both routes are committed to replying or making an appointment within 48h. Fig. 1 shows the flow of working.
Diagram of the process initiated when diabetic patients with probable severe atherogenic dyslipidaemia are detected by analysis. Activation of the algorithm triggers the implementation of an analytical warning.
PC: primary care; ApoB: apolipoprotein B; HDLc: cholesterol bound to high density lipoproteins; LDLc: cholesterol bound to low density lipoproteins; HbA1c: glycated haemoglobin; TG: triglycerides.
A descriptive retrospective analysis was performed of the analytical data of the patients with HbA1c>7 to evaluate the performance of the said algorithm, which was activated from January to December 2021. The following analytical parameters were analysed to describe the biochemical characteristics of the population in question:
- •
Lipid profile: triglycerides, total cholesterol, LDL cholesterol, HDL cholesterol, apolipoprotein B and the LDLc/ApoB coefficient.
- •
Evaluation of diabetes: glycated haemoglobin.
- •
Evaluation of kidney function: glomerular filtration (estimated based on the CKD-EPI equation) and the albumin/creatinine coefficient.
The number of analytical warnings issued is described, together with whether the patients met their lipid targets or not. The statistical software used for this study was R Commander (version 2.8–0). The Shapiro–Wilk test was used to study the normalcy of the variables.
ResultsDuring 2021 the diagnostic algorithm for atherogenic dyslipidaemia was activated in 899 patients with HbA1c>7. 730 of these patients came from primary care, 132 from specialized departments and 37 from hospitalization. The population identified was composed of 619 men and 280 women, with an average age of 61 years old.
The main biochemical characteristics, and the ones that were found to be the most useful in characterizing the general population obtained, are shown in Table 1. Due to the non-normalcy of the variables, data are shown in terms of the median and interquartile range.
General biochemical characteristics of the diabetic population identified (HbA1c>7) expressed as the median and interquartile range.
| Parameter | Median (interquartile range) |
|---|---|
| TG (mg/dl) | 402 (337–509) |
| TC (mg/dl) | 197 (167–233) |
| LDLc (mg/dl) | 101 (75–126) |
| HDLc (mg/dl) | 33 (29–37) |
| ApoB (mg/dl) | 119 (101–140) |
| LDL/ApoB | 0.85 (0.72–0.96) |
| HbA1c (%) | 8.5 (7.6–10) |
| GF (ml/min/1.73m2) | 90 (65–102) |
ApoB: apolipoprotein B; HDLc: cholesterol bound to high density lipoproteins; LDLc: cholesterol bound to low density lipoproteins; TC: total cholesterol; GF: glomerular filtration rate; HbA1c: glycated haemoglobin; TG: triglycerides.
The following results were obtained in this population regarding the achievement of lipid targets (defined specifically for diabetic patients who were at least at high risk due to the presence of dyslipidaemia)12 and the recommendations for normal values of total cholesterol:
- •
LDL cholesterol <70mg/dl: 196 patients achieved the target (21.8% of the population).
- •
Apolipoprotein B <80mg/dl: 52 patients achieved the target (5.8% of the population).
- •
Total cholesterol <200mg/dl: 463 patients achieved the target (51.5% of the population).
Different degrees of severity were defined for triglyceride analysis. A TG concentration higher than 500mg/dl is considered to be severe hypertriglyceridemia. A total of 237 patients had a result of TG >500mg/dl (26.4% of the population).
Respecting kidney function, a glomerular filtration rate below 60ml/min/1.73m2 (indicating a poor filtration rate and kidney damage) was detected in 184 patients (20.5% of the population).
Of the 899 patients with HbA1c>7 and diagnosed atherogenic dyslipidaemia, 307 had a result of HbA1c>9.3 (34.1% of the population). Of these, 253 came from primary care, 36 came from specialized departments and 18 from hospitalization. After review by a doctor of these figures it was found that only 65 patients were within the targets set for LDLc (LDLc<70mg/dl). Of the remaining 242 patients who did not meet the targets, 203 came from primary care and were referred to the diabetes day hospital for cardiovascular prevention due to their high risk.
