The CADIT-CAM study was designed to retrospectively analyze the clinical characteristics, treatments, and outcomes of patients with differentiated thyroid carcinoma (DTC) in Castilla La Mancha.
Patients and methodsA total of 1434 patients from 7 hospitals in Castilla La Mancha were enrolled into the study from 2001 to 2015.
ResultsSeventy-seven percent of patients were female, with a mean age at diagnosis of 48 years. Papillary thyroid carcinoma accounted for 93% of cases. Mean tumor size was significantly smaller at final follow-up (p<0.05). Radioiodine ablation (RA) was performed in 84% of patients, and its use decreased during the study, especially in tumors with low recurrence risk. Recurrence occurred in 22% of patients and was associated to male gender, greater tumor size, multifocality, lymph node metastases, extrathyroid involvement, distant metastases and increasing thyroglobulin antibody titers. At the end of follow-up 76.2% of patients were alive and free of disease, 2.4% had died from DTC. Overall survival of the cohort was 95.1% at 15 years of follow-up.
ConclusionsCharacteristics of DTC in this Spanish cohort are similar to those reported in other studies in our country. Final results were excellent and use of treatment (RA) was consistent with risk-stratified recommendations.
El estudio CADIT-CAM es un estudio retrospectivo diseñado para analizar las características clínicas, el tratamiento y los resultados finales de los pacientes con cáncer diferenciado de tiroides (CDT) en Castilla-La Mancha.
Pacientes y métodosSe ha incluido a 1.434 pacientes diagnosticados en 7 hospitales castellano-manchegos, entre 2001 y 2015.
ResultadosEl 77% eran mujeres, con una edad media al diagnóstico de 48 años, y el tipo histológico principal fue carcinoma papilar en el 93%. El tamaño el tumor fue descendiendo de forma significativa a lo largo de los 15 años (p<0,05). El tratamiento con radioyodo se ha utilizado en el 84% de la serie, habiendo disminuido su utilización a lo largo del estudio, sobre todo en los de bajo riesgo de recurrencia. Existió recurrencia en el 22% de los pacientes, siendo los factores relacionados con la misma: sexo masculino, mayor tamaño tumoral, multifocalidad, presencia de metástasis linfáticas o a distancia o de afectación extratiroidea así como la presencia de anticuerpos antitiroglobulina con evolución desfavorable. Al final del seguimiento, el 76,2% de los casos estaban libres de enfermedad y el 2,4% de los pacientes habían fallecido por CDT, siendo la supervivencia global de la cohorte del 95,1% a los 15 años de seguimiento.
ConclusionesLas características del CDT de la cohorte de Castilla-La Mancha son similares a las de otras series españolas. Los resultados finales son excelentes y las tendencias del tratamiento se han ido adaptando al riesgo de recurrencia de los pacientes.
Thyroid carcinoma is the most common endocrine neoplasm and comprises a number of different tumour types characterized by variable clinical behaviour and prognoses. Tumours originating from the thyroid follicular cells account for over 90% of these neoplasms and are known as differentiated thyroid carcinoma (DTC). Although DTC is not a frequent neoplasm, it accounts for 3% of all tumours in females and 1% in males. Its incidence has increased exponentially in recent decades, particularly in developed countries,1–3 and Spain has been no exception to this worldwide increase. Based on different methods, studies in Galicia,4 Murcia5 and Navarre6 have demonstrated a sustained increase in the incidence of DTC since the 1980s. In Spain, thyroid cancer ranks second as the malignancy with the most favourable prognosis, the overall 5-year survival rate in adults being 87.4%, with better figures in women (89.8%) than in men (78.3%).7 The above data suggest an immediate future characterized by a significant and growing number of patients with thyroid cancer, who moreover will need adequate management.
The great advances in our knowledge of thyroid cancer have led to changes in the approach to the management of the disease, as reflected in the new guidelines published in recent years.8,9 However, many clinical, diagnostic and therapeutic aspects of DTC continue to generate controversy and require us to continuously improve and unify the patient management protocols. Awareness of the current situation in this field may help us in planning future strategies at both the clinical – healthcare level and in research.
A number of Spanish national series have already been published, describing the characteristics and outcomes of patients treated for DTC in certain areas10–13 and regions of the country.6,14,15
In order to further our understanding of the clinical reality of patients with thyroid cancer, the Society of Endocrinology, Nutrition and Diabetes of Castilla-La Mancha (Sociedad Castellano Manchega de Endocrinología Nutrición y Diabetes [SCAMEND]) decided to conduct a retrospective study to assess the profile of DTC in our geographical setting. The CADIT-CAM study on differentiated thyroid carcinoma in Castilla-La Mancha was designed to evaluate the characteristics, treatments and clinical outcomes of patients diagnosed with DTC over a 15-year period between 2001 and 2015 in the Autonomous Community of Castilla-La Mancha.
