There is controversy regarding the performance of preoperative laryngoscopy (LP) in thyroid surgery, with different recommendations being made, based on observational studies, in various publications.
The aim of the study was to know the prevalence of laryngeal paralysis found in the LPs of patients who underwent thyroidectomy in benign and malignant pathology.
A systematic review was carried out with 29 articles included for the qualitative study and a meta-analysis of 13 articles in which the data could be obtained to evaluate the same effect (in all patients in which an LP was carried out, those with preoperative laryngeal paralysis were included, and assigned to malignant or benign postoperative histology groups).
The pooled prevalence of preoperative paralysis in benign pathology was 1.1% (95% CI 0.7 to 1.7%, 71% I2) and in 6.3% malignant pathology (95% CI 3.8 to 9.4%; I2 85%). The prevalence was significantly higher among patients with malignant pathology with an estimated effect RR 5.66, 95% CI [2.48, 12.88].
The studies analyzed present biases that will need to be corrected in future research, eliminating blinding biases in the selection and allocation of patients or in the laryngoscopy technique used. The LP in thyroid surgery evaluates possible disorders of laryngeal motility. The prevalence of laryngeal paralysis in thyroid pathology found in LPs in patients with a postoperative diagnosis of malignant pathology was higher than in the benign pathology group. This information is necessary for interpreting the intraoperative neuromonitoring signal and for making informed decisions.
Hay controversia sobre la realización de laringoscopia preoperatoria (LP) en cirugía de tiroides. Las recomendaciones, basadas en estudios observacionales, varían entre unas publicaciones y otras.
El objetivo del estudio es conocer la prevalencia de parálisis laríngea hallada en LP de pacientes a los que se realizó tiroidectomía en patología benigna y maligna.
Se realizó la revisión sistemática con 29 artículos incluidos para el estudio cualitativo y la metanálisis de 13 artículos en los que pudieron obtenerse los datos para evaluar el mismo efecto (LP realizada en todos los pacientes incluidos, se recogen los pacientes con parálisis laríngea preoperatoria, figura el número total de pacientes y pueden asignarse las parálisis preoperatorias a los grupos de histología posoperatoria maligna o benigna).*
La prevalencia agrupada de parálisis preoperatoria en patología benigna fue 1,1% (IC95% 0,7 a 1,7%; I2 71%) y en patología maligna 6,3% (IC95% 3,8 a 9,4%; I2 85%). La prevalencia es significativamente superior entre pacientes con patología maligna con un efecto estimado RR 5.66, IC 95% [2,48, 12,88].
Los estudios analizados presentan sesgos que será necesario corregir en investigaciones futuras, eliminando los sesgos de cegamiento en la selección y asignación de pacientes o en la técnica de laringoscopia empleada. La LP en cirugía de tiroides evalúa posibles trastornos de motilidad laríngea. La prevalencia de la parálisis laríngea en patología de tiroides hallada en la LP en pacientes con diagnóstico posoperatorio de patología maligna es más elevada que en el grupo de patología benigna. Esta información es necesaria para interpretar la señal de neuromonitorización intraoperatoria y tomar decisiones.
The routine use of preoperative laryngoscopy in thyroid surgery (PLTS) is subject to controversy. The recommendations, based on observational studies, vary among the different publications.
Some groups recommend selective PLTS in patients at increased risk1–4 (a history of neck surgery having placed the recurrent laryngeal nerve [RLN] or vagus nerve at risk, a history of external neck irradiation, suspected malignant thyroid disease, or a history of voice changes). Cost criteria have also been cited, indicating that routine flexible fiberoptic laryngoscopy is not cost-effective in asymptomatic patients with ultrasound low risk thyroid cancer, regardless of the planned initial extent of surgery.5
Other associations and working groups recommend that PLTS be used in all patients,6–8 due to the discrepancy between subjective voice appreciation and the laryngoscopic findings (laryngeal paralysis may be present without dysphonia, and vice versa), the need to plan the surgical strategy in the event of paralysis revealed prior to surgery, in order to interpret the intraoperative neuromonitoring signal, and for medical-legal reasons.
Indeed, since there are patients with paralysis of a vocal cord that have a normal voice, routine PLTS is an essential standard of practice with good scientific and academic support that should be routinely performed to assess the extent of the disease, make key intraoperative decisions, and monitor complications and the functional outcomes postoperatively.9 In addition, unidentified preoperative unilateral paralysis of the RLN increases the risk of bilateral laryngeal paralysis if contralateral thyroidectomy is to be performed, with the risk of respiratory difficulty and the need for tracheotomy.1,10,11
Preoperative vocal cord paralysis in thyroid surgery (PVCPTS) identified by preoperative laryngoscopy suggests that there may be NLR invasion, and has a prevalence of 0-3.5% in patients with a preoperative diagnosis of benign disease and of 8% in those with malignant disease.1
The following research (PICO) question is therefore raised: In patients with thyroid disease subjected to primary thyroidectomy (patient), can preoperative laryngoscopy (intervention) related to the postoperative histopathological diagnosis (benign versus malignant disease)(comparison) yield differences in the prevalence of preoperative laryngeal paralysis (outcome)?
The present study was designed to assess the prevalence of laryngeal paralysis found at preoperative laryngoscopy in patients undergoing thyroidectomy, with a postoperative diagnosis of benign or malignant disease.
