The current guidelines on hypoparathyroidism offer a model for treating patients but do not cover real-world situations or patient diversity. Given the lack of data regarding hypoparathyroidism, a Delphi panel was convened in Spain to establish consensus in defining the characteristics of patients with chronic hypoparathyroidism not adequately controlled with conventional treatment, as well as to investigate patterns of management.
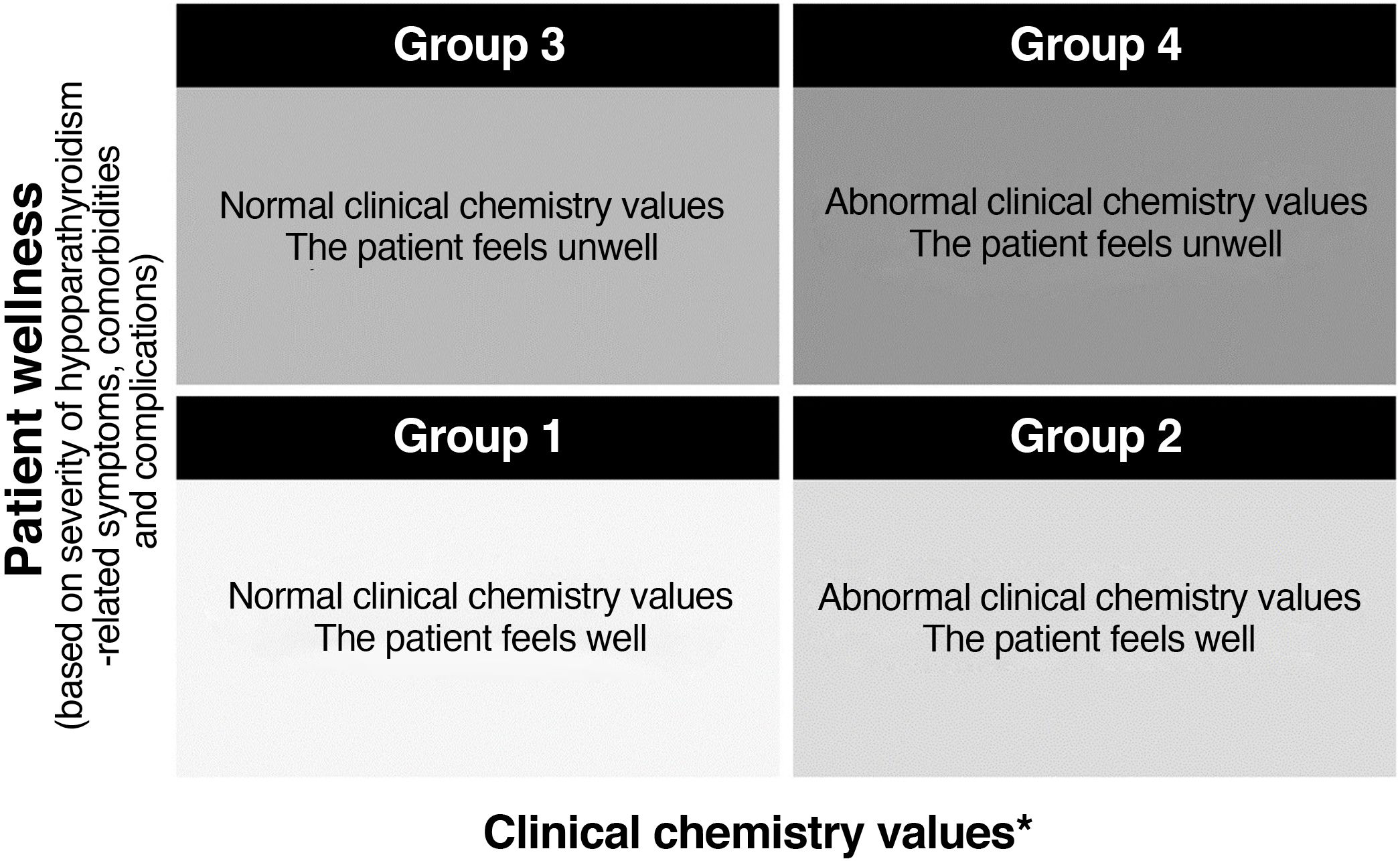
Material and methodsA presentation matrix provided a framework for characterizing inadequately controlled chronic hypoparathyroidism, based on four predefined patient groups: group 1 (normal biochemical levels and the patient feeling well); group 2 (abnormal biochemical levels and the patient feeling well); group 3 (normal biochemical levels and the patient feeling unwell); and group 4 (abnormal biochemical levels and the patient feeling unwell). Based on Likert scales (scored 1–9), the experts were asked to state their agreement/disagreement with the characteristics of patients with chronic hypoparathyroidism, including demographic data, family history, comorbidities, biochemical values, symptoms and quality of life. Consensus was achieved when ≥66% of the respondents were in agreement.
