In recent years, the implementation of electronic health records across all hospitals and primary care centres within the National Health System has significantly enhanced access to patients’ clinical data. This study aims to estimate the prevalence of type 2 diabetes (T2DM) in primary care settings and to outline its associated cardiovascular risk factors (CVRF) and epidemiological characteristics.
MethodsAn observational cross-sectional study was conducted including 89,679 patients diagnosed with T2DM who attended the primary health care system from 2014 to 2018. Data was provided by the Primary Health Care System of the Principality of Asturias (SESPA).
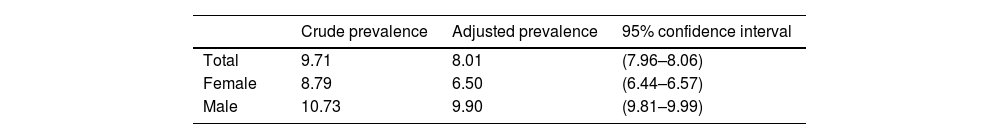
ResultsThe estimated prevalence of diagnosed T2DM was 8.01% (95% Confidence Interval [CI]: 7.96–8.06) of the total population. Additionally, it was more prevalent in males compared to females (9.90% [95% CI: 9.81–9.99] vs. 6.50% [95% CI: 6.44–6.57]) and increased with age in both sexes. People with T2DM had an average age of 74 years, 52.3% were male, and the most frequently associated CVRF were: dyslipidaemia (47.90%) and hypertension (62.20%). Glycaemic control improved during the 2014–2018 period (31.69%), as did lipid control (23.66%). However, the improvement in blood pressure control (9.34%) was less pronounced for the same period. Regarding the multifactorial control of diabetes (measured by LDL-cholesterol, HbA1C and blood pressure) the overall degree of control improved by 11.55% between 2014 and 2018.
ConclusionIn this 5-year retrospective population-based study, the utilisation of data from electronic medical records provides insights into the prevalence of T2DM in a large population, as well as real-time CVRFs. Leveraging this data facilitates the development of targeted health policies.
En los últimos años, la implementación de registros electrónicos de salud en todos los hospitales y centros de atención primaria dentro del Sistema Nacional de Salud ha mejorado significativamente el acceso a los datos clínicos de los pacientes. Este estudio tiene como objetivo estimar la prevalencia de la diabetes tipo 2 (T2DM) en entornos de atención primaria y describir sus factores de riesgo cardiovascular (CVRF) asociados y características epidemiológicas.
MétodosSe realizó un estudio observacional transversal que incluyó a 89.679 pacientes diagnosticados con T2DM que asistieron al sistema de atención primaria de salud desde 2014 hasta 2018. Los datos fueron proporcionados por el Sistema de Atención Primaria de Salud del Principado de Asturias (SESPA).
ResultadosLa prevalencia estimada de T2DM diagnosticada fue del 8,01% (intervalo de confianza del 95% [IC]: 7,96-8,06) de la población total. Además, fue más prevalente en hombres en comparación con mujeres (9,90% [IC del 95%: 9,81-9,99] vs. 6,50% [IC del 95%: 6,44-6,57]) y aumentó con la edad en ambos sexos. Las personas con T2DM tenían una edad promedio de 74 años, el 52,3% eran hombres y los CVRF más frecuentemente asociados fueron: dislipidemia (47,90%) e hipertensión (62,20%). El control glucémico mejoró durante el período de 2014-2018 (31,69%), al igual que el control lipídico (23,66%). Sin embargo, la mejora en el control de la presión arterial (9,34%) fue menos pronunciada para el mismo período. En cuanto al control multifactorial de la diabetes (medido por LDL-colesterol, HbA1C y presión arterial), el grado general de control mejoró un 11,55% entre 2014 y 2018.
ConclusiónEn este estudio retrospectivo de base poblacional de 5 años, la utilización de datos de registros electrónicos de salud proporciona información sobre la prevalencia de T2DM en una gran población, así como sobre los CVRF en tiempo real. El aprovechamiento de estos datos facilita el desarrollo de políticas de salud dirigidas.