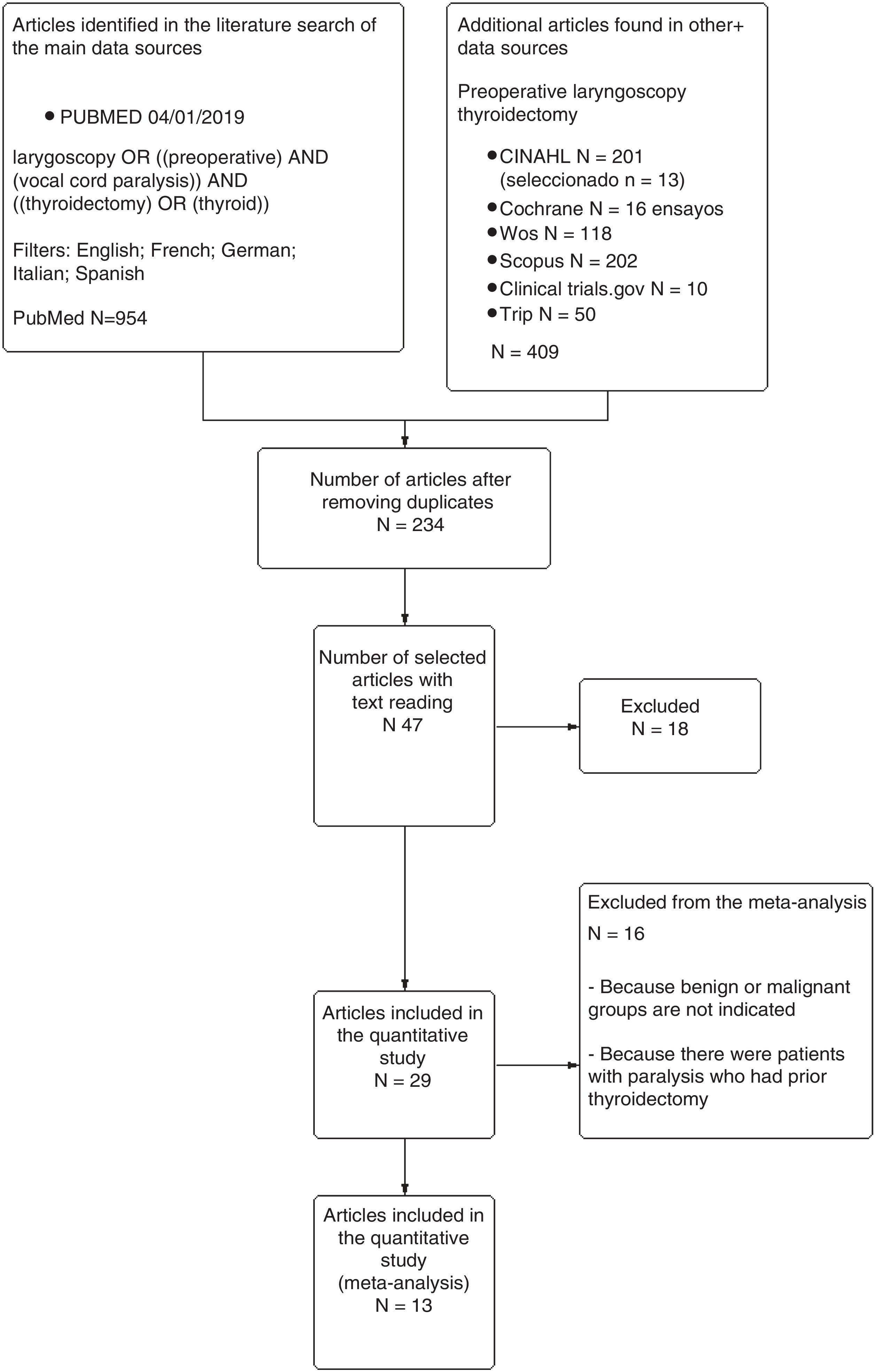
Material and methodsA systematic literature search was conducted in the PubMed, Cochrane Library, Scopus, CINAHL and WoS databases using the descriptors, strategies and filters summarized in Fig. 1. The final search was completed on 26 December 2018. The PRISMA-P12 checklist was used to generate the report.
The CREBP SRA tool (http://crebp-sra.com/#/tools) was used to select and remove duplicates.
The search, article selection and evaluation of the risk of bias were carried out by two investigators on an individual basis.
Criteria for the initial search and selection of patients: randomized and nonrandomized studies (retrospective or prospective observational studies) including a sample of adults subjected to primary thyroidectomy (total or partial), and who underwent preoperative laryngoscopy with any technique, with documentation of the number of patients with laryngeal paralysis at preoperative laryngoscopy and its relation to the final histological diagnosis (benign or malignant disease).
No randomized studies were found; the investigation therefore consisted of nonrandomized studies.
Patient exclusion: patients with laryngeal paralysis due to previous neck surgery (thyroidectomy, vascular surgery, surgical access to the cervical spine, or others).
Twenty-nine articles were selected for the qualitative study.13–41 A meta-analysis was made of 13 of these articles21,26–34 from which data could be obtained to assess the same effect (preoperative laryngoscopy performed on all included patients, documentation of the patients with preoperative laryngeal paralysis, documentation of the total number of patients, and the designation of preoperative paralysis to the postoperative histopathological malignant or benign groups).
The Wilcoxon test (W) was used for comparison of the mean paralysis data detected in the studies included in the meta-analysis versus those not included, according to the laryngoscopy technique used or whether voice assessment had been performed before surgery.
The ROBINS-I tool42,43 was used to assess the risk of bias in nonrandomized interventional studies.
The meta-analysis was performed using the RevMan 5 package (Version 5.3. Copenhagen. The Nordic Cochrane Center, The Cochrane Collaboration, 2014)44 applying the Mantel-Haenszel statistical method with analysis of the random effects model and the measurement of effect with the risk ratio and a 95% confidence interval (95%CI) for each study and for the total. Pooled prevalences were estimated with the MetaXL application for Excel (MetaXL version 5.3. Epigear International. www.epigear.com), assuming random effects, including a sensitivity analysis.
The GRADEpro tool (https://gdt.gradepro.org) was used to generate the table of results.
The descriptive statistical analyses and nonparametric tests were performed using the R statistical package (R version 3.5.2. The R Foundation for Statistical Computing).
