Little is known about the quality of adherence to glucocorticoid replacement therapy in patients with Addison disease (AD). The aim of this study was to evaluate the quality of glucocorticoid treatment adherence in patients with AD and to assess its association with patients’ disease knowledge and quality of life.
MethodsThis is a cross-sectional study including 58 patients with AD. The Girerd questionnaire was used to assess the quality of adherence to glucocorticoid replacement therapy. A questionnaire was specially designed to assess patients’ disease knowledge. The AddiQol questionnaire, specific to AD, was used to assess the patients’ quality of life. Patients were considered non-adherent if they gave three or fewer than three negative answers to the Girerd questionnaire (score≤3/6).
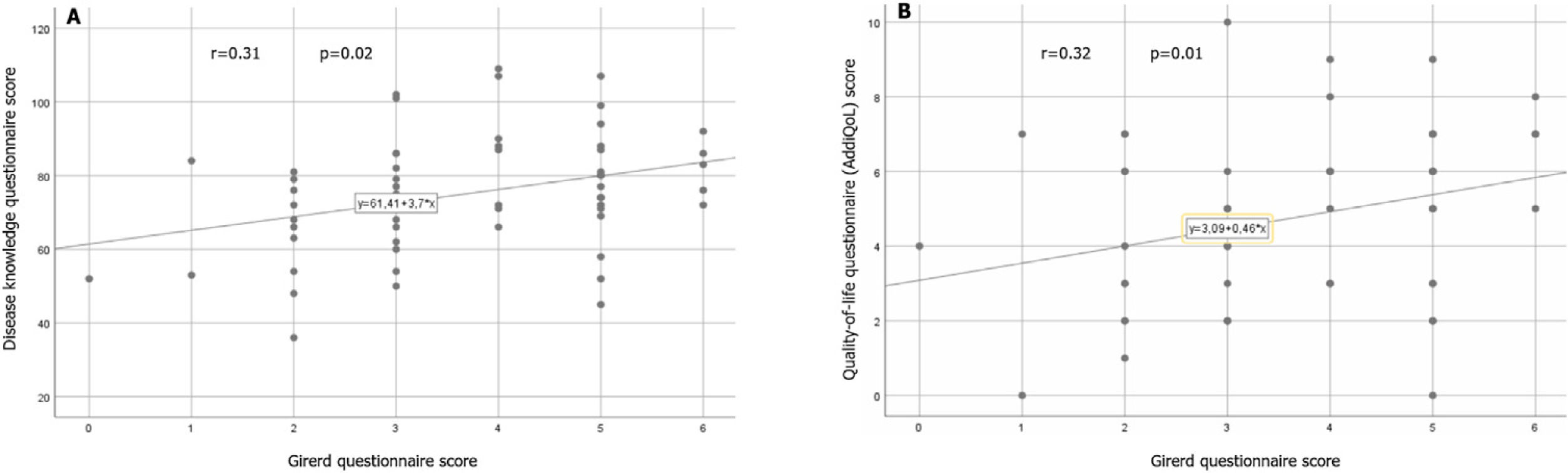
ResultsThe mean age of the patients was 48.4±13.3 years (39 women and 19 men). Twenty-seven patients (46%) were non-adherent to glucocorticoid replacement therapy. An age below 48 years, poor adherence to comorbidity treatments, baseline cortisolemia at diagnosis>5μg/dl, history of adrenal crisis, poor knowledge about the disease, BMI<26.7kg/m2, waist circumference<90cm, low systolic blood pressure, fasting blood glucose<0.9g/l, and triglyceride<1g/l were the factors independently associated with non-adherence (respectively ORa [CI 95%]=4.8 [2.8–10.7], 5.0 [3.0–12.2], 2.3 [1.2–6.2], 4.1 [2.0–8.3], 3.9 [1.2–7.2], 3.9 [1.1–6.9], 1.8 [1.1–2.9], 4.8 [2.6–8.2], 2.5 [1.1–5.3], and 2.2 [1.1–5.1]). There was a positive correlation between the disease knowledge questionnaire score and the Girerd score (p=0.02, r=0.31). There was a positive correlation between the AddiQoL score and the Girerd score (p=0.01, r=0.32).