ResultsConsensus was achieved on the importance of assessing demographic data and comorbidities (e.g., renal complications) in groups 2, 3 and 4; family medical history in groups 2 and 3; biochemical parameters (e.g., calcemia/urinary calcium excretion) in groups 2 and 4; and clinical symptoms and quality of life in groups 3 and 4. Consensus was also reached regarding the maintenance of several biochemical parameters and the need for personalized treatment and training in symptoms and complications.
ConclusionsThe Spanish expert panel reached consensus defining key disease parameters and factors of importance for characterizing and treating patients with inadequately controlled chronic hypoparathyroidism.
Las directrices actuales sobre el hipoparatiroidismo ofrecen un modelo para tratar a los pacientes, pero no abarcan situaciones de la práctica real ni la diversidad de pacientes. Dada la falta de datos respecto al hipoparatiroidismo, se reunió un panel Delphi en España con el fin de obtener un consenso para definir las características de los pacientes con hipoparatiroidismo crónico no adecuadamente controlado con el tratamiento convencional, así como para investigar los patrones del manejo.
Materiales y métodosUna matriz de presentación proporcionó un marco para caracterizar el hipoparatiroidismo crónico no adecuadamente controlado basándose en cuatro grupos de pacientes predefinidos: grupo 1, valores bioquímicos normales y que el paciente se siente bien; grupo 2, valores bioquímicos anormales y que el paciente se siente bien; grupo 3, valores bioquímicos normales y que el paciente se siente mal; grupo 4, valores bioquímicos anormales y que el paciente se siente mal. Por medio de escalas de Likert (puntuadas de 1 a 9), se pidió a los expertos que indicaran su acuerdo o desacuerdo respecto a las características de los pacientes con hipoparatiroidismo crónico, entre ellas, datos demográficos, antecedentes familiares, enfermedades concomitantes, valores bioquímicos, síntomas y calidad de vida. El consenso se alcanzó al mostrarse de acuerdo un mínimo del 66% de los encuestados.
ResultadosSe alcanzó el consenso respecto a la importancia de evaluar los datos demográficos y las enfermedades concomitantes (p. ej., complicaciones renales) en los grupos 2, 3, y 4, los antecedentes médicos familiares en los grupos 2 y 3, los parámetros bioquímicos (p. ej., calcemia/excreción urinaria de calcio) en los grupos 2 y 4 y los síntomas clínicos y la calidad de vida en los grupos 3 y 4. También se alcanzó el consenso respecto al mantenimiento de varios parámetros bioquímicos y la necesidad de un tratamiento personalizado y de formación sobre los síntomas y complicaciones.
ConclusionesEl panel de expertos español llegó a un consenso que definía los factores y los parámetros clave de la enfermedad importantes para caracterizar y tratar a los pacientes con hipoparatiroidismo crónico no adecuadamente controlado.
- •
Conventional treatment may not control hypoparathyroidism.
