Subclinical hypothyroidism is defined as elevation of thyroid-stimulating hormone (TSH) levels, with normal thyroid hormone levels and negative autoimmunity, in asymptomatic patients with no findings on examination. Because of the unwarranted increase in thyroid function tests in asymptomatic children, the main objective of this review was to analyze the course of these patients. Analysis of associated costs was a secondary objective.
Material and methodsA longitudinal, observational, retrospective study of patients referred to the endocrinology department of a tertiary hospital for high TSH levels (TSH 5–20mIU/l). Clinical and laboratory variables, number of visits until discharge, need for treatment, monitoring time, and economic variables were collected.
ResultsThe study sample consisted of 155 patients with a mean age of 7.8years±3.6SD. Referrals to endocrinology accounted for 4% of first office visits. Baseline mean TSH level was 7.8mU/l (5.03–15.8mU/l). TSH levels normalized after the first repeated measurement during the subsequent month in 60% of cases. A total of 83.6% of patients were discharged within a maximum of 3years, with a mean follow-up of 8.14±6.8months and 2.4visits/patient. Average cost per patient was €251.27 (range €143.49–444.21).
ConclusionIt is essential not to alarm the family when subclinical hypothyroidism is detected, because this is a biochemical situation which normalizes in most cases. This fact, together with the mean cost of specialized care, suggests that the first step should be repeated TSH measurements in primary care.
La hipertirotropinemia aislada se describe como una elevación de la hormona estimulante del tiroides (TSH) con niveles normales de hormonas tiroideas y autoinmunidad negativa en pacientes asintomáticos y sin hallazgos en la exploración. Dado el aumento no justificado del análisis de la función tiroidea en niños asintomáticos, el objetivo principal es analizar la evolución de estos pacientes. Como objetivo secundario se realiza un análisis de costes asociado.
Material y métodosEstudio longitudinal observacional retrospectivo de los pacientes derivados a endocrinología de un hospital de tercer nivel por hipertirotropinemia aislada (TSH 5-20mUI/l). Se recogieron variables clínicas, analíticas, número de visitas hasta el alta, necesidad de tratamiento, tiempo de seguimiento, así como variables económicas.
ResultadosSe obtuvo una muestra de 155 pacientes, con edad media de 7,8años ±3,6DE. La derivación a endocrinología representó el 4% de las consultas de primera visita. La cifra media de TSH inicial fue de 7,8mU/l (5,03-15,8mU/l). Los niveles de TSH se normalizaron tras la primera repetición durante el mes posterior, en el 60% de los casos. En un intervalo máximo de 3años fueron dados de alta el 83,6%, con un seguimiento medio de 8,14±6,8meses y 2,4 visitas/paciente. Se obtuvo un coste medio de 251,27€/paciente (rango 143,49-444,21€).
ConclusiónEs fundamental no generar alarma familiar ante una hipertirotropinemia, dado que se trata de una situación bioquímica que, en la mayoría de los casos, se normaliza. Este hecho, junto con el coste medio derivado de la asistencia especializada, pone de manifiesto que el primer paso debería ser la repetición de la misma en atención primaria.
Isolated hyperthyrotropinemia is described as a discrete elevation of thyroid stimulating hormone (TSH) with normal thyroid hormone levels (free T3 and T4) and negative autoimmunity in asymptomatic patients, with no alterations identified in the physical examination. The disorder is also referred to as subclinical hypothyroidism. However, this is a biochemical condition that does not involve clinical disease; consequently, it is more appropriate to use the former term.