Patients and methodsA retrospective study was made of patients with DTC (derived from the follicular epithelium: primary histological type either papillary or follicular) diagnosed or operated upon between 1 January 2001 and 31 December 2015 in any of the healthcare areas of Castilla-La Mancha. We included patients diagnosed and followed-up on at 7 reference hospitals of the 8 healthcare areas of this Autonomous Community (Complejo Hospitalario Universitario de Albacete, Hospital General Universitario de Ciudad Real, Hospital Virgen de la Luz de Cuenca, Hospital Universitario de Guadalajara, Hospital General Mancha-Centro de Alcázar de San Juan, Hospital Nuestra Señora del Prado de Talavera de la Reina and Complejo Hospitalario de Toledo). These hospitals cover over 95% of the population in the region. The data were collected or updated during 2017.
The following variables were analyzed:
- 1.
Demographic characteristics: gender, date of birth.
- 2.
Tumour-related characteristics at diagnosis: the date of diagnosis was defined as the date of surgery or the date of fine needle aspiration biopsy (FNAB) of the suspected nodule in patients not undergoing surgery.
- 3.
Initial treatment provided: the type of thyroid surgery (total thyroidectomy, subtotal thyroidectomy, two-stage total thyroidectomy), lymphadenectomy, and radioiodine treatment (initial activity, number of doses used, and total activity administered).
- 4.
Baseline pathological characteristics: the primary histological type (papillary or follicular), the histological subtype, tumour size, the presence or absence of multifocality, lymph node involvement and its extent, extrathyroid spread and its extent, and the presence of distant metastases at diagnosis.
- 5.
The probability of survival was classified using the American Joint Committee on Cancer (AJCC)-TNM 7th edition criteria, and was stratified by the risk of recurrence based on the American Thyroid Association (ATA) guidelines of 2009.16
- 6.
Recurrence/persistence: disease recurrence or persistence was evaluated throughout the patient follow-up period. Recurrence was considered to have occurred if the patient presented active disease after a period of healing, while persistence was considered to have occurred if the absence of disease could not be confirmed at any time after the initial treatment or successive treatments.
- 7.
The following possibilities were taken into consideration when the final status or outcome of the patients was being assessed: the absence of disease in patients with no clinical, biochemical or structural evidence of DTC based on the dynamic stratification criteria proposed by the ATA 20158; and persistent disease in patients with persistent biochemical (including indeterminate response) and structural disease. In patients not treated with radioiodine, we used the criteria proposed by Momesso et al.17 “Lost to follow-up” was also considered as a final status or outcome if the initially diagnosed and treated patient did not continue active follow-up to the end of the study period, in the same way as “death”. In the case of death we considered two possibilities: death due to DTC and death due to other causes. In order to calculate follow-up time, we recorded the date of death and the date of loss to follow-up.
- 8.
Other aspects assessed in the study were:
- a.
Thyroglobulin antibodies: the investigators were asked to classify the patients according to the presence of thyroglobulin antibodies analyzed in each hospital using the usual analytical method. Three qualitative categories were established: negative antibodies, positive antibodies with a favourable course (i.e., decrease or negative conversion), and positive antibodies with an unfavourable course (persistently high or increasingly positive antibody titres).
- b.
Treatment in the context of recurrence: in patients with persistent/recurrent disease, the treatment decided in this situation was recorded (surgery, radioiodine, radiotherapy, tyrosine kinase inhibitors, etc.).
Only those patients with over 90% of the study variables were analyzed and included.
Results were expressed as the mean±standard deviation (SD) for quantitative variables and as proportions for qualitative variables. The Student t-test and analysis of variance (ANOVA) were used to compare quantitative variables. The chi-squared test was used to compare qualitative variables. The factors associated with recurrence were investigated using binary logistic regression analysis. Differentiated thyroid carcinoma-specific survival was estimated using the Kaplan–Meier method. The factors relating to survival were analyzed by univariate (log-rank test) and multivariate analyses (Cox proportional hazards model). Statistical significance was considered for p<0.05. The SPSS version 22.0 statistical package (IBM Corp.) was used throughout.