ConclusionNon-adherence to glucocorticoid replacement therapy was common in patients with AD and was associated with more frequent adrenal crisis and poorer quality of life. The quality of treatment adherence was correlated with patients’ disease knowledge. Therapeutic education is essential to reduce the frequency of non-adherence, especially among young patients.
Se sabe poco acerca de la calidad de la adherencia a la terapia de reemplazo de glucocorticoides en pacientes con enfermedad de Addison (EA). El objetivo de este estudio fue evaluar la calidad de la adherencia al tratamiento con glucocorticoides en pacientes con EA y analizar su asociación con el conocimiento de la enfermedad y la calidad de vida de los pacientes.
MétodosSe trata de un estudio transversal que incluye 58 pacientes con EA. Se utilizó el cuestionario de Girerd para evaluar la calidad de la adherencia al tratamiento sustitutivo con glucocorticoides. Se diseñó un cuestionario especialmente para evaluar el conocimiento de los pacientes sobre la enfermedad. Para evaluar la calidad de vida de los pacientes se utilizó el cuestionario Addi-Qol, específico de la EA. Los pacientes se consideraron no adherentes si dieron 3 o menos de 3 respuestas negativas al cuestionario de Girerd (puntuación≤3/6).
ResultadosLa edad media de los pacientes fue de 48,4±13,3 años (39 mujeres y 19 hombres). Veintisiete pacientes (46%) no cumplieron con la terapia de reemplazo de glucocorticoides. Edad menor de 48 años, mala adherencia a tratamientos de comorbilidades, cortisolemia basal al diagnóstico>5μg/dl, antecedente de crisis suprarrenal, escaso conocimiento de la enfermedad, IMC<26,7kg/m2, perímetro de cintura<90cm, presión arterial sistólica baja, glucemia en ayunas<0,9g/l y triglicéridos<1g/l fueron los factores asociados de forma independiente con la no adherencia (respectivamente ORa[IC 95%]=4,8 [2,8-10,7]; 5,0 [3,0-12,2]; 2,3 [1,2-6,2]; 4,1 [2,0-8,3]; 3,9 [1,2-7,2]; 3,9 [1,1-6,9]; 1,8 [1,1-2,9]; 4,8 [2,6-8,2]; 2,5 [1,1-5,3] y 2,2 [1,1-5,1]). Hubo una correlación positiva entre la puntuación del cuestionario de conocimiento de la enfermedad y la puntuación de Girerd (p=0,02; r=0,31). Hubo una correlación positiva entre la puntuación de AddiQoL y la puntuación de Girerd (p=0,01; r=0,32).
ConclusiónLa falta de adherencia a la terapia de reemplazo de glucocorticoides fue común en pacientes con EA y se asoció con crisis adrenales más frecuentemente y una peor calidad de vida. La calidad de la adherencia al tratamiento se correlacionó con el conocimiento de la enfermedad de los pacientes. La educación terapéutica es fundamental para reducir la frecuencia de la no adherencia, especialmente entre los pacientes jóvenes.
Addison's disease (AD), or primary adrenal insufficiency (PAI), is a rare disease caused by the destruction of the adrenal cortex. It is characterized by glucocorticoid and mineralocorticoid deficiencies1 and its prevalence is between 100 and 140 cases per million.2 Treatment requires lifelong glucocorticoid replacement therapy, which should be taken at fixed times to best mimic the physiological circadian rhythm of cortisol secretion.3,4 Hydrocortisone (HC) is the most used replacement glucocorticoid medication. It is often associated with fludrocortisone. Dehydroepiandrosterone (DHEA) replacement therapy is controversial.3 Treatment adherence is necessary to control the symptoms of the disease and prevent the occurrence of acute adrenal crisis which can be life-threatening.4,5 The incidence of acute adrenal crisis in patients with adrenal insufficiency is between 6 and 8/100 patient years. Its mortality rate is around 6%.6 The main precipitating factor is infection, which is found in 20–30% of cases.7–9 In Germany, discontinuation of glucocorticoid replacement therapy by the patient accounts for 5% of the causes of acute adrenal crisis in patients with adrenal insufficiency.9 Identifying the reasons behind non-adherence to treatment in this population is crucial to best manage this disease and improve its prognosis. Few studies have assessed the quality of treatment adherence in adrenal insufficiency. Only two European studies have addressed this issue with divergent results.10,11 These two studies explored therapeutic adherence in patients with primary and secondary adrenal insufficiency. No studies have assessed therapeutic adherence in patients with PAI specifically. Little is known about the link between treatment adherence and patients’ knowledge about their disease. In this context, in this study we proposed to evaluate the quality of glucocorticoid treatment adherence in patients with PAI, to identify the factors associated with non-adherence, and to determine the relationship between the quality of treatment adherence, the patients’ disease knowledge, and the patient's quality of life (QoL).