Diabetes mellitus (DM) is a chronic disease that has become one of the major public health problems worldwide. According to the International Diabetes Federation, in 2021, it was estimated that 537 million adults had diabetes, which is projected to increase to 643 million by 2030 and to 783 million by 2045 (type 1 diabetes represents approximately 5–10%), although there are substantial differences between regions.1 This means a global diabetes prevalence of 10.5% in 2021, which is expected to increase to 12.2% by the year 2045. The increase in the incidence of diabetes may be due to many factors, but the most prominent are changes in diagnostic criteria and disease management, increased case detection, improved survival rates and the influence of various environmental factors. In Europe, the prevalence of DM was reported to be 9.2% in adults aged 20–79 years.1 In Spain, according to the Primary Care Clinical Data Base (BDCAP) published in 2020 the prevalence of DM was 6.6% of the total population assigned to primary care in the National Health System.2 In contrast, The Di@bet.es Study showed, for the first time, that the prevalence rate of diabetes was 13.8% in a representative sample of the Spanish population in 2012.3 In Asturias, based on the data from BDCAP as reported in the study conducted by Menendez-Torre et al., the prevalence of DM was determined to be 6.48%.2
The digitization of healthcare systems has brought about the production of a large amount of electronic patient data that is integrated into them. The storage of this information has led to the creation of “big data” or massive, complex and varied data sets that require the use of technological tools to be processed.4 Furthermore, the development, use, and implementation of various intelligent devices in patient health monitoring, as well as the evolution of data analysis techniques based on artificial intelligence, has led to a significant increase in big data that can be used for various purposes. All the information collected in healthcare systems is known as Real-World Data (RWD), which provides knowledge to establish Real-World Evidence.5
RWD that accurately describe the total population with diagnosed diabetes within a geographical area, and that include validated clinical data, are currently lacking.6 Our hypothesis is that prevalence rates based on self-reported data, administrative registries without validated diagnoses or health surveys with a risk of selection bias, may differ significantly from the actual prevalence rates. The prevalence of DM in the adult outpatient population in our local setting, the Principality of Asturias, and its epidemiological characteristics are currently unknown. To date, only a few studies with representative samples have been conducted. Therefore, the aim of this work is to determine the prevalence of diagnosed type 2 diabetes mellitus (T2DM) based on primary care records from Asturias and analyse the trends of cardiovascular risk factors (CVRF), as well as comorbidities associated with T2DM.
MethodsStudy design and populationThe Principality of Asturias is an 11,000km2 autonomous community located in northern Spain with 78 municipalities and a total population of 1,023,627 as of 31 October 2018.7 Asturias has a public health system in which every citizen is registered with a general practitioner (GP) and a nurse at a publicly funded primary care centre. At each centre, GPs and nurses work as a team caring for the total population of a determined geographic area. All primary care centres use the same software, called OMI-AP, to record all the patients’ clinical information. Diagnostic procedures and healthcare are free of charge to patients. Thus, this study encompasses the vast majority of individuals with diabetes in the general population attending primary health care at GP practices. This study was a cross-sectional, observational and descriptive study, which included all patients over 14 years of age who had attended the primary health care system of the Health Service of the Principality of Asturias (SESPA) between 2014 and 2018. The study protocol was evaluated and approved by the Research Ethics Committee of the Principality of Asturias (no. 137/16). As this was an observational and retrospective study, the participants were not required to sign an informed consent form.
Data requestAll clinical and administrative information related to comprehensive care is stored in a single, centralised repository of computerised data accessible through the electronic medical record (EMR) in OMI-AP. To gather patient information, a formal request was made by the Sociedad Asturiana de Medicina de Familia y Comunitaria (SAMFyC) to the Health Service of the Principality of Asturias (SESPA) for access to diagnosed diabetes records, specifically those coded according to the International Classification of Diseases 10 (ICD-10) with codes E11 and E14.8,9 This information was included in the Data for Improvement in the Care of People with Diabetes in Asturias (DaMeDiAs) project. For this study, we considered only individuals aged 14 years and older, excluding paediatric patients from the analysis. Additionally, we analysed variables pertaining to demographic information and cardiovascular risk factors, including dyslipidaemia (coded as E78 in the ICD-10) and arterial hypertension (coded as I10, I11, I12, I13, and I15 in the ICD-10). We also examined macrovascular complications such as coronary artery disease and cerebrovascular disease (coded as G45 and G46, respectively, in the ICD-10), along with other essential variables required to define metabolic control.