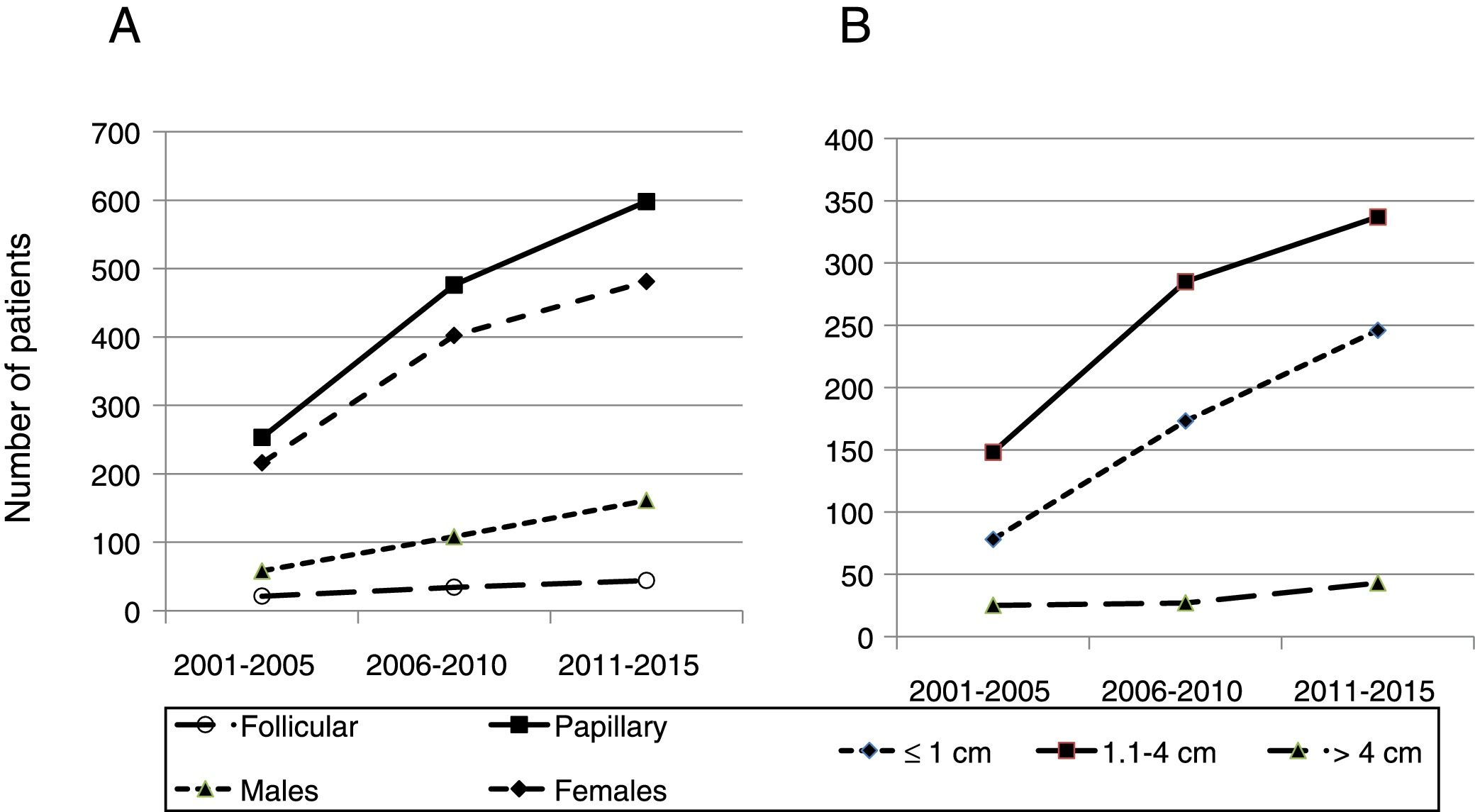
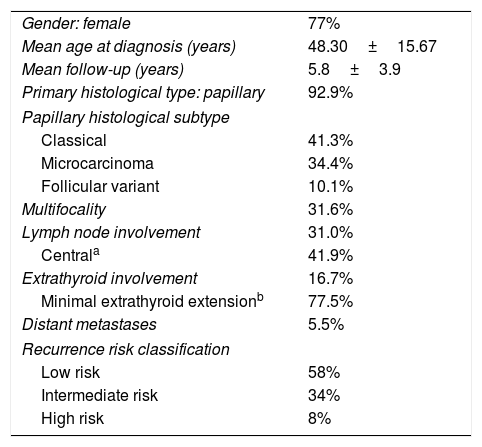
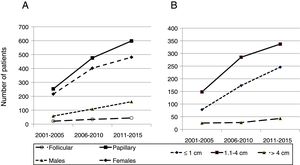
ResultsA total of 1434 patients with DTC were included in the study. Their baseline demographic and histological characteristics are shown in Table 1; no significant differences were observed between the different hospitals. In the course of the study period, an increase was seen in the number of cases of DTC diagnosed in both males and females, particularly at the expense of papillary carcinoma. The frequency of follicular carcinoma remained stable by comparison (Fig. 1A).
Demographic and initial presentation characteristics of the cohort of patients with DTC in Castilla-La Mancha.
| Gender: female | 77% |
| Mean age at diagnosis (years) | 48.30±15.67 |
| Mean follow-up (years) | 5.8±3.9 |
| Primary histological type: papillary | 92.9% |
| Papillary histological subtype | |
| Classical | 41.3% |
| Microcarcinoma | 34.4% |
| Follicular variant | 10.1% |
| Multifocality | 31.6% |
| Lymph node involvement | 31.0% |
| Centrala | 41.9% |
| Extrathyroid involvement | 16.7% |
| Minimal extrathyroid extensionb | 77.5% |
| Distant metastases | 5.5% |
| Recurrence risk classification | |
| Low risk | 58% |
| Intermediate risk | 34% |
| High risk | 8% |
Quantitative variables are reported as the mean±standard deviation (SD).
Number of patients diagnosed by 5-year intervals according to histological type, gender and tumour size. (A) Number of patients diagnosed according to primary histological type and gender. (B) Number of patients diagnosed in each 5-year interval according to tumour size. Microcarcinomas (tumours≤1cm) were the group that increased significantly (p<0.05) over the study period.
In the study cohort, tumour size decreased significantly during the study period: the mean tumour size in 2001 was 21.5±14.5mm versus 15.1±13.0mm in 2015 (p<0.05). Likewise, a significant increase was recorded (p<0.05) in the number of microcarcinomas diagnosed over the 15-year period (Fig. 1B). The number of patients with tumours measuring between 1 and 4cm in size increased during the study period, though not significantly so. The number of tumours greater than 4cm in size remained stable. Patient age at diagnosis increased significantly, from 47.1±17.1 years at the start to 51.9±15.6 years in 2015, (the last year of data collection) (p<0.05).
