Secondary hyperparathyroidism (SHPT) affects approximately 100% of patients on a dialysis program. Almost 90% are controlled with conservative treatment, while the rest require more aggressive treatment for control. Surgery has traditionally been the treatment of choice for these difficult to control cases.1,2 Since 2005, when the calcimimetic cinacalcet was approved by the European Medicines Agency, therapeutic management of SHPT has gradually changed. Cinacalcet has progressively become the first treatment option for patients with difficult to control SHPT. There is however little information as to whether this has had a real long term impact on the need for surgery in patients with difficult to control SHPT.3–5 The study objective was to analyze the impact of cinacalcet on surgery for SHPT at our hospital after 10 years of use.
The study population consisted of patients with chronic kidney failure on a dialysis program who had undergone surgery for SHPT from January 1995 to December 2014. Patients with prior thyroid and/or parathyroid surgery, and those diagnosed with multiple endocrine neoplasia syndrome, were excluded For data analysis, two periods were distinguished based on the date of introduction of cinacalcet at our hospital: 1) pre-cinacalcet period: 1995 to 2004; and 2) post-cinacalcet period: 2005–2014. Epidemiological, clinical, therapeutic, and evolutionary variables were analyzed. SHPT persistence was defined as absence of a decrease greater than 50% from preoperative PTH levels within six months of surgery. Relapse or recurrence was defined as a PTH increase above 250pg/mL after the six months following surgery. Statistical analysis was performed with SPSS v.15.0 for Windows, using Chi-square, Fisher exact, Student's t, and Mann–Whitney U tests.
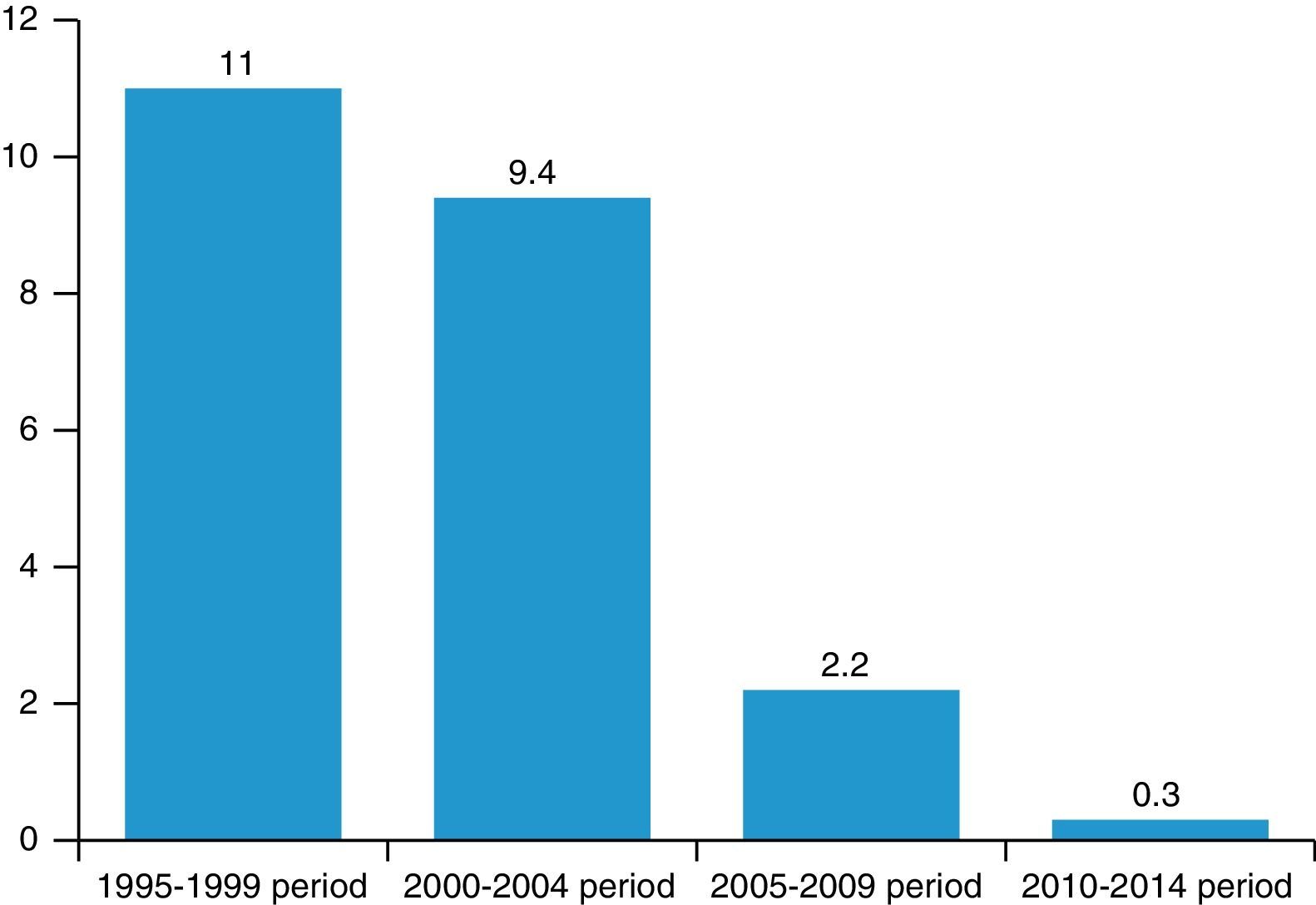
During the study period, 76 patients with SHPT refractory to conservative management underwent surgery. Mean patient age was 51±14.4 years, and there were 57.9% (n=44) male patients. Ninety-three percent of patients underwent surgery in the pre-cinacalcet period, and the remaining 7% (n=5) after introduction of the calcimimetic as treatment for SHPT (p<0.001). Of all patients on dialysis, 10.1% by year underwent surgery for HPT in the pre-cinacalcet period, as compared to 1.3% in the post-cinacalcet period (p<0.001). As shown in Fig. 1, such decrease was