- •
Clinical chemistry and wellness parameters are considered in four predefined groups.
- •
Management patterns for patients not adequately controlled are defined.
- •
It is important to assess the parameters and symptoms of the disease in all groups.
- •
Personalised treatment and patient education are required.
Hypoparathyroidism is a rare endocrine disorder resulting from the absence of parathyroid hormone (PTH) or unduly low levels of this hormone.1 PTH regulates calcium homeostasis through a negative feedback loop. Therefore, PTH deficiency alters calcium homeostasis, leading to hypocalcaemia.2 The estimated prevalence of permanent hypoparathyroidism after thyroid surgery ranges from 1.6% to 14.5% in different countries, based on figures from national registries and large multicentre studies.3–11 It should be noted that there were considerable differences in the definition of chronic hypoparathyroidism. Although in most studies it was defined as the need for calcium or vitamin D supplements 6 months after the procedure, in others no definition was specified or the only condition was administration of vitamin D supplements. The conventional treatment for hypoparathyroidism consists of calcium supplements and active vitamin D.2
Although the European Society of Endocrinology guidelines offer a model for treating patients,12 they do not necessarily cover all real-world situations, the diversity of patient profiles or a standard definition of patients whose chronic hypoparathyroidism is not adequately controlled with conventional treatment. Given the general lack of data regarding hypoparathyroidism, a Delphi panel was convened in Spain to establish a consensus in defining the characteristics associated with chronic hypoparathyroidism not adequately controlled with conventional treatment. The secondary objective was to investigate management patterns in Spain.
Materials and methodsPatient classification matrixTo define hypoparathyroidism severity, we used a previously reported patient classification matrix.13 Briefly, the matrix uses two axes, clinical chemistry values and patient wellness (including symptoms, comorbidities and complications), and classifies adult patients with hypoparathyroidism into four groups. Predefined patient groups provide experts with a framework for identifying important parameters that characterise patients who are considered to meet the criteria for that group.
Abnormal clinical chemistry was defined in the classification matrix as clinical chemistry meeting the following criteria: serum calcium concentration adjusted for albumin <2.0 mmol/l (8.0 mg/dl) on at least three or four occasions a year, even while receiving ≥3 μg/day of active vitamin D, wide fluctuations in calcium for no apparent reason but with considerable time outside normal limits, serum phosphate concentration >1.6 mmol/l (5.0 mg/dl) and 24-h urinary calcium excretion >7.5 mmol (300 mg) in males and >6.25 mmol (250 mg) in females. Patient wellness was defined based on severity of hypoparathyroidism-related symptoms, comorbidities and complications, with signs and symptoms grouped into three categories: disease-specific, disease-related, and general/nonspecific. Disease-specific signs and symptoms were those independently indicative of severe hypoparathyroidism, such as seizures. Disease-related signs and symptoms were those appearing together and occurring repeatedly, such as paraesthesia and cramps. General/nonspecific signs and symptoms included cardiac arrhythmias, anxiety and obesity.
The patient classification matrix13 is shown in Fig. 1 and illustrates the following four groups: group 1 (patients with normal clinical chemistry who feel well), group 2 (patients with abnormal clinical chemistry who feel well), group 3 (patients with normal clinical chemistry who feel unwell) and group 4 (patients with abnormal clinical chemistry who feel unwell).
Patient classification matrix.13
*Clinical chemistry values considered independently of patients’ symptoms.
A Delphi expert panel was convened in Spain, using the RAND/UCLA Appropriateness Method14 as a model, to define chronic hypoparathyroidism not adequately controlled with conventional treatment, according to the patient classification matrix. The Delphi method is a widely used and accepted technique for achieving a convergence of opinion of experts in their respective fields on real-world issues.15 With the Delphi technique, group opinions are solicited using iterative voting. After each round of voting, group and individual responses are scrutinised by members of the expert panel. Finally, a consensus is reached through a process of multiple iterations that involves identifying common trends and examining outliers.