Over 50% of our patients were initially classified as being at low risk of recurrence. Less than 10% of the initial cohort met high risk criteria, mostly due to the presence of distant metastases at diagnosis (Table 1).
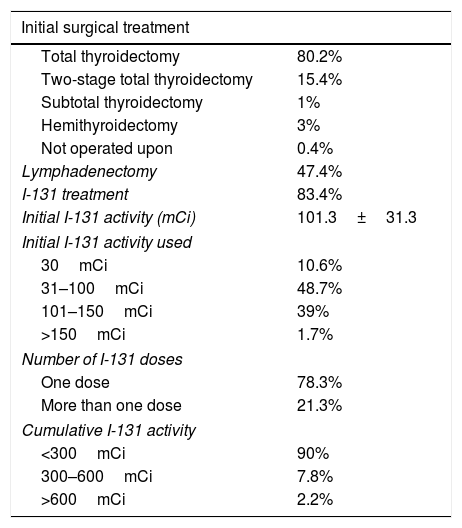
Table 2 shows the results of the initial treatment provided to the study cohort. The most commonly used initial treatment was total or near total thyroidectomy in over 80% of the cases. Hemithyroidectomy was performed in 3% of the series, with a tendency to increase in the course of the study period (2.4% in 2001 versus 6.9% in 2015) (p=ns). By contrast, totalizing or two-stage thyroidectomy was less frequently performed (24% in 2001 versus 11.2% in 2015) (p<0.01).
Results of treatment in the DTC cohort of Castilla-La Mancha.
| Initial surgical treatment | |
|---|---|
| Total thyroidectomy | 80.2% |
| Two-stage total thyroidectomy | 15.4% |
| Subtotal thyroidectomy | 1% |
| Hemithyroidectomy | 3% |
| Not operated upon | 0.4% |
| Lymphadenectomy | 47.4% |
| I-131 treatment | 83.4% |
| Initial I-131 activity (mCi) | 101.3±31.3 |
| Initial I-131 activity used | |
| 30mCi | 10.6% |
| 31–100mCi | 48.7% |
| 101–150mCi | 39% |
| >150mCi | 1.7% |
| Number of I-131 doses | |
| One dose | 78.3% |
| More than one dose | 21.3% |
| Cumulative I-131 activity | |
| <300mCi | 90% |
| 300–600mCi | 7.8% |
| >600mCi | 2.2% |
Quantitative variables were reported as the mean±standard deviation (SD).
I-131: radioiodine.
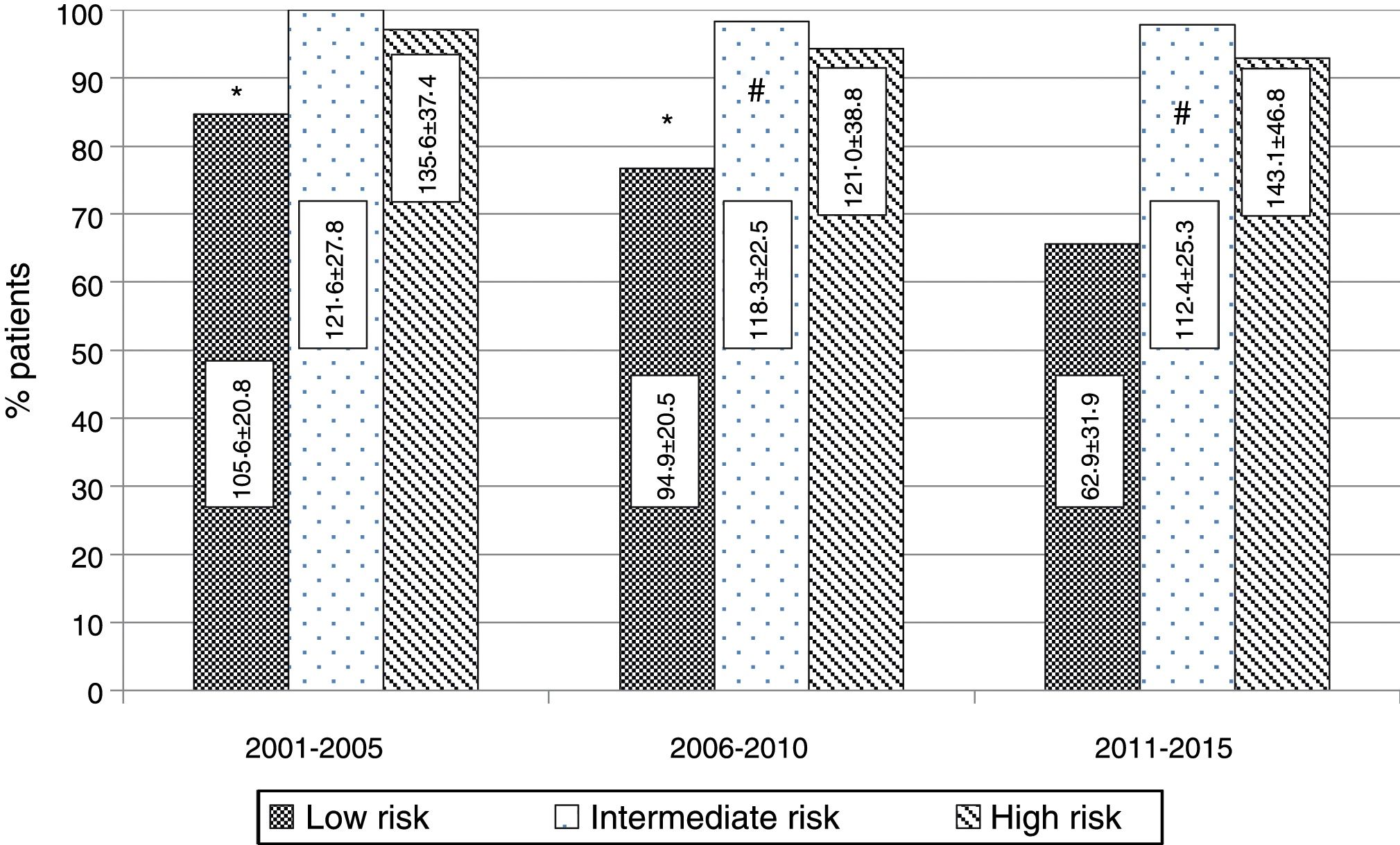
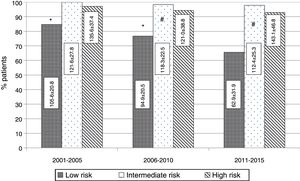
Most of the patients (83.4%) in the cohort received radioiodine therapy after initial surgery. The activity initially used, the number of doses, and the cumulative activity is reported in Table 2. An initial activity of 30mCi used in 10.6% of the patients was decided in patients at a low risk of recurrence in the last 5 years of the study (2011–2015). This activity level had not been used as the initial treatment in the previous