MethodsThis is a cross-sectional study conducted in the endocrinology department of La Rabta University Hospital (Tunis – Tunisia) between September 2020 and April 2021. Adult patients (age>18 years) followed and treated for PAI for at least one year were included. The guidelines of the Endocrine Society from 2016 were used to assess the diagnosis of PAI.3 Patients with congenital adrenal hyperplasia, psychiatric illness, and pregnant women were not included. Each patient was asked about their medical history and a physical examination (weight, height, waist circumference and blood pressure) was performed. Written informed consent was obtained from each patient.
Clinical and paraclinical data at diagnosis and during follow-up, glucocorticoid treatment regimens during follow-up, and the number and causes of acute adrenal crisis since the diagnosis were collected from the patient's medical record. The paraclinical data collected were less than twelve months old.
Body mass index (BMI) (kg/m2) and daily HC dose (mg/m2/day) were calculated for each patient. Patients receiving free medical care and patients whose monthly income was less than 500 Tunisian dinars were classified as having a low socioeconomic status. The guaranteed interprofessional minimum wage in Tunisia was 450 Tunisian dinars (143.5 US dollars) in 2022. Patients who were illiterate or had a primary education level were classified as having a low level of instruction. Systolic blood pressure was considered low if it was <90mmHg.
The study was approved by the Ethics Committee of La Rabta Hospital.
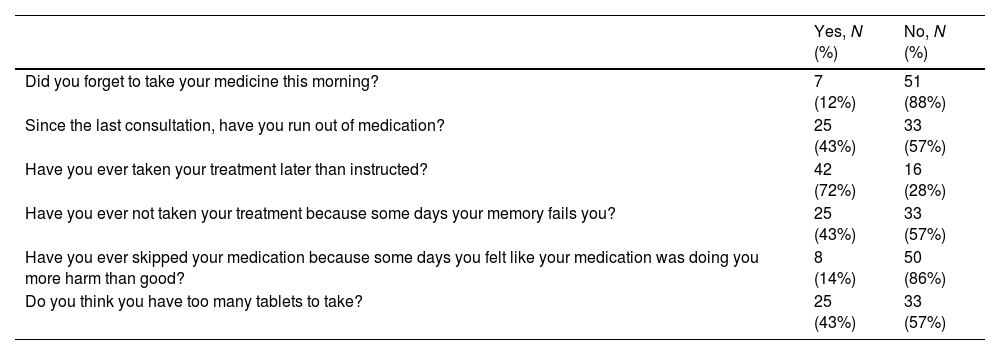
Assessment of adherence to glucocorticoid replacement therapyAdherence to glucocorticoid replacement therapy was assessed using the 6-item self-administered Girerd questionnaire. This questionnaire was established in 2001 by Girerd et al. to assess compliance with antihypertensive treatment.12 It was then used to assess the quality of treatment adherence in other chronic illness. We used in this study the version translated into Arabic and validated in the work of Chelbi et al.13 The questionnaire (Table 1) includes six questions with binary answers (Yes/No) exploring three different dimensions of medication intake (treatment discontinuation, delay in taking medication, and patients’ feelings about the number of drugs taken). A positive answer reflects poor adherence to the considered item. A score of 1 was assigned if the answer to the question was “No” (reflecting good adherence) and 0 if the answer was “Yes” (reflecting poor adherence). A score out of 6 points was established. The higher the score, the better the treatment adherence. Patients were considered adherent if they gave more than three negative answers to the Girerd questionnaire (score>3) and non-adherent if they gave three or fewer than three negative answers to the Girerd questionnaire (score≤3). Full adherence was considered if no positive answer was given to the Girerd questionnaire (score=6).