The RAND/UCLA Delphi method differs from the conventional method in that the experts do not have a formal obligation to reach a consensus; instead, a group meeting is held to discuss areas of agreement and disagreement.
In this survey, the first of the two rounds of the RAND/UCLA Delphi method consisted of each expert completing a questionnaire. In the second round, areas of disagreement were investigated and the experts were then asked to reconsider the questions based on the group conversation.
ParticipantsFifty clinical endocrinologists, endocrine surgeons and internal medicine specialists were invited to take part. In order to represent a variety of patients, we selected hospital clinics in different regions. As hypoparathyroidism is a rare disease with a limited number of medical experts, Shire Pharmaceuticals Ibérica SL (Madrid, Spain, a Takeda company) contacted two medical associations to which most Spanish endocrinologists belong: the Sociedad Española de Endocrinología y Nutrición [Spanish Association of Endocrinology and Nutrition] (SEEN) and the Sociedad Española de Investigación Ósea y del Metabolismo Mineral [Spanish Association of Bone and Mineral Metabolism Research] (SEIOMM). Both associations provided Comunicación y Ediciones Sanitarias [Health Communication and Publications] (CYESAN) SL (Madrid, Spain) with a list of endocrinologists who treat hypoparathyroidism, and the expert panel was created from that list. Shire did not select the experts or make any contributions after the experts were selected by the medical associations. Shire also did not have access to the experts’ answers.
Questionnaire and interaction of expert panelThe questionnaire was developed in the United Kingdom and identified the variables associated with chronic hypoparathyroidism. These were then validated from a Swedish perspective by a Norwegian clinical expert. The Swedish version of the questionnaire13 was then translated into Spanish for this survey. However, in the resulting translation there were some unintended differences between the Spanish version of the Delphi questionnaire and the questionnaire used in Sweden. In particular, there was a difference in the question related to the definition of “not adequately controlled” hypoparathyroidism: the Spanish questionnaire asked the experts whether or not it was “important to assess” certain characteristics or parameters in order to define disease that is not adequately controlled, while the questionnaire in Sweden asked the “degree of importance” of individual characteristics or parameters in defining a patient’s disease as not adequately controlled. Furthermore, while the panellists in Spain were asked about adherence to treatment, they were not asked about patient adherence problems. The questions for which a consensus was sought were grouped according to the classification matrix.13 A copy of the full questionnaire used in Spain is provided in Appendix B Table S1 of the Annex.
The experts were asked to rate various statements on a 9-point Likert scale (1 = strongly disagree; 9 = strongly agree). The responses were ranked as follows: from 1 to 3, I disagree with the statement (the lower the score, the greater the degree of disagreement); from 4 to 6, I do not agree or disagree with the statement or I do not have a clearly defined opinion on this question (a lower score was closer to disagreement and a higher score was closer to agreement); and from 7 to 9, I agree with the statement (the higher the score, the greater the degree of agreement). The experts had the option of adding a comment to explain or clarify their choices.
The clinical characteristics were grouped into the following categories: demographic data, family history, concomitant diseases, clinical chemistry values, symptoms and impact on quality of life reported by the patient. The experts were asked whether assessment of age, sex, personal history, social situation and adherence to treatment was important in defining a patient’s disease as not adequately controlled with conventional treatment.
Data analysisConsensus was defined as agreement among at least 66% of the survey respondents. Descriptive statistics are presented.
ResultsOf the 50 experts invited, 35 completed both rounds of the survey.
Patients with disease not adequately controlledThe majority of the participants (94.6%) agreed that chronic hypoparathyroidism in patients included in group 1 of the patient classification matrix (patients with normal clinical chemistry who feel well) is considered controlled with conventional treatment.