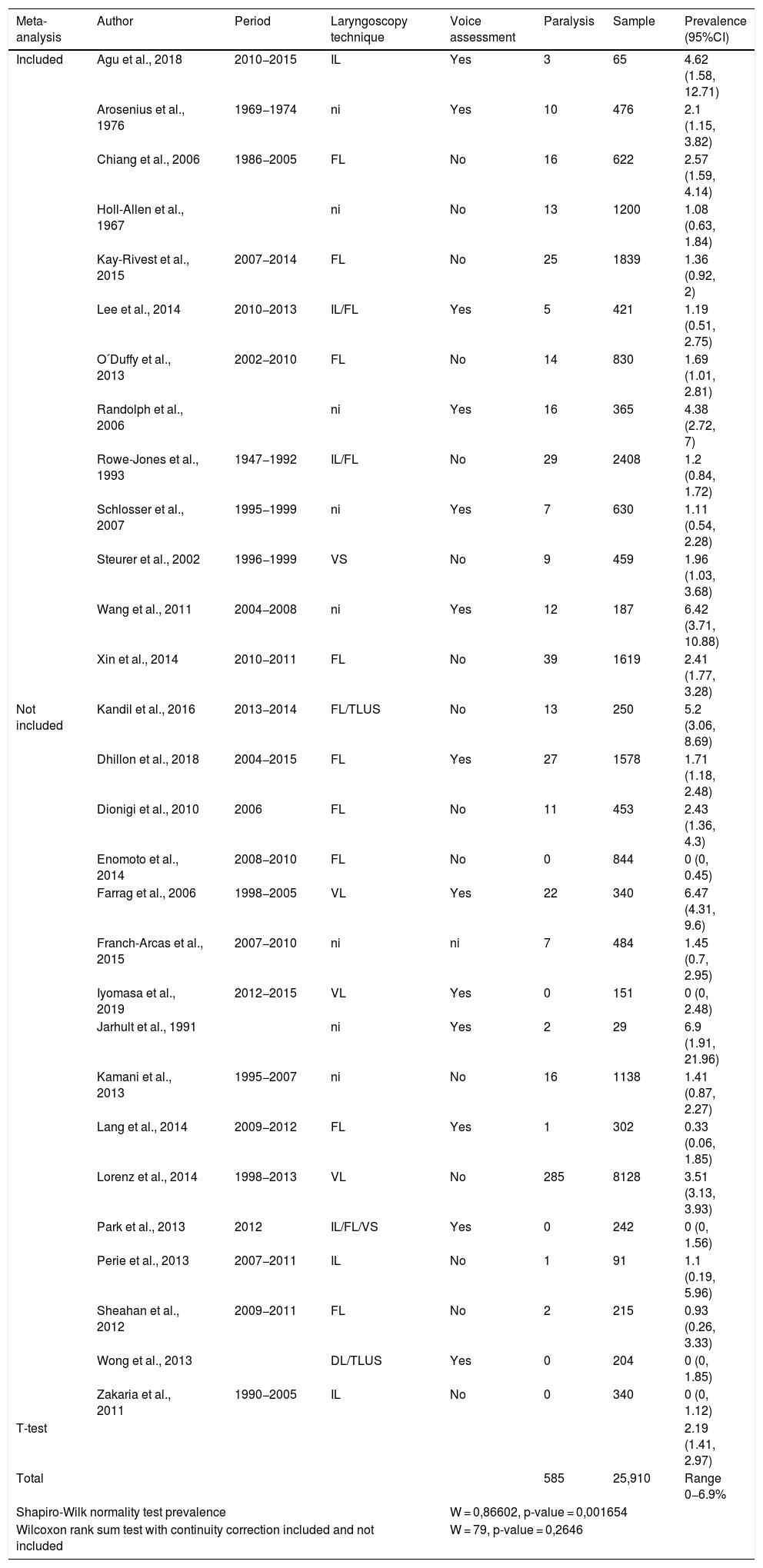
ResultsTable 1 shows the prevalence of PVCPTS in PLTS in the 29 studies selected for the qualitative study, comprising 25,910 patients subjected to primary thyroidectomy, in which 585 cases of unilateral vocal cord paralysis were detected (mean 2.19% [95%CI, 1.41–2.97], range 0−6.9%). The pooled prevalence in benign disease was 1.1% (95%CI, 0.7–1.7%; I2 71%) versus 6.3% in malignant disease (95%CI, 3.8–9.4%; I2 85%).
Prevalence of preoperative laryngeal paralysis in thyroid surgery found in the reviewed articles.
| Meta-analysis | Author | Period | Laryngoscopy technique | Voice assessment | Paralysis | Sample | Prevalence (95%CI) |
|---|---|---|---|---|---|---|---|
| Included | Agu et al., 2018 | 2010−2015 | IL | Yes | 3 | 65 | 4.62 (1.58, 12.71) |
| Arosenius et al., 1976 | 1969−1974 | ni | Yes | 10 | 476 | 2.1 (1.15, 3.82) | |
| Chiang et al., 2006 | 1986−2005 | FL | No | 16 | 622 | 2.57 (1.59, 4.14) | |
| Holl-Allen et al., 1967 | ni | No | 13 | 1200 | 1.08 (0.63, 1.84) | ||
| Kay-Rivest et al., 2015 | 2007−2014 | FL | No | 25 | 1839 | 1.36 (0.92, 2) | |
| Lee et al., 2014 | 2010−2013 | IL/FL | Yes | 5 | 421 | 1.19 (0.51, 2.75) | |
| O´Duffy et al., 2013 | 2002−2010 | FL | No | 14 | 830 | 1.69 (1.01, 2.81) | |
| Randolph et al., 2006 | ni | Yes | 16 | 365 | 4.38 (2.72, 7) | ||
| Rowe-Jones et al., 1993 | 1947−1992 | IL/FL | No | 29 | 2408 | 1.2 (0.84, 1.72) | |
| Schlosser et al., 2007 | 1995−1999 | ni | Yes | 7 | 630 | 1.11 (0.54, 2.28) | |
| Steurer et al., 2002 | 1996−1999 | VS | No | 9 | 459 | 1.96 (1.03, 3.68) | |
| Wang et al., 2011 | 2004−2008 | ni | Yes | 12 | 187 | 6.42 (3.71, 10.88) | |
| Xin et al., 2014 | 2010−2011 | FL | No | 39 | 1619 | 2.41 (1.77, 3.28) | |
| Not included | Kandil et al., 2016 | 2013−2014 | FL/TLUS | No | 13 | 250 | 5.2 (3.06, 8.69) |
| Dhillon et al., 2018 | 2004−2015 | FL | Yes | 27 | 1578 | 1.71 (1.18, 2.48) | |
| Dionigi et al., 2010 | 2006 | FL | No | 11 | 453 | 2.43 (1.36, 4.3) | |
| Enomoto et al., 2014 | 2008−2010 | FL | No | 0 | 844 | 0 (0, 0.45) | |
| Farrag et al., 2006 | 1998−2005 | VL | Yes | 22 | 340 | 6.47 (4.31, 9.6) | |
| Franch-Arcas et al., 2015 | 2007−2010 | ni | ni | 7 | 484 | 1.45 (0.7, 2.95) | |
| Iyomasa et al., 2019 | 2012−2015 | VL | Yes | 0 | 151 | 0 (0, 2.48) | |
| Jarhult et al., 1991 | ni | Yes | 2 | 29 | 6.9 (1.91, 21.96) | ||
| Kamani et al., 2013 | 1995−2007 | ni | No | 16 | 1138 | 1.41 (0.87, 2.27) | |
| Lang et al., 2014 | 2009−2012 | FL | Yes | 1 | 302 | 0.33 (0.06, 1.85) | |
| Lorenz et al., 2014 | 1998−2013 | VL | No | 285 | 8128 | 3.51 (3.13, 3.93) | |
| Park et al., 2013 | 2012 | IL/FL/VS | Yes | 0 | 242 | 0 (0, 1.56) | |
| Perie et al., 2013 | 2007−2011 | IL | No | 1 | 91 | 1.1 (0.19, 5.96) | |
| Sheahan et al., 2012 | 2009−2011 | FL | No | 2 | 215 | 0.93 (0.26, 3.33) | |
| Wong et al., 2013 | DL/TLUS | Yes | 0 | 204 | 0 (0, 1.85) | ||
| Zakaria et al., 2011 | 1990−2005 | IL | No | 0 | 340 | 0 (0, 1.12) | |
| T-test | 2.19 (1.41, 2.97) | ||||||
| Total | 585 | 25,910 | Range 0−6.9% | ||||
| Shapiro-Wilk normality test prevalence | W = 0,86602, p-value = 0,001654 | ||||||
| Wilcoxon rank sum test with continuity correction included and not included | W = 79, p-value = 0,2646 | ||||||
TLUS: transcutaneous laryngeal ultrasound; DL: direct laryngoscopy; FL: flexible laryngoscopy; IL: indirect laryngoscopy; ni: not indicated; VS: videostroboscopy; VL: videolaryngoscopy.