years. Over the 15 years of the study, a progressive decrease was observed in the number of patients receiving radioiodine (95.1% in 2001 versus 74.1% in 2015; p<0.01) and in the initial mean activity used (113.5±25.6mCi versus 84.8±47.5mCi; p<0.01). This decrease mainly occurred at the expense of the low-risk patients. Fig. 2 shows the radioiodine doses used according to 5-year intervals in each of the recurrence risk categories.
Radioiodine treatment according to risk categories by 5-year intervals in patients with DTC in the Castilla-La Mancha cohort. The figure shows the percentages of patients receiving at least one radioiodine dose in each recurrence risk category (p<0.01). The mean activities used in each risk category and by 5-year interval are indicated. Statistically significant differences were found in the low-risk (*p<0.01) and intermediate-risk patients (**p<0.05). There were no differences in the high-risk patients.
A total of 409 patients (29.6%) had positive thyroglobulin antibody titres among the 1381 individuals for which this laboratory test parameter was available. The majority of antibody-positive DTCs (84.3%) showed a favourable response.
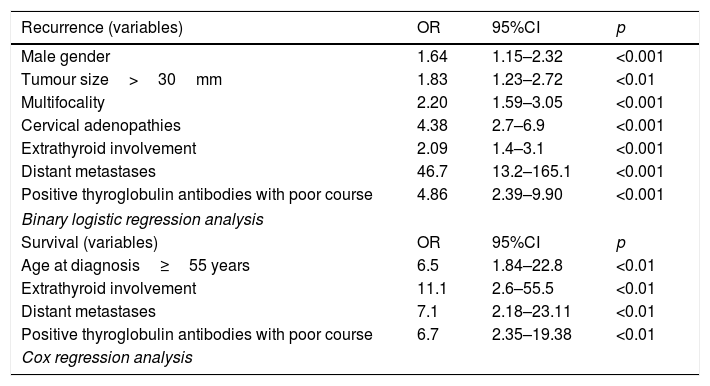
During the study period, 326 patients presented disease recurrence or persistence, representing 22.7% of the study cohort. In the low-risk category 9.0% of the patients suffered recurrence, compared with 33% and 82% in the intermediate- and high-risk categories, respectively (p<0.01). Table 3 shows the factors independently associated with disease recurrence/persistence in the study cohort. Radioiodine treatment was the most commonly used initial therapy for recurrence (57.5%), followed by surgery (32.2%). In cases with advanced DTC and persistent disease, external radiotherapy was used in a small percentage of cases (1.65%). Tyrosine kinase inhibitors were used in 1.4% of the patients, and of these, most were initially at high risk and with no response to other treatments.