Many studies are available on the natural course of hyperthyrotropinemia over time. Progression to hypothyroidism is uncommon, with normalization being the most common outcome.1,2
The main disorder that we need to discard in patients with elevated TSH levels is autoimmune thyroiditis, which is the most common cause of hypothyroidism acquired in childhood.3
In recent years there has been a marked tendency to request TSH determinations in routine blood tests, in many cases requested from primary care centers. Isolated TSH elevation is a common reason for referral to the pediatric endocrinology clinic, with the consequent family concern this implies. However, population-based screening for hypothyroidism outside the neonatal period is not warranted, except in concrete risk groups.2
Closer follow-up is required in such risk groups, in view of the greater frequency of primary hypothyroidism. These are patients with autoimmune diseases (type 1 diabetes mellitus, rheumatoid arthritis, celiac disease, vitiligo, etc.), individuals with chromosomal disorders (Down syndrome, Turner syndrome, etc.), people living in iodine-deficient areas, and patients receiving treatment with drugs that interfere with thyroid hormones (valproic acid, phenytoin, lithium, amiodarone, etc.).1,4
An increased prevalence of hyperthyrotropinemia has been reported in the presence of obesity2,5; an associated increase in cardiovascular risk has also been described.6–8 However, most studies have been conducted in the adult population, and in many cases the results have been inconclusive and are clearly not extrapolatable to the pediatric population.1 In this regard, an inappropriate tendency to extrapolate the relationship between TSH and cardiovascular risk in the adult population often leads to overtreatment, which in most cases is not needed in this age group.
In view of the above, our working hypothesis is that children referred to hospital due to TSH levels ranging between 5 and 20mIU/l, with no other associated disorders, mostly suffer no disease and therefore do not initially require T4 replacement therapy.
The primary objective of our study was to analyze the middle-term course of patients with hyperthyrotropinemia seen in the endocrinology clinic, in view of the unwarranted increase in requests for thyroid function testing in asymptomatic children, and the existing controversy regarding the required management approach. As a secondary objective, we conducted a cost analysis of such patient consultations.
Material and methodsA retrospective, longitudinal observational study was carried out involving all patients under 14years of age referred to the pediatric endocrinology clinic of a tertiary hospital due to isolated hyperthyrotropinemia (TSH 5–20mIU/l). A search was made in the database of the Andalusian Public Health System (Diraya, DAH) using the diagnostic terms “isolated hyperthyrotropinemia” or “subclinical hypothyroidism”. As inclusion criteria, and in addition to the above-mentioned age and reason for consultation, the patients were required to have been referred to our Department in the previous three years (2015–2017). On the other hand, patients who in addition to elevated TSH levels had consistent symptoms, goiter or chromosomal disorders, or who were being treated with drugs that could interact with thyroid hormones, were excluded from the study. As an exception, we included patients with positive autoimmunity, because the corresponding determinations were made once they had already been referred.
We likewise recorded clinical (age, weight, height, presence of goiter) and laboratory test variables (TSH and FT4 on the first visit, as well as TSH, FT4 and anti-thyroperoxidase [TPO] antibodies requested successively over time). On a standardized basis, laboratory testing was requested on the first visit, with the determination of TSH, FT4 and anti-TPO antibodies, which was performed in the month following the visit. The number of visits made until discharge, whether treatment was required, and the duration of follow-up (in months) until discharge were also recorded. Lastly, we compiled the variables for the cost analysis, using the costs provided by the clinical analysis department and the hospital pharmacy, namely a cost per visit of 139.5€ (first visit) and 69.75€ (successive visits), and a cost per laboratory test (thyroid function; TSH, FT4, anti-TPO) of 6.87€.
Hormone parameters (TSH, FT4 and TPO) were measured using electrochemiluminescent assay (ECLIA) with ruthenium chelate-labeled antibodies, TSH levels ranging from 0.4 to 5μIU/ml being considered normal.
The variables were subjected to a statistical analysis, the patient's course being assessed by year and subsequently on a global basis for the three year study period. Values were reported as the mean and standard deviation, and qualitative variables were reported as percentages. Likewise, the characteristics of the patients requiring treatment were analyzed in comparison with the other patients.
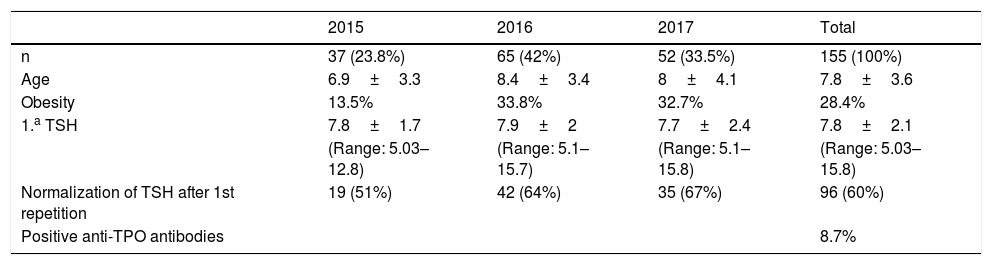
ResultsReferral to the endocrinology department due to hyperthyrotropinemia represented 4% of the consultations on the first visit to our unit. A sample of 155 patients was compiled. A total of 45.8% were males, with a mean age (standard deviation [SD]) of 7.8±3.6years, and 28.4% were overweight or obese. The mean TSH concentration was 7.8mU/l (range 5.03–15.8mU/l) (Tables 1 and 2).