Metabolic control variablesHigh-performance liquid chromatography methods were used to measure glycated haemoglobin (HbA1c). Mean systolic and diastolic blood pressures were calculated by including all readings obtained. Blood pressure (BP) control was defined as mean systolic and diastolic blood pressures less than 140/90mm Hg respectively. In addition, serum cholesterol was measured enzymatically and low-density lipoprotein (LDL) cholesterol values were calculated. Lipid control was defined as an LDL cholesterol level below 100mg/dL. Multifactorial control of T2DM, stated by the current local guideline targets, and defined as HbA1c≤7%, BP≤140/90mmHg and LDL cholesterol≤100mg/dL were also analysed, which is considered the target for metabolic control.
Statistical analysisPrevalences are reported with their respective 95% confidence intervals (95% CI), estimated using a normal approximation. The denominator was defined as a reference population, the population with an Individual Health Insurance Card registered in the Population and Resources Identification System, which is used as the key standard for population reference in the SESPA.7 The numerator was defined as the count of cases identified with the codes E11 and E14 from the International Classification of Diseases, denoting patients with T2DM. Specifically, E11 corresponds to non-insulin-dependent diabetes mellitus, while E14 refers to unspecified diabetes mellitus. Global rates are reported, as well as rates stratified by sex. A descriptive analysis of the variables