DiscussionDyslipidaemia is common in patients with diabetes, and it adds to the increased risk of cardiovascular events and death. Genetic factors, lifestyle, hypertension, kidney disease, obesity, inflammation, a prothrombotic state, the duration of diabetic disease and control of glycaemia are also important cardiovascular risk factors within this context.13
Clinical laboratories should play a fundamental role in the detection of dyslipidaemia, given that the diagnosis is always based on analytic proof of lipid alteration. Thus, by combining serum biomarkers and the implementation of biochemical algorithms in information systems it is possible to identify patients at an early stage and reclassify them correctly. To this end, in our nutrition and cardiovascular risk laboratory we implemented an automated algorithm for the detection of the most common form of dyslipidaemia in diabetic patients: atherogenic dyslipidaemia.
An initial evaluation of the project found that we had diagnosed almost 900 patients with atherogenic dyslipidaemia, adding an explanation commentary in the analytical report and enhancing the post-analytical phase. We also activated more than 300 diagnostic analytical warnings of severe atherogenic dyslipidaemia, and more than 200 primary care patients with poor lipid and diabetic control were prioritized for referral to the diabetes day hospital for cardiovascular prevention in 2021. Taking into consideration the substantial pressure during the said year due to the COVID-19 pandemic, and the fact that fewer analyses were received by our laboratory, this figure cannot be ignored. In fact, once these cases have been detected it is primordial to refer them for specialized care, when necessary, given that these patients are at very high cardiovascular risk. To achieve this, it is fundamental for the laboratory to cooperate with clinical units, and this is achieved with this model SmartLab 2.0, interconnecting the laboratory with the clinical and with the patient.
When the average values of the population studied (899 patients) are examined, our results can be said to be comparable with those reported by the Atherogenic Dyslipidaemia Work Group of the Spanish Society of Atherosclerosis in its PREDISAT study. They concluded that diabetic patients with atherogenic dyslipidaemia had an average triglyceridaemia level close to 500mg/dl, and HDLc at 33mg/dl. Our population had an average triglyceridaemia of 437mg/dl and HDLc at 32mg/dl.
The 2021 European Society of Cardiology Guide on the prevention of cardiovascular disease in clinical practice states that cardiovascular risk factors are generally poorly treated even in patients who are considered to be at high risk, including patients with diabetes mellitus and atherogenic dyslipidaemia.14,15 This statement agrees with the results obtained in our study, as when the lipid parameters of the selected patients were described, it was found that the majority had not achieved their targets.
78.2% of the sample population did not meet their target for LDLc, and 94.2% did not achieve the expected ApoB target figures for diabetic patients. Moreover, many patients had very high total cholesterol and severe hypertriglyceridaemia.
These results underline the need to reinforce all levels of cardiovascular prevention. Implementing biochemical algorithms and enhancing analytic reports with diagnostic remarks and explanations is a simple way of contributing to cardiovascular prevention, and this was the ultimate aim of this project. It is of primordial importance to detect these patients early to prevent progression to complicated or fatal cardiovascular disease, and it is fundamental for different clinical units to work together to thereby guarantee patient safety.
As limitations of this study, we can assume that it is not possible to calculate the actual prevalence of atherogenic dyslipidaemia in our area during 2021 based on these data, given that if the algorithm is to activate, analysis must find a complex lipid profile (which includes ApoB), and this is not requested in the majority of basic analyses.
ConclusionsThe implementation of a SmartLab 2.0 which promotes multidisciplinary collaboration between the clinical laboratory and the diabetes day unit can be an effective means of identifying patients with atherogenic dyslipidaemia.
The automated algorithms in the LIS make it possible to identify a high number of patients with poor control of glycaemia and atherogenic dyslipidaemia who do not fulfil desirable targets according to their degree of risk, so that those with the most severe cardiovascular risk can receive priority referral to the diabetes day unit.
FinancingThis paper was partially financed by the SEA grant awarded in 2021 with the title “Aplicación de la telemedicina de laboratorio en atención primaria para la prevención de la enfermedad cardiovascular”.
Conflict of interestsThe authors have no conflict of interests to declare.