Distribution of answers to Girerd questionnaire.
| Yes, N (%) | No, N (%) | |
|---|---|---|
| Did you forget to take your medicine this morning? | 7 (12%) | 51 (88%) |
| Since the last consultation, have you run out of medication? | 25 (43%) | 33 (57%) |
| Have you ever taken your treatment later than instructed? | 42 (72%) | 16 (28%) |
| Have you ever not taken your treatment because some days your memory fails you? | 25 (43%) | 33 (57%) |
| Have you ever skipped your medication because some days you felt like your medication was doing you more harm than good? | 8 (14%) | 50 (86%) |
| Do you think you have too many tablets to take? | 25 (43%) | 33 (57%) |
Adherence to medication of the other associated chronic diseases was also assessed by the same questionnaire.
Assessment of patients’ disease knowledgePatients’ disease knowledge was assessed using a questionnaire designed for this study. The conception of the questionnaire and the choice of the domains to explore were inspired by various published articles focusing on the education and evaluation of patient knowledge about PAI.14,15 The questionnaire contains 10 questions (six open-response questions and four multiple-choice questions) written in Tunisian dialect. The domains explored were related to the definition of the disease, its chronic nature, risks of treatment discontinuation, signs of acute adrenal crisis, what to do in the presence of signs of acute adrenal crisis, the need to eat normally salty foods, the need to increase the dose of glucocorticoid in stressful situations, drugs to avoid, possession and use of emergency card for adrenal insufficiency. Patients were considered to have poor knowledge about their disease if they gave fewer than five correct answers to the questionnaire (score<5/10).
Assessment of patients’ quality of lifeThe Addison's disease-specific quality-of-life questionnaire (AddiQoL) was used to assess patients’ QoL.16,17 It is a 30-item questionnaire with a global score ranging from 30 to 120. We used the version translated but not yet validated from English to the Tunisian dialect used by Chihaoui et al. in 2020.18 Different dimensions are explored by the questionnaire: eight questions explore fatigue, eight questions explore the emotional sphere, nine questions explore the symptoms of adrenal insufficiency, and five questions explore various domains, which are sleep, sexuality, and the impact of intercurrent diseases.
A higher score reflects a better health-related QoL. The median of the AddiQoL score (75 points) was used as a cut-off to compare adherence according to the quality of life.
Statistical analysisData were analyzed using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). Data were expressed as means with standard deviations (SD) for quantitative variables and percentages for qualitative variables. The Mann–Whitney U test was used to compare means and Pearson's Chi squared and Fisher's exact tests to compare proportions. Spearman's test was used to assess the correlation between two quantitative variables. The quantitative variables significantly associated with non-adherence were transformed into binary qualitative variables by using the median of the studied variable. The binary regression analysis included the parameters with a p-value<0.2. A p-value<0.05 was considered significant.
ResultsFifty-eight patients (39 women and 19 men) meeting the selection criteria were included. The mean age of patients was 48.4±13.3 years. Thirty-one patients (53%) had at least one comorbidity associated with AD. The most common comorbidities were peripheral hypothyroidism (34%), type 1 diabetes (15%) and hypertension (12%). The mean disease duration was 9.7±10.3 years (range: 1–42 years). The mean number of adrenal crises during follow-up was 0.97±1.6 [0–8]. Autoimmunity was the most common etiology (90%). All the patients were on HC, with a 2-dose regimen in 54 patients (93%) and a 3-dose regimen in four patients (7%). The mean dose of HC was 23.3±7.4mg/day. Sixteen patients (28%) were on fludrocortisone in combination with hydrocortisone. No patient was on dehydroepiandrosterone (DHEA) replacement therapy.
Assessment of adherence to glucocorticoid replacement therapyThe mean score for the Girerd questionnaire was 3.7±1.4/6 (extremes: 0–6). Twenty-seven patients (46%) were non-adherent. Five patients (9%) were fully adherent. Table 1 shows the distribution of answers to the items of the Girerd questionnaire. Delay in medication intake was the most affected domain of adherence.