Factors independently related to recurrence/persistence and survival in the DTC cohort of Castilla-La Mancha.
| Recurrence (variables) | OR | 95%CI | p |
|---|---|---|---|
| Male gender | 1.64 | 1.15–2.32 | <0.001 |
| Tumour size>30mm | 1.83 | 1.23–2.72 | <0.01 |
| Multifocality | 2.20 | 1.59–3.05 | <0.001 |
| Cervical adenopathies | 4.38 | 2.7–6.9 | <0.001 |
| Extrathyroid involvement | 2.09 | 1.4–3.1 | <0.001 |
| Distant metastases | 46.7 | 13.2–165.1 | <0.001 |
| Positive thyroglobulin antibodies with poor course | 4.86 | 2.39–9.90 | <0.001 |
| Binary logistic regression analysis | |||
| Survival (variables) | OR | 95%CI | p |
| Age at diagnosis≥55 years | 6.5 | 1.84–22.8 | <0.01 |
| Extrathyroid involvement | 11.1 | 2.6–55.5 | <0.01 |
| Distant metastases | 7.1 | 2.18–23.11 | <0.01 |
| Positive thyroglobulin antibodies with poor course | 6.7 | 2.35–19.38 | <0.01 |
| Cox regression analysis | |||
95%CI: 95% confidence interval; OR: odds ratio.
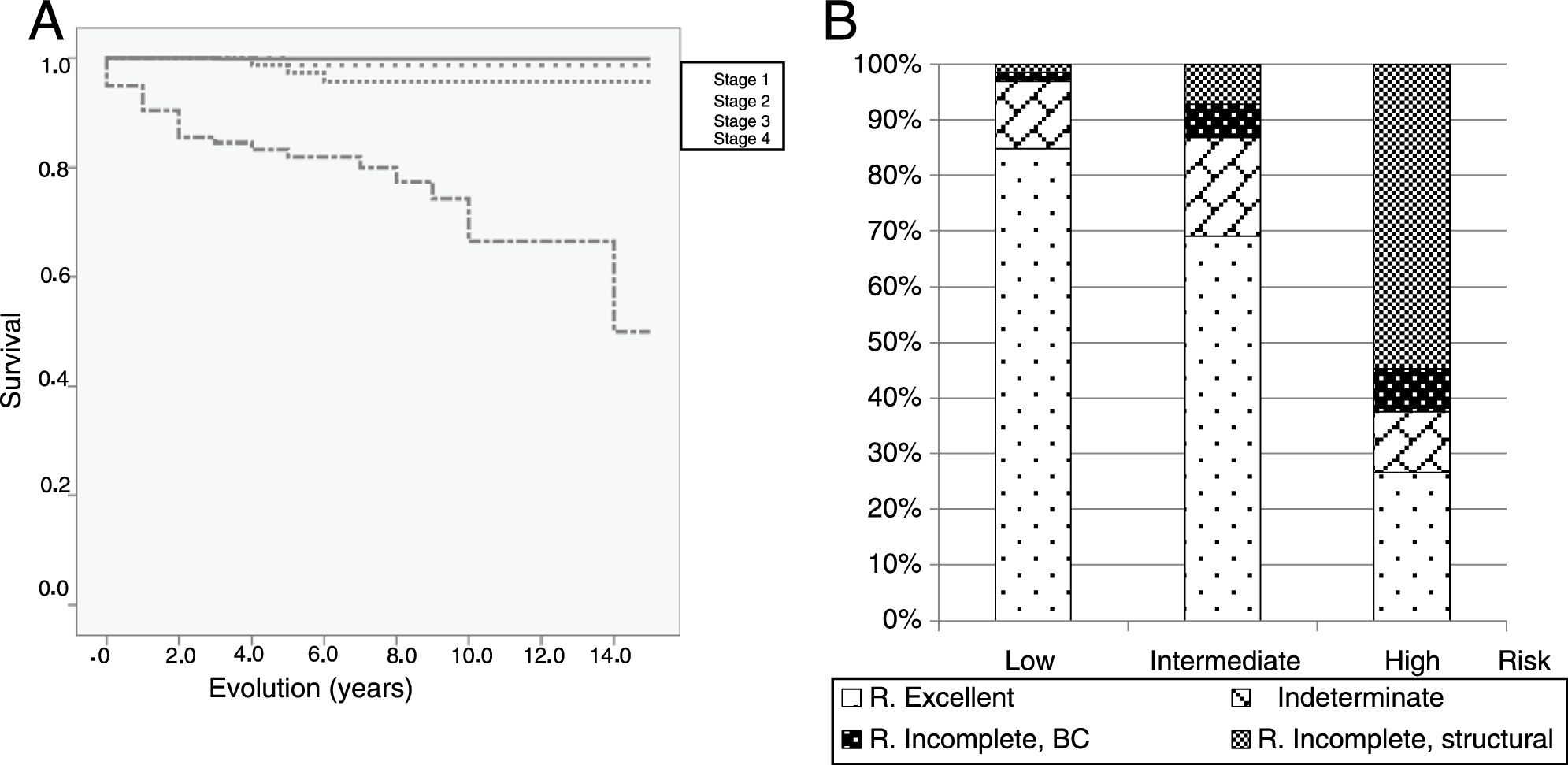
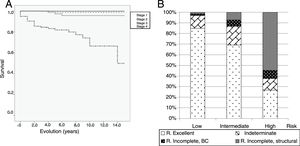
The DTC-specific survival of the series after 15 years of follow-up was 95.1%. Fig. 3A shows the probability of thyroid cancer survival according to the AJCC-TNM 7th edition criteria; 75 patients with DTC died in the period studied, 34 of them as a consequence of the thyroid tumour process (2.4%). Data referring to final clinical outcome were available for a total of 1218 patients; 76.2% were disease-free and the remaining 23.8% continued to have active disease (14% indeterminate response, 3.4% incomplete biochemical response, and 6.4% incomplete structural response). Fig. 3B shows the final disease status stratified according to the initial recurrence risk. The percentage of patients with an excellent response proved statistically different for each of the initial risk categories (84.5% low risk, 69% intermediate risk and 26.6% high risk) (p<0.001). Most of the patients with an indeterminate response were subjects with positive thyroglobulin antibodies and decreasing or stable titres. At the end of follow-up this implied favourable clinical response rates of over 95% in the low-risk patients and of over 85% in the intermediate-risk patients. The presence of persistent structural disease reached 54.7% in the high-risk patients versus only 1.5% in the low-risk subjects.