No cases of bilateral paralysis were reported.
No significant difference was found in the detection of preoperative vocal cord paralysis in relation to preoperative voice assessment (W = 88, p-value = 0.6776) or the laryngoscopy technique (W = 45, p-value = 0.3439).
No significant difference was found between the mean number of cases of paralysis detected in the studies included in the meta-analysis (2.47%) and those not included (1.97%) - Wilcoxon test, W = 74, p-value = 0.1947.
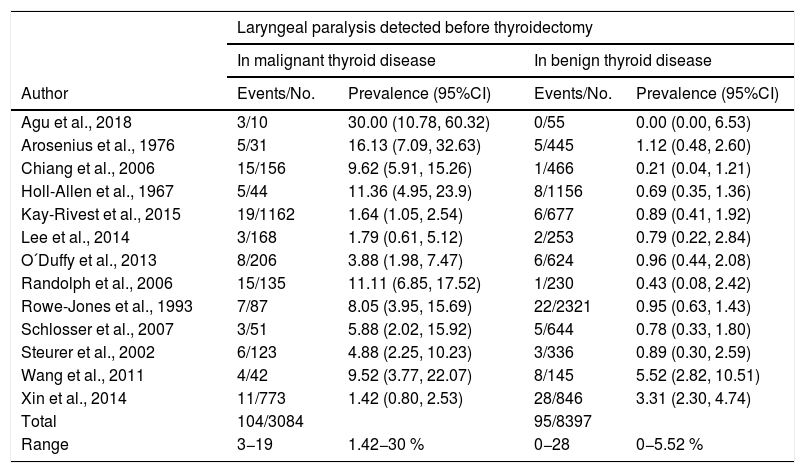
Table 2 shows the data from the 13 studies included in the meta-analysis, comprising 11,186 patients subjected to PLTS, and which reported on the distribution of preoperative paralysis according to the postoperative histopathological findings in 199 patients.
Laryngeal paralysis detected by preoperative laryngoscopy in the articles included in the meta-analysis.
| Laryngeal paralysis detected before thyroidectomy | ||||
|---|---|---|---|---|
| In malignant thyroid disease | In benign thyroid disease | |||
| Author | Events/No. | Prevalence (95%CI) | Events/No. | Prevalence (95%CI) |
| Agu et al., 2018 | 3/10 | 30.00 (10.78, 60.32) | 0/55 | 0.00 (0.00, 6.53) |
| Arosenius et al., 1976 | 5/31 | 16.13 (7.09, 32.63) | 5/445 | 1.12 (0.48, 2.60) |
| Chiang et al., 2006 | 15/156 | 9.62 (5.91, 15.26) | 1/466 | 0.21 (0.04, 1.21) |
| Holl-Allen et al., 1967 | 5/44 | 11.36 (4.95, 23.9) | 8/1156 | 0.69 (0.35, 1.36) |
| Kay-Rivest et al., 2015 | 19/1162 | 1.64 (1.05, 2.54) | 6/677 | 0.89 (0.41, 1.92) |
| Lee et al., 2014 | 3/168 | 1.79 (0.61, 5.12) | 2/253 | 0.79 (0.22, 2.84) |
| O´Duffy et al., 2013 | 8/206 | 3.88 (1.98, 7.47) | 6/624 | 0.96 (0.44, 2.08) |
| Randolph et al., 2006 | 15/135 | 11.11 (6.85, 17.52) | 1/230 | 0.43 (0.08, 2.42) |
| Rowe-Jones et al., 1993 | 7/87 | 8.05 (3.95, 15.69) | 22/2321 | 0.95 (0.63, 1.43) |
| Schlosser et al., 2007 | 3/51 | 5.88 (2.02, 15.92) | 5/644 | 0.78 (0.33, 1.80) |
| Steurer et al., 2002 | 6/123 | 4.88 (2.25, 10.23) | 3/336 | 0.89 (0.30, 2.59) |
| Wang et al., 2011 | 4/42 | 9.52 (3.77, 22.07) | 8/145 | 5.52 (2.82, 10.51) |
| Xin et al., 2014 | 11/773 | 1.42 (0.80, 2.53) | 28/846 | 3.31 (2.30, 4.74) |
| Total | 104/3084 | 95/8397 | ||
| Range | 3−19 | 1.42−30 % | 0−28 | 0−5.52 % |
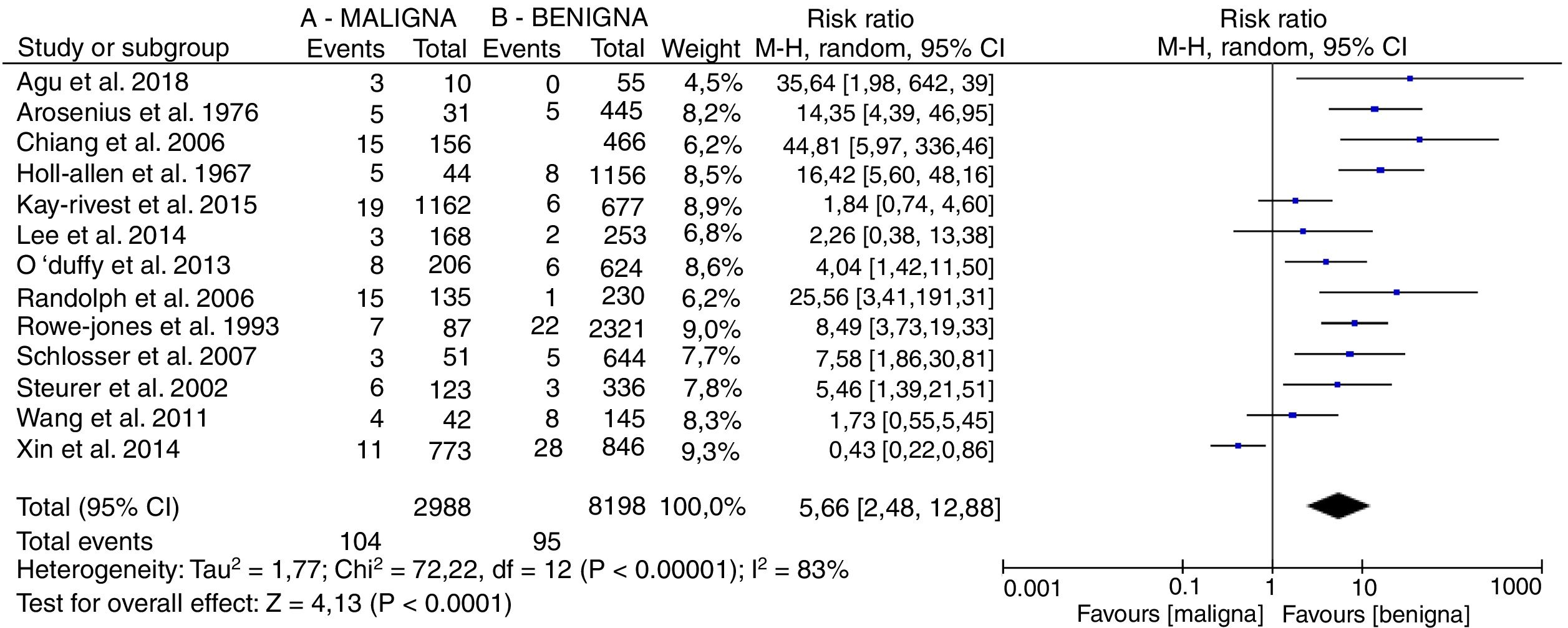
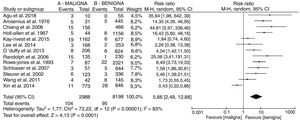
Fig. 2 shows the forest plot with the results of the meta-analysis.