was conducted, with categorical variables represented as absolute and relative frequency, and continuous variables presented as median and interquartile range. To compare the results of our analysis with other studies, we adjusted the prevalence according to the European Standard Population10 using the direct method in 5-year intervals.2 All statistical analyses and graphing were performed with R version 3.5.2.11
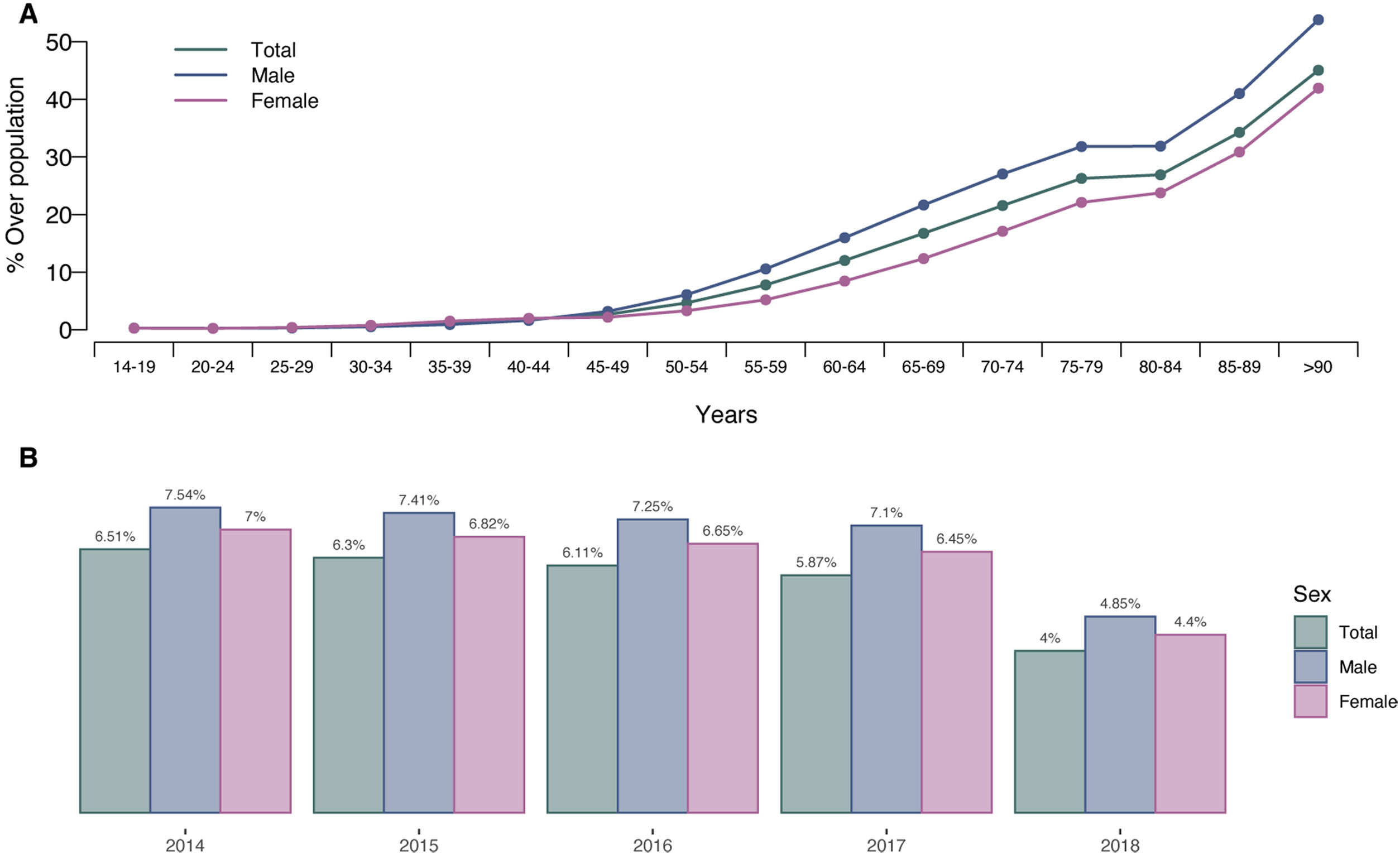
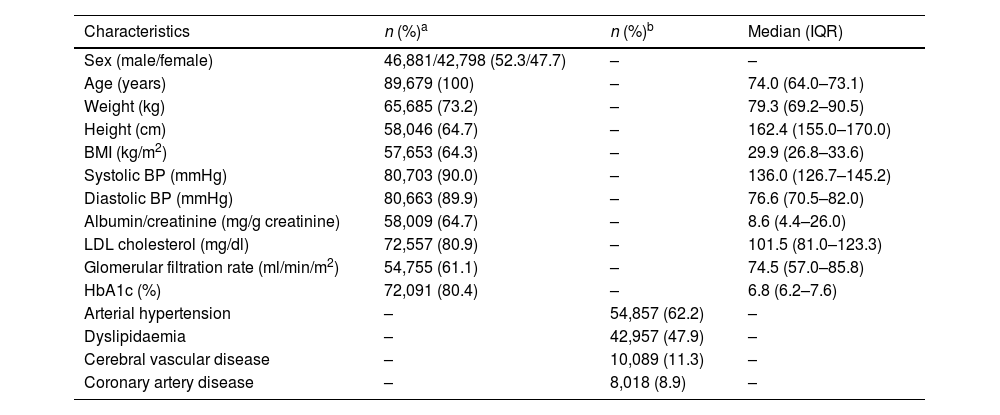
ResultsA total of 89,679 patients with a diagnosis of T2DM were detected out of a total population of 923,158 (≥14 years). Our dataset included both males (n=46,881; 52.3%) and females (n=42,798; 47.7%). The median (IQR) age was 74.0 (64.0–73.1) years (Table 1). The overall prevalence of T2DM in patients over 14 years from 2014 to 2018 was 8.01% (95% CI: 7.96–8.06) (Table 2). Table 2 shows the overall prevalence stratified by sex, where a prevalence of 6.50% (95% CI: 6.44–6.57) for T2DM was observed in women, while for males, the data showed a prevalence of 9.90% (95% CI: 9.81–9.99). Additionally, the prevalence progressively increases as we expand the age range, primarily from 45 years onwards (Fig. 1A). Moreover, after adjusting for the European population, the prevalence is higher in males than females for all age groups. Fig. 1B shows the overall prevalence year by year between 2014 and 2018.
Characteristics and vascular complications of all adults with diabetes mellitus in the Principality of Asturias between 2014 and 2018.