Differentiated thyroid carcinoma-specific survival plot and final clinical outcomes in the cohort of patients in Castilla-La Mancha. (A) Specific survival (Kaplan–Meier) is represented by AJCC 7th edition stages, showing a significant difference between the different stages (p<0.01). (B) Final outcome of the patients according to initial recurrence risk category. The dynamic stratification criteria have been used. The percentage of patients with an excellent response was statistically different for each of the baseline risk categories (p<0.01).
The present retrospective study reviewed the most relevant clinical characteristics, the treatments used and the final outcomes in a large cohort of patients diagnosed with DTC between 2001 and 2015 in the Autonomous Community of Castilla-La Mancha (Spain). The results show a population with characteristics similar to those of other Spanish national10–15 and international series,18–20 with a clear female predominance; patients diagnosed in middle age; a predominance of the papillary histological type; and excellent final outcome and survival data.
The figures referring to the incidence of thyroid cancer in our Autonomous Community supplied by the population cancer registries of the provinces of Albacete, Cuenca and Ciudad Real, are lower than the Spanish national average, with an adjusted annual incidence of 5.7 cases per 100,000 inhabitants for both genders in 2011.21 The retrospective data in our cohort are not findings from which epidemiological conclusions can be drawn, though they indicate a significant increase in the number of cases diagnosed over the 15 years of the patient registry. This increase has occurred in both women and men, and at the expense of the papillary histological type. In Spain, the studies published on the incidence of DTC in Galicia, Murcia or Navarre4–6 all confirm the existence of an increasing incidence over more than three decades in the same groups of patients (both genders and papillary carcinoma).
The exponential increase in the incidence of DTC observed in most developed countries may be related to overdiagnosis, among other factors.2 The use of different and increasingly sophisticated imaging techniques accessible to a population22 demanding greater healthcare undoubtedly facilitates the diagnosis of small and possibly nonlethal lesions, which in past decades would not have become diagnostic or treatment problems. Despite the limitations of the study, some of our findings, such as the exponential increase in microcarcinomas and the significant decrease in tumour size over the study period, suggest that improvements in diagnostic procedures and histopathological study criteria may have contributed to an increase in the number of patients with incidental lesions in Castilla-La Mancha.
On the other hand, it is not possible to discard the existence of other potential factors that may be contributing to an increase in thyroid cell carcinogenesis (ionizing radiation, nuclear medicine or diagnostic procedures, still unidentified environmental carcinogens, etc.), and which could explain the increase in larger tumours described in some series.4,23 In our study, the percentages of tumours measuring 1–4cm in size and larger lesions (>4cm) remained stable during the data collection interval, though in absolute terms the number of patients with tumours between 1 and 4cm in size also experienced a significant increase.
The clinical guides published in recent years8,9,16 were developed to facilitate the best clinical and therapeutic decisions, based on scientific evidence, with the primary aim of minimizing the potential damage of overtreatment in a majority of patients at low risk of mortality, and of individualizing treatment in patients with high-risk DTC. In general, the most recent guides reflect a clear preference for more conservative management both in relation to surgery and the use of radioiodine. In some already published series, the final outcomes in patients with DTC treated according to the evidence-based international guidelines are better than the outcomes before such guidelines were implemented in clinical practice.24 In Italy, a recent retrospective study25 attempted to assess how publication of the 2009 ATA guidelines16 has modified the clinical practice of Italian endocrinologists in patients with DTC. Our results are consistent with those of the Italian study, which reflect few changes in surgical treatment. Most of the patients in our cohort underwent total or intentionally total thyroidectomy, regardless of the baseline clinical characteristics. Although we found a greater use of hemithyroidectomy as initial treatment, this technique remains a minority surgical option, and possibly reflects a lesser indication of totalized thyroidectomy when the final pathology report diagnoses incidental carcinoma. However, with regard to treatment with radioactive iodine, we confirmed a lesser use, particularly from 2010 onwards, and especially in low-risk patients. This would suggest that the use of this treatment modality is adapted to the recurrence risk category in Castilla-La Mancha.26,27 Lamartina et al.25 reported radioiodine to be used between 2013 and 2016 in 41.2% of low-risk patients, 87.1% of intermediate-risk patients and 93.1% of high-risk patients. Likewise, the radioiodine activity administered to low-risk patients was significantly lower than in high- and intermediate-risk patients in both the Italian study and in our own series. In a recent study, the use of low doses of radioactive iodine in low-risk patients followed-up on in hospitals in Castilla-La Mancha afforded excellent results in most of these patients.28
The recurrence risk classification proposed by the ATA in its 2009 guidelines16 has consistently shown its usefulness in discriminating the higher risk population, allowing for the individualization of treatment both initially and in the immediate follow-up period after surgery. This classification uses prognostic factors that have been modified in the most recent guides8 and which are intended to indirectly reflect tumour biology. Using this stratification in our cohort, over 50% of the patients were classified as being at low risk, with a recurrence rate of 9%, this being similar to the figures reported in low risk patients from other series,18,19 though our study involved a longer clinical follow-up period. Our high-risk patients showed a very high probability of recurrence (over 80%); early identification is therefore essential for individualized management adapted to the risk posed by this type of tumour. We consider that our results validate the risk classification criteria proposed by the international guides in a large series of patients with DTC in Spain. Initial patient stratification, even in the case of tumours with an excellent prognosis a priori, is a key element in the therapeutic orientation of patients with DTC.