Characteristics of the study population over the three consecutive years.
| 2015 | 2016 | 2017 | Total | |
|---|---|---|---|---|
| n | 37 (23.8%) | 65 (42%) | 52 (33.5%) | 155 (100%) |
| Age | 6.9±3.3 | 8.4±3.4 | 8±4.1 | 7.8±3.6 |
| Obesity | 13.5% | 33.8% | 32.7% | 28.4% |
| 1.a TSH | 7.8±1.7 | 7.9±2 | 7.7±2.4 | 7.8±2.1 |
| (Range: 5.03–12.8) | (Range: 5.1–15.7) | (Range: 5.1–15.8) | (Range: 5.03–15.8) | |
| Normalization of TSH after 1st repetition | 19 (51%) | 42 (64%) | 35 (67%) | 96 (60%) |
| Positive anti-TPO antibodies | 8.7% |
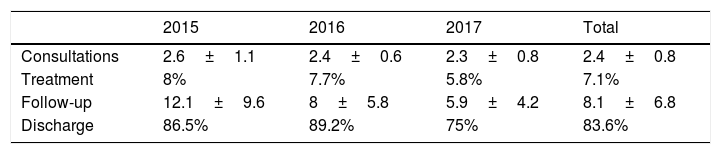
The TSH levels normalized after the first repeat measurement in the month after the visit in 96 cases (60%), with consequent patient discharge from the endocrinology clinic. The condition evolved towards primary hypothyroidism in 7.1% of the patients, with the start of replacement therapy. A total of 83.6% of the patients were discharged in the course of a maximum follow-up period of three years (since the patients referred over the previous three years were considered). The mean duration of follow-up was 8.14±6.8months, with a mean number of visits of 2.4. The analysis of the characteristics of the patients requiring replacement therapy revealed no significant differences in terms of age, baseline TSH or autoimmunity.
We recorded a mean cost per patient seen for hyperthyrotropinemia in our department of 251.27€, with a range from 143.49 to 444.21€. The mean cost of the blood tests was 12.75€/patient, with a mean consultation cost of 238.5€/patient.
DiscussionOf note in our study is the fact that in 83.6% of the cases repetition of the assessment of thyroid function in successive tests made over a maximum follow-up period of three years revealed values within the normal ranges, thereby warranting patient discharge from our unit. In addition, in 60% of these cases normalization had already been confirmed by the first repetition of the laboratory tests, one month after the first measurement, this probably being attributable to the low reproducibility of the laboratory tests.9
Our results are similar to those of Pérez-Pérez et al.,3 in a study conducted in 2014 at Hospital Infantil Universitario Niño Jesús, in which the natural course of TSH and the costs of the disorder were analyzed in a sample of 102 patients. Of note is the fact that TSH normalized in 90.4% of the patients. The number of consultations was also very similar, with 2.6±1.5 visits on average. The mean cost described by these authors was 570±273.15€ per patient. However, despite the similarities between the two studies, comparisons cannot be made, since the analysis of these investigators included all patients with TSH elevation, with goiter or receiving treatment with antiepileptic drugs. Furthermore, they added the costs associated with the ultrasound studies, which were not considered in our analysis. We also found the TSH levels to “normalize” in the first month in most cases, a circumstance that cannot be attributed to the natural course of hyperthyrotropinemia, but rather to the poor reproducibility of the method employed.