| Characteristics | n (%)a | n (%)b | Median (IQR) |
|---|---|---|---|
| Sex (male/female) | 46,881/42,798 (52.3/47.7) | – | – |
| Age (years) | 89,679 (100) | – | 74.0 (64.0–73.1) |
| Weight (kg) | 65,685 (73.2) | – | 79.3 (69.2–90.5) |
| Height (cm) | 58,046 (64.7) | – | 162.4 (155.0–170.0) |
| BMI (kg/m2) | 57,653 (64.3) | – | 29.9 (26.8–33.6) |
| Systolic BP (mmHg) | 80,703 (90.0) | – | 136.0 (126.7–145.2) |
| Diastolic BP (mmHg) | 80,663 (89.9) | – | 76.6 (70.5–82.0) |
| Albumin/creatinine (mg/g creatinine) | 58,009 (64.7) | – | 8.6 (4.4–26.0) |
| LDL cholesterol (mg/dl) | 72,557 (80.9) | – | 101.5 (81.0–123.3) |
| Glomerular filtration rate (ml/min/m2) | 54,755 (61.1) | – | 74.5 (57.0–85.8) |
| HbA1c (%) | 72,091 (80.4) | – | 6.8 (6.2–7.6) |
| Arterial hypertension | – | 54,857 (62.2) | – |
| Dyslipidaemia | – | 42,957 (47.9) | – |
| Cerebral vascular disease | – | 10,089 (11.3) | – |
| Coronary artery disease | – | 8,018 (8.9) | – |
BP=blood pressure; HbA1c=glycated haemoglobin; LDL cholesterol=Low-density lipoprotein cholesterol; BMI=body mass index; InterQuartile Range (IQR): percentile 25–percentile 75.
Prevalence of type 2 diabetes mellitus diagnosed in the Principality of Asturias between 2014 and 2018. (A) Prevalence of T2DM diagnosed in the Principality of Asturias between 2014 and 2018 by age group and sex. (B) The diagnosed prevalence of T2DM in each year in the Principality of Asturias between 2014 and 2018 is based on data collected through electronic medical records for each year.
Data related to metabolic control are shown in Table 1. 80.4% of the patients had at least one mean HbA1c in the last year, with a median value of 6.8%. Regarding systolic/diastolic blood pressure, approximately 90% had a recorded value with a median of 136.0/76.6mmHg. LDL cholesterol was determined in 80.9% of patients, with an average value of 101.5mg/dL (Table 1). The most frequent non-communicable cardiovascular comorbidities were: 62.2% arterial hypertension and 47.9% dyslipidaemia. As for complications related to the pathology, the most frequent antecedents were coronary artery disease (8.9%) and cerebral vascular disease (11.3%).
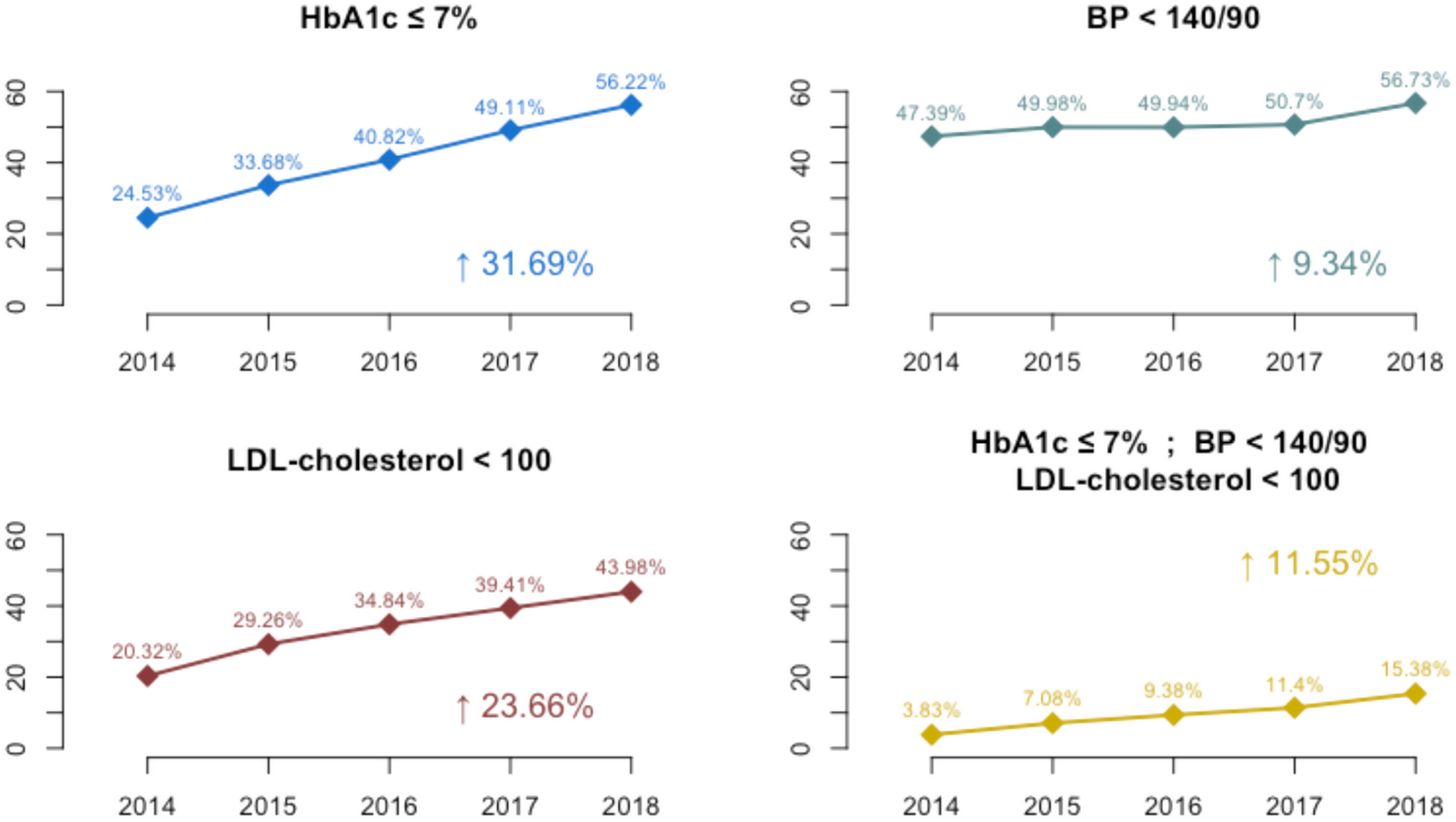