more pronounced as time elapsed since introduction of cinacalcet and patients were treated earlier. Thus, 2.2% of patients on dialysis underwent surgery for SHPT in the 2005–2009 period, as compared to 0.3% in the 2010–2014 period. Comparison of patients in the pre-cinacalcet versus the post-cinacalcet era showed no differences in any of the variables analyzed, except for laboratory values. Thus, patients who underwent surgery in the pre-cinacalcet period had higher values of calcium-phosphorus product (70.4 vs 51.9; p=0.002) and serum phosphorus levels (6.6 vs 5.3mg/dL; p=0.035). The surgical procedure performed in all patients was subtotal parathyroidectomy. There were three recurrences (3.9%) of SHPT, all in the pre-cinacalcet group.
After approval of cinacalcet, the number of indications of parathyroidectomy has markedly decreased. Cinacalcet provides a better control of SPHT than the drugs previously used, as shown by our study. After introduction of cinacalcet, there was a highly significant decrease in the number of surgical procedures for SHPT at our hospital from 10.1% to 1.3% by year in patients on dialysis. Moreover, in the last study period, from 2010 to 2014, the proportion has decreased to 0.3% by year in patients on dialysis. It should be noted that Spain has one of the highest kidney transplant rates worldwide, and during the study period there has been a progressive increase in the number of kidney transplants,6 a factor which also decreases the surgery rate in SHPT, because it allows for early transplant in these patients without prior parathyroidectomy.
Today, parathyroidectomy is only performed in SHPT in cases difficult to control after treatment with cinacalcet (severe hypercalcemia, calciphylaxis and/or PTH levels higher than 500pg/mL) or in patients with associated complications such as tendon rupture, severe bone pain, or refractory anemia. Surgery should be performed at experienced endocrine departments.7–9
In conclusion, cinacalcet has had a direct impact on control of SHPT, resulting in a highly significant decrease in the need for surgery of hyperparathyroidism in patients with chronic kidney failure on dialysis.
Please cite this article as: Ruiz J, Ríos A, Rodríguez JM, Llorente S, Hernández AM, Parrilla P. Impacto de los calcimiméticos en la cirugía del hiperparatiroidismo secundario. Endocrinol Diabetes Nutr. 2017;64:59–61.