In turn, a 5-yearmulticenter study of 3632 Israeli patients with hyperthyrotropinemia found the most common course to be a normalization of the values, conditioned to the initial TSH concentration. Specifically, in the case of TSH 5–10mIU/l, normalization was recorded in 73.6% of the patients, while in the case of TSH>10mIU/l, normalization occurred in 40%. The identified predictive factors were therefore elevated TSH>7.5mIU/l) and female gender.10
There is controversy regarding when to treat patients over three years of age with isolated, asymptomatic hyperthyrotropinemia not belonging to risk groups. In our opinion, treatment should be started when TSH>20mIU/l or between 10 and 20mIU/l in the event of patients at risk (autoimmune disease, chromosomal disorders, positive anti-TPO antibodies, the presence of goiter, etc.). Mention should be made of a study conducted in Turin (Italy), in which patients with hyperthyrotropinemia were divided into two groups and replacement therapy was started in one of them. The results showed the therapy to be ineffective in preventing subsequent TSH elevation after treatment suspension.11
Hyperthyrotropinemia is much more common in adults than in the pediatric population (estimated prevalence 4–20%),2,5 and as commented above, it is associated with dyslipidemia, insulin resistance, diastolic dysfunction and coronary disease. A more aggressive approach regarding the start of treatment is therefore adopted, replacement therapy being recommended from TSH>10mIU/l, or between 5 and 10mIU/l in the presence of symptoms suggestive of thyroid involvement.5,12,13 By contrast, a prevalence of approximately 1.7–2.9% has been reported in the pediatric population,2 and a more conservative approach is proposed in relation to the start of treatment.14
As regards the relationship between hyperthyrotropinemia and obesity, a similar prevalence of obesity has been reported in patients with hyperthyrotropinemia as in the general population (30%), this being consistent with our own observations. Nevertheless, weight loss in obese patients has been shown to decrease the TSH levels and improve the lipid profile; the disorder therefore appears to be a consequence and not a cause of obesity.15–18 The underlying mechanism is not known, though it has been suggested that the proinflammatory state seen in obesity could play a role.1,18 Likewise, some studies have shown that treatment with levothyroxine in patients with obesity and elevated TSH does not improve the lipid profile.1,19
In addition, a number of studies have reported a relationship between hyperthyrotropinemia and increased cardiovascular risk, with an altered lipid profile and carotid intima thickening.6–8,20,21 However, other studies have failed to observe this association.22 These results differ from those obtained in the adult population, where such a relationship appears to be clearer.23–26
As limitations of our study, the included patients only consisted of those referred to the pediatric endocrinology clinic of a hospital serving as reference for the entire province. The number of patients with hyperthyrotropinemia probably would have been much greater if we had included those patients who were treated in primary care or in a private medical setting, and consequently were not referred to us. With regard to the analysis of the characteristics of the patients requiring treatment, no significant results were obtained, probably due to the few patients receiving treatment. It should also be noted that we included patients with positive antibodies, who cannot strictly be included under the term “isolated hyperthyrotropinemia”. Nevertheless, the analysis of the course of these patients showed no differences versus those with negative autoimmunity.
The main strength of our study is its single-center design, which implies that the approach and data compilation were very homogeneous, as shown by the small variability in the results obtained over the consecutive three-year period of the study.
Based on the data obtained, our recommendation in children over three years of age with hyperthyrotropinemia (5–20mIU/l) is to repeat testing of TSH, FT4 and antithyroid (anti-TPO) antibodies as a first measure. If discrete elevation is confirmed and the antibodies prove negative, we should repeat testing every 6–12months. Discharge may be assessed and follow-up can be carried out by the primary care pediatrician. We recommend closer monitoring in the case of persistent TSH elevation>10mIU/l, in view of the increased likelihood of treatment being required. Patients with positive antibodies should no longer be dealt with as isolated hyperthyrotropinemia cases, and closer monitoring is required.
ConclusionHyperthyrotropinemia in asymptomatic patients is a common reason for referral to the endocrinology clinic, and represents 4% of all first visits to our unit. It is essential not to generate family alarm in the face of such a situation, since it only represents a biochemical condition which in most cases naturally tends towards normalization.
This circumstance, together with the mean costs associated with specialized care, shows that when moderate and isolated TSH elevation is detected in the absence of symptoms of hypothyroidism, TSH measurement should be repeated, with autoimmune testing being requested, if possible, from primary care.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Álvarez Casaño M, López Siguero JP. Revisión de la evolución de los pacientes con hipertirotropinemia y estudio de costes. Endocrinol Diabetes Nutr. 2019;66:550–554.