Fig. 2 shows the trends of CVRFs between 2014 and 2018. The trends for HbA1c, blood pressure, and lipid control appeared to be linear. The percentage of people diagnosed with diabetes who achieved glycaemic control (HbA1c level ≤7%) increased from 24.5% to 56.2% between 2014 and 2018. Additionally, the percentage of participants who achieved blood pressure control (≤140/90mm Hg) rose from 47.4% in 2014 to 56.7% in 2018. The percentage of participants who achieved lipid control (LDL cholesterol level≤100mg/dL) also increased, from 20.3% in 2014 to 43.9% in 2018. The percentage of participants who achieved simultaneous glycaemic, blood pressure, and lipid control increased from 3.8% to 15.4% between 2014 and 2018. All of these indicate an improvement in the control of each parameter (glycaemic control, blood pressure, lipid, and multifactorial control) by 31.7%, 9.3%, 23.6%, and 11.6%, respectively.
Cardiovascular risk factor control trends among participants with diagnosed diabetes in the Principality of Asturias between 2014 and 2018. BP=blood pressure; HbA1c=glycated haemoglobin; LDL cholesterol=low-density lipoprotein cholesterol. The percentages were calculated based on the total number of subjects with available data for each cardiovascular risk variable: blood pressure, LDL cholesterol, and %HbA1C.
The real-world evidence revealed by our primary care diabetes study in the Principality of Asturias found that the prevalence of T2DM was 8.01% (95% CI: 7.96–80.6). In line with recent research, the updated estimates in our study showed that glycaemic control improved during the 2014–2018 period, as did lipid control. However, blood pressure control remained stable over the same period. Regarding the multifactorial control of diabetes, the overall degree of control improved substantially between 2014 and 2018.
Our study included all patients with T2DM from a population database of 1,023,011 individuals aged 14 and above, which yielded data from 89,679 patients with diabetes. The accuracy of our methodology was enhanced by the existing link between primary care clinical records and prescriptions obtained from the OMI-AP database. While numerous studies on the treatment of T2DM have been conducted in Northern and Central Europe and North America,12–16 our study is the first to provide data from a region in Northwest Spain that includes data from all patients attending primary care. To our knowledge, some studies have been carried out in Spain, but only in the Mediterranean area,17–19 which is known for its mild and sunny climate, while the north of Spain is cooler and wetter. This can affect the types of lifestyles. Moreover, the Mediterranean diet has been linked to numerous health benefits, including a reduced risk of heart disease and stroke.20,21 Furthermore, our study is population-based and employs RWD to yield its findings.