The overall disease recurrence/persistence rate (approximately 22%) and the related factors (gender, tumour size and tumour spread) are similar to those of other cohorts. The presence of positive thyroglobulin antibody titres with an unfavourable course is an independent factor for recurrence.29 This poor prognosis factor was not analyzed in many DTC series, and was found to be an unfavourable factor for both recurrence and survival in our series.
The survival outcomes of patients with DTC in Castilla-La Mancha are excellent, the factors associated with a poorer prognosis being patients with extensive extrathyroid involvement, distant metastatic spread, age at diagnosis >55 years, and the presence of antithyroglobulin antibody titres with an unfavourable course. With the exception of the presence of thyroid autoimmunity, these factors are consistent with those considered in the AJCC classification.30 The DTC-specific mortality rate in our cohort was low. Based on the results of our study, we cannot know whether the mortality rate has remained stable or whether it has increased because of the increase in diagnosis. However, the retrospective epidemiological data found in the registries of Castilla-La Mancha indicate that up until 2010 the annual standardized thyroid cancer mortality rate for both genders remained stable or decreased (0.8 cases per 100,000 in 2000 versus 0.5 per 100,000 in 2010).21
Most published studies on treatment response and final outcome in series of patients with DTC have been conducted in patient populations subjected to surgery and radioiodine ablation. In the data of the Castilla-La Mancha series referring to treatment response and final outcome, use was made of the dynamic stratification criteria proposed by Tuttle for patients treated with surgery and radioiodine,8,19 and the response criteria for low-risk patients subjected to thyroidectomy without radioiodine or to hemithyroidectomy.17 The excellent response percentages in the three categories were similar to those described in the ATA guide of 2015,8 which envisages percentages between 86 and 91% for low-risk patients, 57–63% for intermediate-risk patients, and 14–16% for high-risk patients. The inclusion of lower-risk patients not treated with radioiodine, prolonged patient follow-up, and the analysis of outcomes after the treatment of disease relapses may possibly have improved the final outcomes, particularly in intermediate- and high-risk patients (with excellent responses in 69% and 26.6%). The dynamic stratification criteria for assessing final outcome in our cohort reproduce the data found in other international series, and should be used on a routine basis to analyze treatment response and final outcomes in patients diagnosed with DTC.
Our study has the limitations inherent in retrospective data collection over a long period of time (2001–2015) and in different hospitals. However, a large number of patients were included from almost all hospitals in Castilla-La Mancha, and moreover we only analyzed those patients with a very high percentage of satisfactorily collected study variables. This allows us to confirm that the characteristics of our cohort were similar to those of other Spanish national series, and that in addition to the increase in the number of diagnosed cases, the final outcomes in terms of survival and healing of the disease – using the updated response and dynamic stratification criteria – were excellent. Lastly, the data obtained in our study suggest that the trends in the management approach to patients with DTC (particularly as regards radioiodine treatment) are changing in concordance with the latest international recommendations.
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to the present study.
Complejo Hospitalario Universitario de Albacete: J.J. Alfaro, C. Lamas, F. Botella, C. Gonzalvo, A. Hernández, L.M. López, L. García, P. Pinés, R. Quílez. Hospital Virgen de la Luz, Cuenca: M. Alramadán, D. Martín, D. Calderón, J. Pérez Rodríguez, F. Jiménez. Hospital Universitario de Guadalajara: S. Herranz. Hospital General de Ciudad Real: M. Aguirre, P. Gómez, J. Moreno. Complejo Hospitalario Mancha Centro, Alcázar de San Juan: A. García-Manzanares, I. Gómez, J. Silva, F. del Val. Hospital Nuestra Señora del Prado, Talavera de la Reina: B. Blanco, P. de Diego, M.G. Llaro, D. Ariadel. Complejo Hospitalario de Toledo: E. Castro, I. Luque, E. Maqueda, A. Marco, A. Martínez, A. Vicente, M.A. Carrasco, J. López.
Please cite this article as: Sastre Marcos J, Aznar S, Álvarez V, Torres B, Delgado M, González J, et al. Resultados del seguimiento de pacientes con carcinoma diferenciado de tiroides en Castilla-La Mancha (2001–2015). Estudio CADIT-CAM. Endocrinol Diabetes Nutr. 2019;66:164–172.