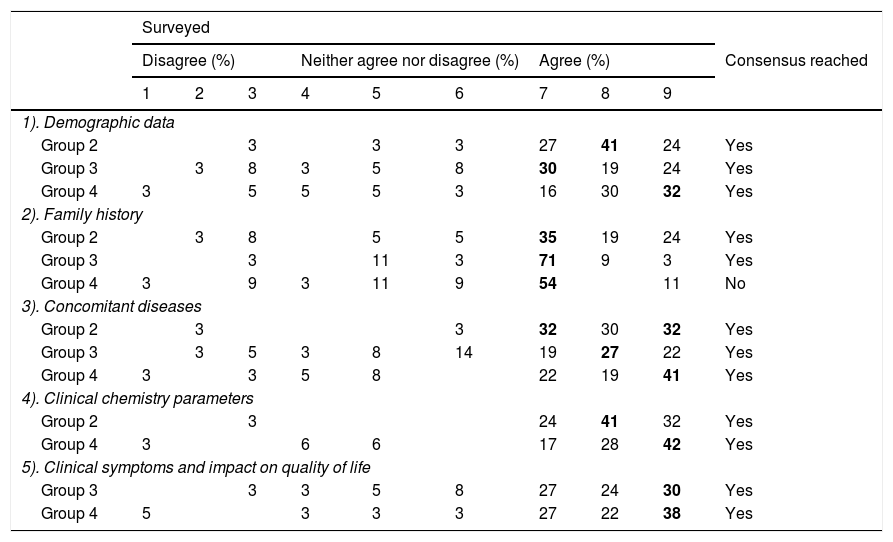
Important characteristics in the assessment of patients with chronic hypoparathyroidism not adequately controlled with conventional treatmentThe characteristics that, by consensus, were considered important in the assessment of a patient with disease not adequately controlled with conventional treatment are summarised in Table 1. A detailed description of the statements reviewed by the Delphi group in relation to characteristics of patients with chronic hypoparathyroidism is provided in Appendix B Table S1. The experts reached an agreement on most of the statements in round 1. In general, the experts reached an agreement in all groups with respect to demographic data and comorbidities, in groups 2 and 4 with respect to clinical chemistry parameters and in groups 3 and 4 with respect to clinical symptoms and quality of life. Interestingly, to define a patient’s disease as not adequately controlled with conventional treatment, in groups 2 and 3, the experts agreed that it is important to assess the patient’s family history of hypoparathyroidism, bone disease, fractures, other endocrine disorders and nephrolithiasis. However, they did not reach an agreement in group 4 (Table 1).
Percentage of experts who answered the survey questions.
| Surveyed | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Consensus reached | |||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| 1). Demographic data | ||||||||||
| Group 2 | 3 | 3 | 3 | 27 | 41 | 24 | Yes | |||
| Group 3 | 3 | 8 | 3 | 5 | 8 | 30 | 19 | 24 | Yes | |
| Group 4 | 3 | 5 | 5 | 5 | 3 | 16 | 30 | 32 | Yes | |
| 2). Family history | ||||||||||
| Group 2 | 3 | 8 | 5 | 5 | 35 | 19 | 24 | Yes | ||
| Group 3 | 3 | 11 | 3 | 71 | 9 | 3 | Yes | |||
| Group 4 | 3 | 9 | 3 | 11 | 9 | 54 | 11 | No | ||
| 3). Concomitant diseases | ||||||||||
| Group 2 | 3 | 3 | 32 | 30 | 32 | Yes | ||||
| Group 3 | 3 | 5 | 3 | 8 | 14 | 19 | 27 | 22 | Yes | |
| Group 4 | 3 | 3 | 5 | 8 | 22 | 19 | 41 | Yes | ||
| 4). Clinical chemistry parameters | ||||||||||
| Group 2 | 3 | 24 | 41 | 32 | Yes | |||||
| Group 4 | 3 | 6 | 6 | 17 | 28 | 42 | Yes | |||
| 5). Clinical symptoms and impact on quality of life | ||||||||||
| Group 3 | 3 | 3 | 5 | 8 | 27 | 24 | 30 | Yes | ||
| Group 4 | 5 | 3 | 3 | 3 | 27 | 22 | 38 | Yes | ||
Percentage of experts who answered the survey questions on the characteristics considered important by consensus in the assessment of a patient whose disease is not adequately controlled with conventional treatment using scores on a Likert scale (1 = strongly disagree; 9 = strongly agree).