According to the results shown by this study, the prevalence of T2DM increases with age, which is consistent with what is shown in the literature.22 In Asturias, the adjusted prevalence was 8.01%, which is slightly lower than that reported by IDF in Europe (9.2%), and in South and Central America (9.5%).1 The similarity with the Latin American prevalence could be explained by the high migratory influence from that continent in that age group. Moreover, our data were lower than the data reported by the IDF for the United States, where a prevalence of 14.0% was estimated in adults over 79 years old.1 On the one hand, regarding biological sex, we estimated a higher prevalence in males (9.90%) compared to females (6.50%). These data are similar to those reported by a study carried out in Spain with data corresponding to the year 2016 from the Primary Care Clinical Database (BDCAP).2 This study also reports a prevalence of 5.75% for a representative sample of the population of the Principality of Asturias, which is lower than that reported in our study.2 However, the prevalence reported here is lower than that reported (13.8%) by one of the main population-based epidemiological studies on diabetes carried out in Spain (Di@bet.es study).3,23 These variations may be attributed to the distinct characteristics of each study (real-world data analysis vs. random population sampling) and the discrepancy in participant ages (Di@bet.es study23: mean age, 47.9 years vs. current study, median age: 74.0 years) and that in this study, we are primarily considering patients with type 2 diabetes patients adjusted for the European Standard Population.
The results shown in this study indicate similar or better control of glucose, lipids, and blood pressure in patients with T2DM compared to previous studies conducted in Spain.4,8 The observation of better control of glucose, lipids, and blood pressure in our study could be associated with a potential improvement in the registration of patients with diabetes in the healthcare system. This enhancement in registration allows for more regular monitoring of patients’ conditions and more frequent control tests, leading to early detection of treatment issues and medication adjustments as needed. Furthermore, improved coordination among healthcare professionals facilitated by an enhanced registration system can ensure more comprehensive and personalised care for each patient, ultimately resulting in better health outcomes for people with diabetes. Regarding the control of CVRFs, greater improvements have been observed in cholesterol levels and glycaemic control than in blood pressure, as described in previous reports from the United States and the United Kingdom.24,25 However, this improvement in CVRF control is remarkably superior to what has been described in the United States.26 Differences in healthcare delivery may contribute to variations in control rates.27 This highlights the great utility that large databases provide for studies such as this. At this point, it is important to emphasise that this study includes all individuals diagnosed with T2DM in our region except those covered by private health insurance. To date, only two studies have been conducted in the Principality of Asturias through representative population samplings, and these were carried out more than 10 years ago.28,29 Having access to all the records of the population with diabetes in our region is a differentiating factor when establishing improvement protocols for disease control and management. This is because we can extract all the necessary data (“big data”) from the patient's medical record, in contrast to other studies like Di@bet.es,3 where the information was self-reported or there was a higher participation of women and older individuals, which could have resulted in biased outcomes.
RWD have increasingly been used in diabetes research literature in recent years.30 New therapies, informed by real-world evidence, have revolutionised the management of patients with diabetes with associated cardiovascular disease or risk factors. While previous clinical guidelines primarily focused on meeting specific HbA1c control criteria, recent updates reflect a paradigm shift towards a comprehensive multi-morbidity risk management approach, with a particular emphasis on CVRFs.31 Arterial hypertension, a significant determinant of cardiovascular disease, is influenced by various genetic, dietary and lifestyle factors, alongside biological factors such as hyper-responsiveness to adrenergic stimuli, insulin resistance and endothelial dysfunction. Numerous studies have demonstrated that targeted medical interventions to reduce the prevalence of arterial hypertension can substantially reduce cardiovascular mortality rates.32,33 Our data reveal a consistent improvement in glycaemic control and associated CVRFs over the study period. However, a recent study conducted in the United States, involving adults with diabetes enrolled in the National Health and Nutrition Examination Survey (NHANES), indicated a decline in glycaemic and blood pressure control, while lipid control remained stable.24 Further research is warranted to assess the specific impact of risk factors on individual complications and to explore potential changes following the COVID-19 pandemic or with the introduction of new-generation drugs.