The prevalence of preoperative laryngeal paralysis in malignant disease (A) versus benign disease (B) was analyzed taking the risk ratio as the effect size index weighted by the Mantel-Haenszel method, and assuming the random effects model given the great heterogeneity (I2 = 83%), there being a significantly higher prevalence among patients with malignant disease, with an estimated effect RR 5.66, 95%CI, 2.48, 12.88.
Although removal of the studies that increased heterogeneity contributed to decrease the latter, it did not modify the trend of effect.
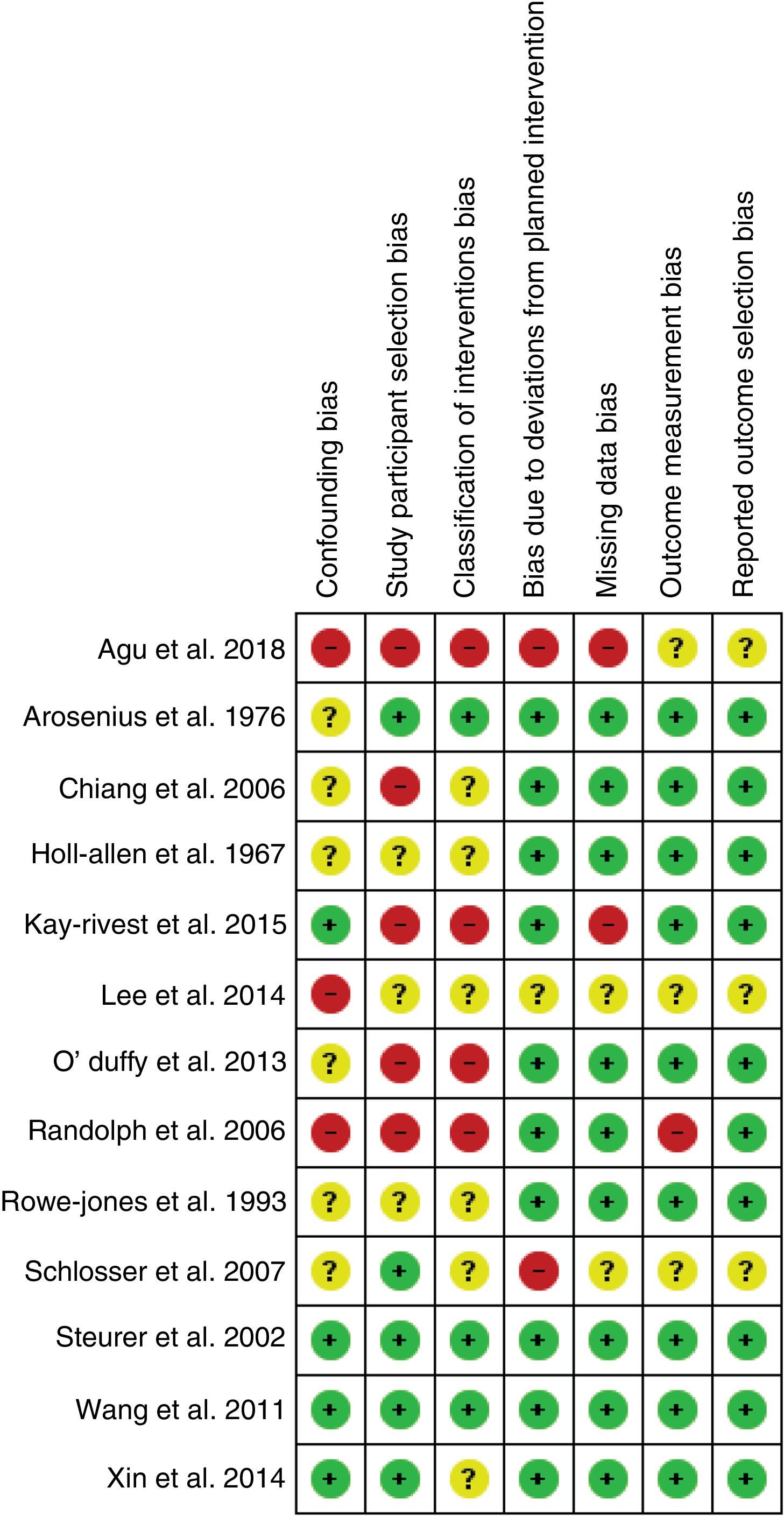
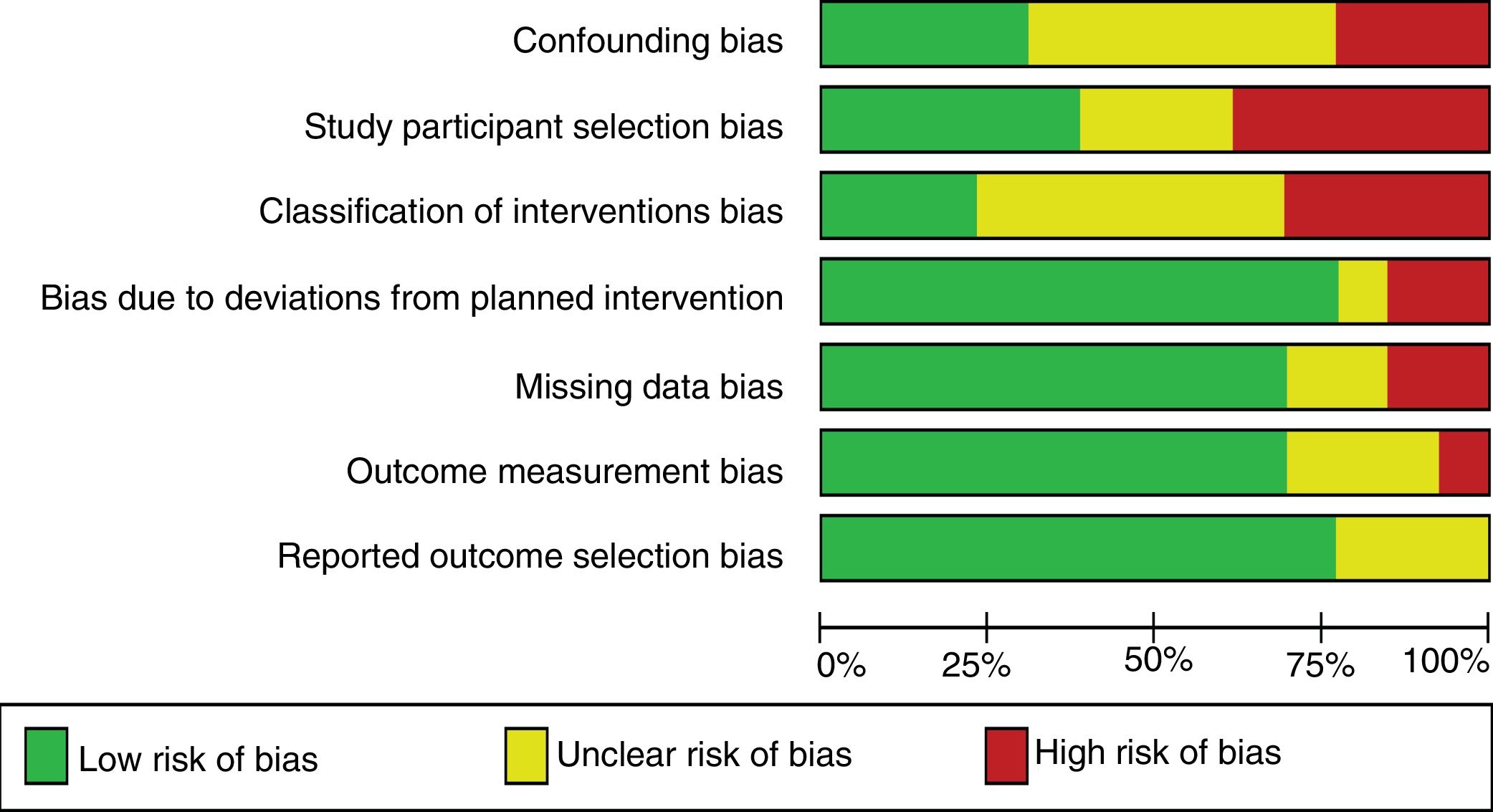
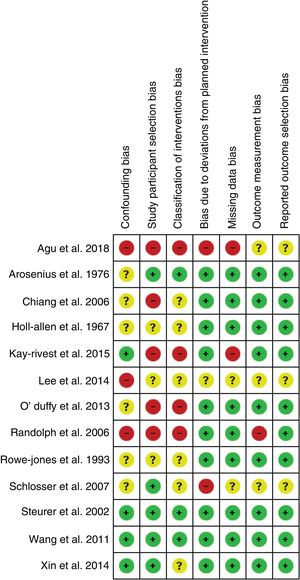
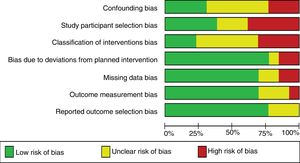
Fig. 3 summarizes the risk of bias assessed by the authors using ROBINS-I42,43 for each of the articles included in the meta-analysis. The risk of bias plot is shown in Fig. 4.
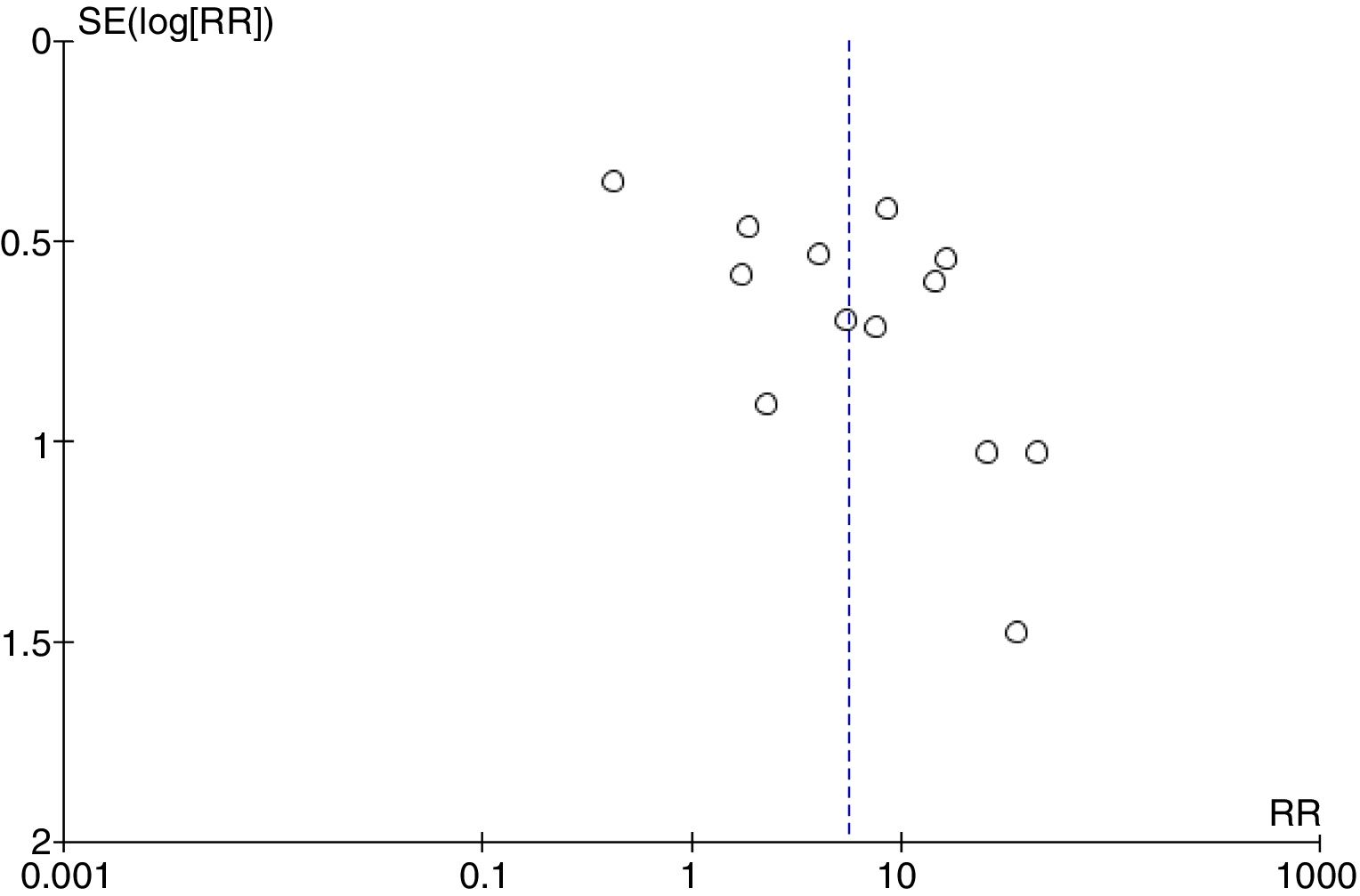
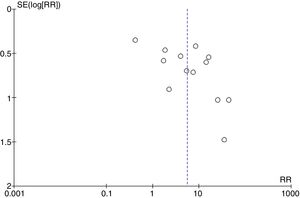
Fig. 5 shows the funnel plot with the studies included in the meta-analysis exhibiting high publication bias.