The numbers in bold reflect the answer selected by the majority of the experts.
Group 2: abnormal clinical chemistry values; the patient feels well. Group 3: normal clinical chemistry values; the patient feels unwell. Group 4: abnormal clinical chemistry values; the patient feels unwell.
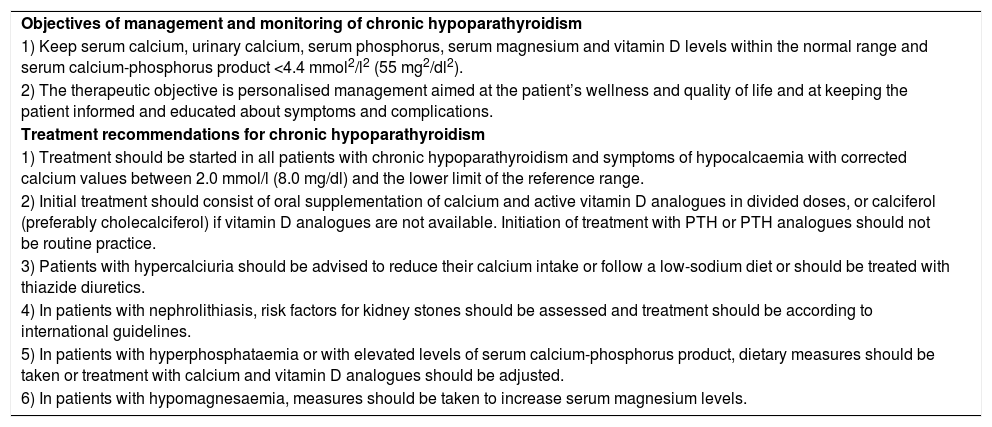
The experts agreed on the therapeutic objectives of the management of patients with chronic hypoparathyroidism and the therapeutic regimen aimed at achieving the treatment objectives, which are summarised in Table 2. As in the case of the characteristics important for assessing patients with chronic hypoparathyroidism, the experts agreed on most of the statements in round 1. A full description of the secondary objectives for which the expert panel reached a consensus regarding the treatment of chronic hypoparathyroidism is provided in Appendix B Table S1.
Summary of consensus statements for the follow-up and management of patients with chronic hypoparathyroidism.
| Objectives of management and monitoring of chronic hypoparathyroidism |
| 1) Keep serum calcium, urinary calcium, serum phosphorus, serum magnesium and vitamin D levels within the normal range and serum calcium-phosphorus product <4.4 mmol2/l2 (55 mg2/dl2). |
| 2) The therapeutic objective is personalised management aimed at the patient’s wellness and quality of life and at keeping the patient informed and educated about symptoms and complications. |
| Treatment recommendations for chronic hypoparathyroidism |
| 1) Treatment should be started in all patients with chronic hypoparathyroidism and symptoms of hypocalcaemia with corrected calcium values between 2.0 mmol/l (8.0 mg/dl) and the lower limit of the reference range. |
| 2) Initial treatment should consist of oral supplementation of calcium and active vitamin D analogues in divided doses, or calciferol (preferably cholecalciferol) if vitamin D analogues are not available. Initiation of treatment with PTH or PTH analogues should not be routine practice. |
| 3) Patients with hypercalciuria should be advised to reduce their calcium intake or follow a low-sodium diet or should be treated with thiazide diuretics. |
| 4) In patients with nephrolithiasis, risk factors for kidney stones should be assessed and treatment should be according to international guidelines. |
| 5) In patients with hyperphosphataemia or with elevated levels of serum calcium-phosphorus product, dietary measures should be taken or treatment with calcium and vitamin D analogues should be adjusted. |
| 6) In patients with hypomagnesaemia, measures should be taken to increase serum magnesium levels. |
As shown in Appendix B Table S1, there was a consensus on most of the statements about what it is important to assess in the patients in each group. Exceptions were seen in group 4 (patients with abnormal clinical chemistry who feel unwell), where a consensus was not reached on the investigation of the patient’s family history to define the patient’s condition as not adequately controlled. The experts pointed out that these assessments were not necessary, as the patient’s clinical chemistry abnormalities and symptoms were sufficient to suggest that the patient’s hypoparathyroidism was not controlled. There were also several therapeutic approaches to the disease on which no consensus was reached, including: initiation of treatment in asymptomatic patients with calcium levels at the lower limit of normal to improve their wellness; conventional therapy consisting of vitamin D supplements, thiazide diuretics or a low-sodium diet to control hypercalciuria; and additional vitamin D supplements at a dose of 400–800 IU/day for patients treated with active vitamin D. There was a consensus in disagreeing that routine treatment should consist of phosphate binders and a low-phosphorus diet to control hyperphosphataemia as well as administration of magnesium supplements.