Optimal diabetes management is crucial for improving clinical outcomes and mitigating the risk of serious complications, including reducing hospitalisations for comorbid conditions and overall healthcare costs associated with managing this chronic disease. Over the past three decades, diabetes management has transitioned towards a patient-centred approach, emphasising the role of GPs as the primary point of contact and entry into the healthcare system. Therefore, a person diagnosed with diabetes is referred to diabetes education specialists for education in controlling their disease. The involvement of medical specialists has been considered a basic pillar of optimal diabetes care. At times, it has been questioned whether specialist-based diabetes care is superior to GP-based care. It is important to note that with the increasing prevalence of diabetes and the scarcity of diabetes specialists, the shared-care model of diabetes care delivery between GP and diabetes specialists has become less sustainable.34 Therefore, the optimal treatment of patients with diabetes increasingly requires a more holistic and integrated approach from primary care.35
This study had some limitations that should be described. One of the main restrictions of these data sources is the lack of individual validation of study events. However, other studies utilising OMI-AP data have assessed the integrity and validity of the data regarding the classification of T2DM, yielding positive results.36 Moreover, these limitations can be addressed by comparing the results with those of other population-based databases, such as mortality or cancer registries, hospital databases, databases of comorbidities, or pharmacy billing databases.37–39 Furthermore, it is important to consider that primary care databases may underestimate the true prevalence of T2DM, which could affect the interpretation of the results obtained in this study.40 Another limitation of this study is the incompleteness of the data for the year 2018, as only information up to October 31st was available. Therefore, the prevalence for this year should be contextualised when making comparisons. We define risk factor management using the objectives of clinical guidelines and research available in 2018, but the recommendations have now changed, primarily in the use of pharmacologic treatments for the management of the person with diabetes. Additionally, due to the nature of our work, we can only refer to known T2DM. However, the literature acknowledges that the prevalence of unknown diabetes should also be taken into account.28,41 Furthermore, it emphasizes the importance of evaluating these patient profiles in order to be more specific in diagnosing the disease. Finally, we must consider that, despite excluding the paediatric population in this study, given the characteristics of how data are collected in primary care systems, we may be including a small number of patients with type 1 diabetes under 30 years of age. This situation could affect the generalisation of our findings in extrapolations to this group of patients
Primary care databases, like the one discussed in this paper, offer several advantages over alternative data sources. They afford access to large samples with long-term follow-up at a significantly lower cost compared to traditional cohort or case-control studies. This study, encompassing the entire population, presents the initial data on diagnosed diabetes for biomedical research in the Principality of Asturias. Moreover, the routinely validated data collected are independently verified, a unique feature not found in other studies.42 Furthermore, these databases do not necessitate active patient involvement in data collection and provide highly representative insights into real-world clinical practice. Unlike in other databases, where participation by healthcare professionals is typically voluntary, this study includes all primary care physicians in SESPA. Additionally, these records offer real-time tracking of affected populations, facilitating the formulation of targeted health policies. They also enable proactive screening for T2DM in specific populations, such as those with coronary disease41 or prediabetes.28
In summary, our study utilising real-world data from electronic health records offers valuable insights into the prevalence of type 2 diabetes mellitus (T2DM) in a large population and facilitates real-time management of cardiovascular risks. These data have the potential to guide the development of targeted health policies. Throughout our study, we observed consistent improvements in glycaemic control and associated cardiovascular risk factors each year. However, further research is needed to fully comprehend the impact of these risk factors on specific complications of diabetes. It is essential to evaluate and compare control levels across different age groups, while also identifying associated risk factors to enhance disease management strategies. Leveraging these data would facilitate the formulation of health policies that cater to these specific requirements.
Authors’ contributionsMiguel García-Villarino: formal analysis, investigation, data curation, methodology, visualisation, writing–original draft, writing-review & editing. Carmen Lambert: investigation, methodology, writing-original draft, writing-review & editing. Jesús M. De la Hera: investigation and writing–review & editing. Edelmiro Menéndez-Torre: investigation and writing-review & editing. José María Fernández Rodríguez-Lacín: methodology, data collection, investigation and writing-review & editing. Elías Delgado: supervision, project administration, funding acquisition, investigation and writing-review & editing.
Conflict of interestThe authors declare no competing financial interests.
The authors would like to extend their sincere gratitude to the Sociedad Asturiana de Medicina de Familia y Comunitaria (SAMFyC) for their assistance in signing the confidentiality and data utilisation agreement with the Health Service of the Principality of Asturias (SESPA), which has greatly contributed to the progress of the DaMeDiAs project. Miguel García-Villarino was funded by JANSSEN Cilag SL and ISPA. This study has been funded by Instituto de Salud Carlos III (ISCIII) through projects PI19/01162 and PI22/01125, and co-funded by the European Union and Universidad de Oviedo.