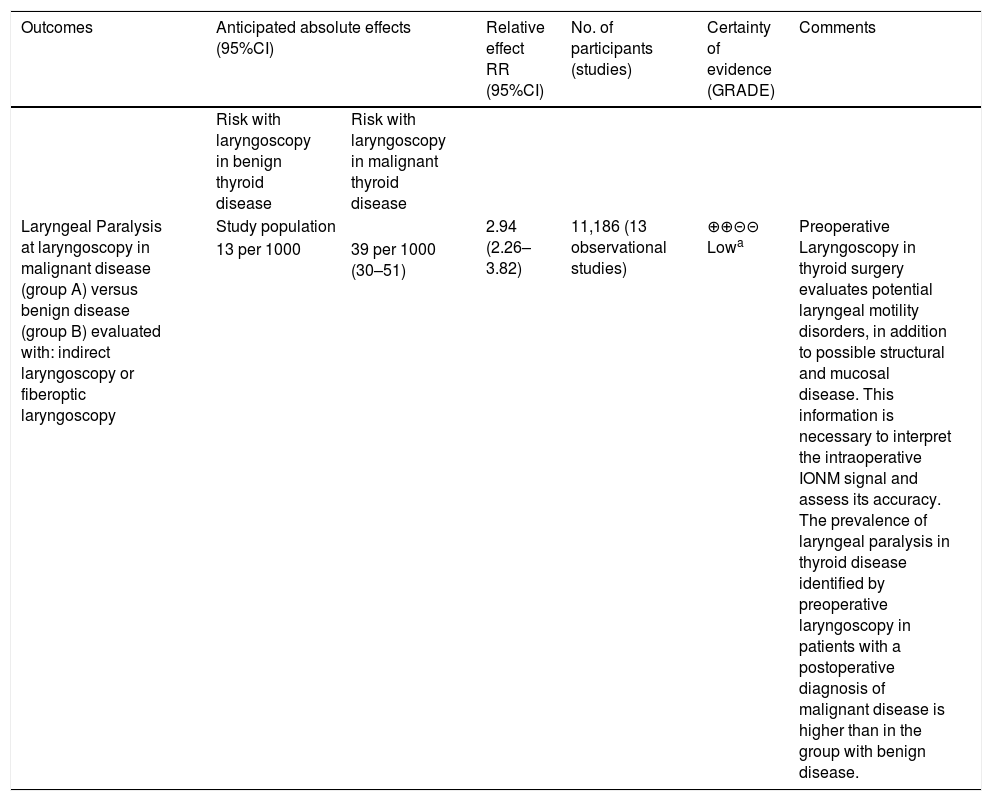
Table 3 summarizes the GRADE findings for the global articles included in the meta-analysis. The level of evidence is low. The risk of bias is high; publication bias corresponds to strong suspicion, and the effect size is large when the fixed effects method (RR 2.88 [2.20, 3.77]) is applied, and very large when the random effects model (RR 5.66 [2.48, 12.88]) is used.
Summarizing table of GRADE findings for the global studies included in the meta-analysis. Laryngeal paralysis detected by preoperative laryngoscopy in malignant and benign thyroid disease.
| Outcomes | Anticipated absolute effects (95%CI) | Relative effect RR (95%CI) | No. of participants (studies) | Certainty of evidence (GRADE) | Comments | |
|---|---|---|---|---|---|---|
| Risk with laryngoscopy in benign thyroid disease | Risk with laryngoscopy in malignant thyroid disease | |||||
| Laryngeal Paralysis at laryngoscopy in malignant disease (group A) versus benign disease (group B) evaluated with: indirect laryngoscopy or fiberoptic laryngoscopy | Study population | 2.94 (2.26–3.82) | 11,186 (13 observational studies) | ⊕⊕⊝⊝ Lowa | Preoperative Laryngoscopy in thyroid surgery evaluates potential laryngeal motility disorders, in addition to possible structural and mucosal disease. This information is necessary to interpret the intraoperative IONM signal and assess its accuracy. The prevalence of laryngeal paralysis in thyroid disease identified by preoperative laryngoscopy in patients with a postoperative diagnosis of malignant disease is higher than in the group with benign disease. | |
| 13 per 1000 | 39 per 1000 (30–51) | |||||
Patient or population: thyroid disease.
Intervention: laryngoscopy in malignant thyroid disease.
Comparison: laryngoscopy in benign thyroid disease.
Risk in the intervention group (and its 95%CI) is based on the assumed risk in the comparator group and on the relative effect of the intervention (and its 95%CI).
CI: confidence interval; RR: relative risk.