DiscussionThe current outlook on treatment of chronic hypoparathyroidism based on the European guidelines is focused on keeping serum calcium within a desired range.12,16 However, calcium control is not always accompanied by restoration of mineral homeostasis. This underlines the need to assess other variables to improve the treatment of hypoparathyroidism.12,16
This study used the RAND/UCLA Delphi technique with a patient classification matrix, previously used in three other European countries,13 to identify the characteristics of patients with chronic hypoparathyroidism not adequately controlled with conventional treatment in Spain. The degree of consensus obtained in the study was generally high: the experts reached a consensus on 35 of the 39 statements.
A consensus was achieved on the importance of assessing the demographic data and the spectrum of related comorbidities, renal complications in particular, in matrix groups 2 through 4; family medical history in groups 2 and 3; clinical chemistry parameters, including serum calcium, phosphorus, magnesium and calcium-phosphate product, in groups 2 and 4; and clinical parameters in groups 3 and 4 in order to define a patient’s disease as not adequately controlled with conventional therapy (Appendix B Table S1). A consensus was not reached on assessing the patient’s family medical history in group 4, because the experts pointed out that classification of the disease as “not adequately controlled” based on clinical chemistry parameters and symptoms made assessment of family background unnecessary.
The characteristics that define patients with chronic hypoparathyroidism not adequately controlled with conventional treatment established in this study for Spain are consistent with the general consensus reported for the United Kingdom, Sweden and Portugal.13 In both studies, comorbidities associated with gastrointestinal disorders accompanied by malabsorption, kidney failure, development of kidney stones and calcifications and hypercalciuria, and clinical chemistry abnormalities (serum calcium, urinary calcium and creatinine) were important in patients in group 2; tingling or numbness in the hands and feet were important in patients in group 3; and comorbidities associated with gastrointestinal disorders accompanied by malabsorption, development of kidney stones and calcifications and hypercalciuria, clinical chemistry abnormalities and clinical symptoms (tingling or numbness of the hands and feet and muscle twitching or tremors) were important in patients in group 4. The Spanish experts were asked about treatment adherence, but not about patient adherence problems, which, according to the United Kingdom, Sweden and Portugal experts, are an important consideration in inadequately controlled hypoparathyroidism in patients in groups 2–4.13
In line with the European Society of Endocrinology guidelines, which state that clinical chemistry parameters should be monitored and kept within their reference ranges and that patients should be educated about the concomitant diseases and symptoms associated with their disease,12 a consensus was reached on the maintenance of several clinical chemistry parameters, the need for personalised care and the need for education about symptoms and complications.
The European Society of Endocrinology guidelines also recommend offering treatment to asymptomatic patients with chronic hypoparathyroidism to see whether their wellness can be improved, as symptoms of hypocalcaemia are not directly reflected in calcium levels.12 However, the experts agreed that treatment of asymptomatic patients with calcium levels at the lower limit of normal would be unnecessary, as their quality of life would not be likely to be affected.
The expert group did not reach a consensus on the type of medication that constitutes conventional treatment. In the case of vitamin D supplements, this can be attributed in part to the fact that some experts interpreted the statement as referring to the administration of vitamin D in the absence of oral calcium. In the case of the use of thiazide diuretics or a low-sodium diet to control hypercalciuria, the lack of consensus was mainly determined by the risks involved in such treatment.
The lack of consensus on the statement about the use of vitamin D in the treatment of the disease could reflect country-specific clinical considerations and the fact that dose adjustment should depend on blood levels of vitamin D. In Spain, the forms (and doses) of vitamin D prescribed may differ from those used in certain other parts of Europe, although the general clinical practice patterns in the treatment of hypoparathyroidism in Spain are similar to those applied in other parts of Europe.
This analysis has a number of limitations that must be taken into account. As this study was limited to Spain, its findings may not apply to non-Spanish patients, limiting the extent to which they might be generalised to an international population. Although a broad spectrum of endocrinologists from different regions treating patients with chronic hypoparathyroidism were invited to take part, not all experts completed the two rounds and, given the subjective selection of the experts, there could be a potential for bias. The use of open questions in the questionnaire could have introduced a certain bias into the interpretation of the results. Lastly, this study was based on expert opinion, but even a consensus based on expert opinion carries subjective bias and ranks low in the hierarchy of clinical evidence.17,18
Regardless of these limitations, the Delphi technique is a well-established method for generating consensus and accommodates the opinions of different experts on different issues.15 One advantage of this Spanish expert panel is that, unlike most Delphi groups, the number of experts making contributions was high because Spain has a large number of centres treating patients with hypoparathyroidism. These data could therefore be considered representative of Spanish endocrinologists.
We believe that our findings may have significant clinical repercussions for the treatment of patients with chronic hypoparathyroidism and that they will be helpful in raising awareness of important parameters of the disease associated with the inability to adequately control it.
ConclusionsA consensus was reached among the Spanish physicians who formed this Delphi group on the elements that are important for assessing patients and on which disease parameters are essential for characterising hypoparathyroidism not adequately controlled with conventional treatment. The expert group recognised that clinical symptoms and complications affect patients’ quality of life regardless of their clinical chemistry values. They also recognised the need for personalised treatment and education about symptoms and complications.
FundingThis work was funded by Shire Internacional GmbH, Zug, Switzerland, a member of the Takeda group of companies, and Shire Pharmaceuticals Ibérica SL, Madrid, Spain, a Takeda company.
Authorship/collaboratorsAll the authors cited met the criteria for authorship of the International Committee of Medical Journal Editors (ICMJE) in relation to this article, had full access to all data in this study, assume responsibility for the integrity of the study as a whole and have granted their approval to publish this version.
Conflicts of interestAll the authors were employees of Shire Pharmaceuticals Ibérica SL (Madrid, Spain, a member of the Takeda group of companies) at the time when this study was conducted. Juan Vila and Elena Burillo Ipiens are currently employees of Sobi SL, Spain.
We would like to thank the members of the Delphi expert panel. Under the direction of the authors, Afia Akram, PhD, an employee of ICON (North Wales, PA, United States), provided editorial assistance, funded by Shire International GmbH, a Takeda group company.
Please cite this article as: Burillo E, Vila J, Oguiza A. Características de los pacientes con hipoparatiroidismo crónico no adecuadamente controlado con el tratamiento convencional y patrones del manejo en España. Endocrinol Diabetes Nutr. 2021;68:304–311.