GRADE Working Group evidence classification. Strong certainty: we are very sure that the true effect is similar to the estimated effect. Moderate certainty: we moderately trust the estimated effect; the true effect is likely to be close to the estimated effect, but there is a possibility that it may be substantially different. Low certainty: our confidence in the estimated effect is limited; the true effect may be substantially different from the estimated effect. Very low certainty: we have very little confidence in the estimated effect; the true effect is likely to be substantially different from the estimated effect.
In the articles included in the meta-analysis, the prevalence of PVCPTS ranged from 1.42% to 30% in malignant disease and from 0% to 5.52% in benign disease. This wide variability may be due, among other factors, to differences in the techniques used (indirect laryngoscopy, videostroboscopy, flexible fiberoptic laryngoscopy or transcutaneous laryngeal ultrasound with a high false-negative results rate27).13,36,39
Although PVCPTS is considered to be an indicator of probable malignant disease, and its prevalence is higher than among patients with benign disease (RR 5.66 [2.48, 12.88]), it is not exclusive, as evidenced by the results of our meta-analysis.21,22,27,30 In this regard, it is probably more appropriate to refer to the invasive or noninvasive nature of the thyroid disease, independently of malignancy, following the criteria of Randolph and Kamani in classifying the groups as invasive (group 1) or noninvasive disease (group 2).29 Some authors advocate preoperative laryngoscopy only in cases of suspected malignancy, due to the low probability of finding PVCPTS in benign disease, and with a view to reducing costs.22
As a clinical predictor of invasive thyroid disease, PVCPTS is superior to imaging studies based on computed tomography (CT).29 Vocal cord paralysis due to malignant thyroid tumors is more common than in lung or esophageal tumors.24,33 Paralysis can occur through a number of mechanisms. In benign disease it can be secondary to compression or elongation, while in malignant disease an additional mechanism is tumor infiltration.21,24,27 Paralysis more often affects the left vocal cord.27 However, it should be taken into account that there may be other causes of paralysis unrelated to thyroid disease.27 Age is greater among patients with PVCPTS24 and in subjects with invasive disease (Randolph and Kamani group 129).
Not all patients with laryngeal paralysis report dysphonia,29 and the latter is therefore not a valid indicator of PVCPTS,32,33 since 16.629-87.2% of all patients with PVCPTS and 55.4% with postoperative paralysis revealed by laryngoscopy may be asymptomatic.34 Thus, preoperative and postoperative laryngoscopy may detect asymptomatic paralysis, and is therefore required in the preoperative and postoperative evaluation of all patients scheduled for thyroid surgery.29,34 In the study published by Lang et al., most of the patients with voice disorders before surgery presented no paralysis (33 patients with voice disorders, of which 7 presented paralysis, all with voice alterations; 7/33, 21.2%).20 However, the use of PLTS is not a generalized practice. In the United States, PLTS is estimated to be performed in 6.1%45 to 54% of the cases.27
This opens up another debate about voice evaluation in patients scheduled for thyroid surgery. Some authors recommend a complete preoperative voice study in patients with voice disorders, voice professionals, or in patients with a high preoperative score in questionnaires such as the Thyroidectomy-Related Voice Questionnaire (TVQ). This study should include fiberoptic laryngoscopy, a videostatic examination, perceptual voice analysis and acoustic analysis. Based on cost considerations, minimal assessment should include fiberoptic laryngoscopy and perceptual voice analysis.40
It is necessary to perform PLTS, because knowledge of the presence or absence of preoperative vocal cord paralysis allows the surgeon to assume invasive disease and to plan the diagnosis with complementary tests (imaging studies using neck and mediastinal CT, ultrasound, or endoscopy of the trachea and esophagus to evaluate mucosal invasion at the start of thyroidectomy), to perform specific surgical planning for each individual patient - including the potential need for tracheotomy or laryngotracheal surgery - and to inform and warn the patient before surgery.29 In addition, a knowledge of preoperative vocal cord motility is essential for making intraoperative decisions (such as leaving residual microscopic disease in functioning RLN, without resection in the case of contralateral paralysis)29 and for improved interpretation of the intraoperative neuromonitoring (IONM)34 signal.
If only voice changes were used as an indication for preoperative laryngoscopy, we would lose two thirds of the patients with invasive disease.29
Thus, some authors recommend laryngoscopy in all patients, regardless of voice or of the preoperative histopathological diagnosis.27
The results obtained in our review suggest that paralysis may be present in 2.19% (between 1.1 and 6.42%) of all patients scheduled for primary thyroid surgery, and is more common in patients with malignant thyroid disease (between 1.42 and 30%) as compared to patients with benign disease (up to 5.52%).
The investigations were based on nonrandomized retrospective studies; the supporting level of evidence was therefore low. Publication bias and heterogeneity were high, and removal from the meta-analysis of those studies that increased heterogeneity did not modify the trend of effect.
With regard to the laryngoscopy technique, the procedure was not used in all studies, and some authors failed to specify whether it was used or not. Not all articles indicated who performed laryngoscopy, and there was no blinding in the exploration in any of the publications.
No systematization was made of the laryngeal motility alterations identified at laryngoscopy. Xin et al. classified the findings into three types of abnormal motion (ranging from slow motility to absent motility with laryngeal asymmetry).34 Lang et al. classified them into two degrees (i. with reduced motility and ii. without motility).20 Lee et al. in turn classified the abnormalities into three categories (decreased vocal cord motility, complete vocal cord paralysis, or other abnormality),28 and Wong et al. classified them into three grades (from grade 1 [normal] to grade 3 [with paralysis]).39 Most studies do not reflect the criterion used to classify the motility disorders. The pattern of laryngeal motility is related to its postoperative course.34
Laryngoscopy is a routine examination in ear, nose and throat practice, and involves no cost.29 Preoperative laryngoscopy in thyroid surgery has a low yield and limited usefulness,31 because the prevalence of preoperative vocal cord paralysis is very low. This is attributed by some authors to selection bias.28
ConclusionsThe studies analyzed present biases that should be corrected in future research, with the elimination of blinding biases in the selection and allocation of patients or in the laryngoscopy technique used.
Preoperative laryngoscopy in thyroid surgery evaluates potential laryngeal motility disorders.
This information is necessary to interpret the IONM signal and to take decisions.
The prevalence of laryngeal paralysis in thyroid disease identified by preoperative laryngoscopy in patients with a postoperative diagnosis of malignant disease is higher than in the group with benign disease.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pardal-Refoyo JL, Pardal-Peláez B, Ochoa-Sangrador C, Estévez-Alonso JS. Parálisis laríngea detectada en la laringoscopia preoperatoria en patología de tiroides maligna y benigna. Revisión sistemática y metaanálisis. Endocrinol Diabetes Nutr. 2020;67:364–373.