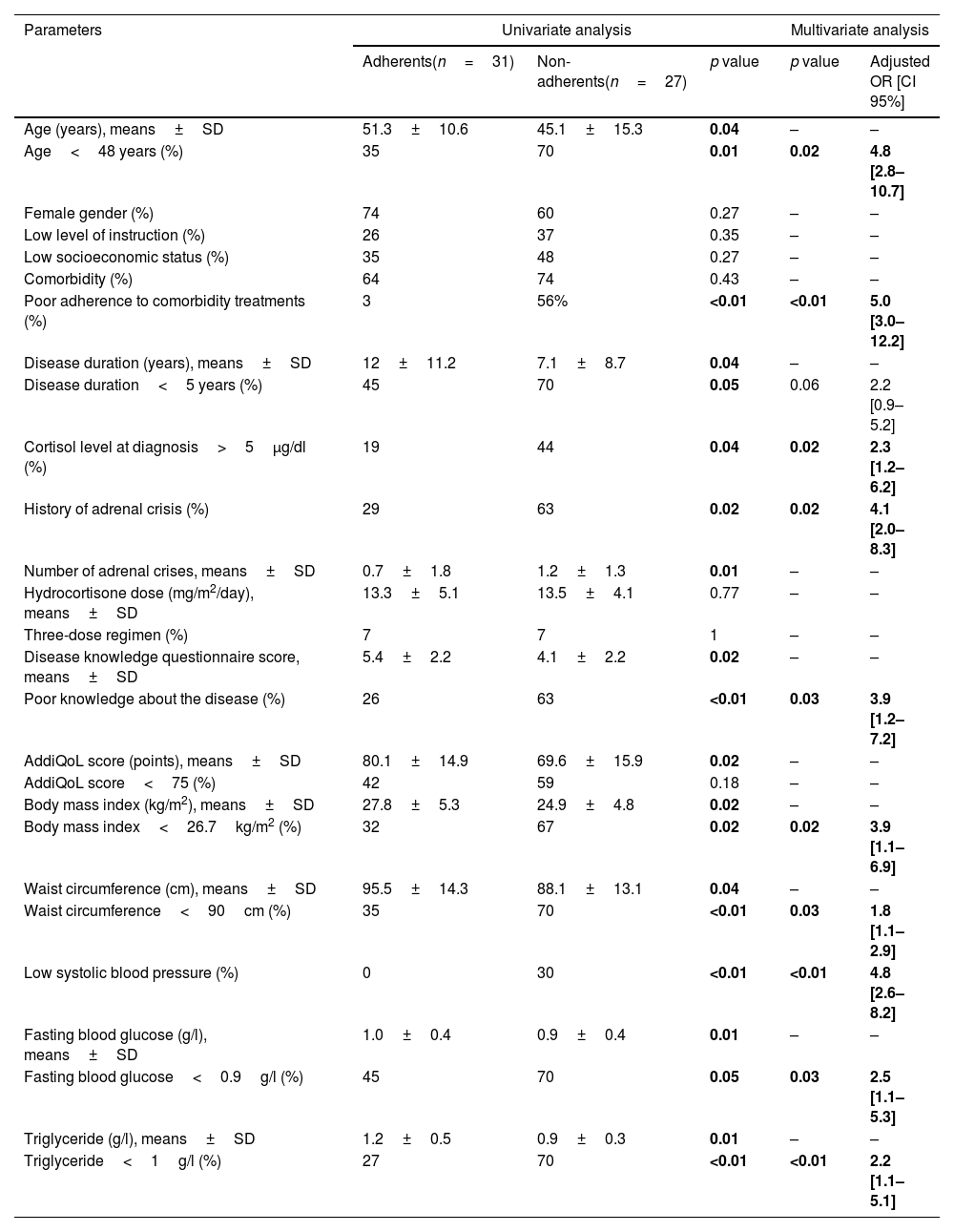
Factors associated with non-adherenceThe factors associated with non-adherence after univariate analysis were younger age, poor adherence to comorbidity treatments, shorter disease duration, higher baseline serum cortisol level at diagnosis, history of adrenal crisis, poor knowledge about the disease, lower AddiQoL score, lower BMI, lower waist circumference, low systolic blood pressure, lower fasting blood glucose, and lower triglyceride level. After multivariate analysis, an age below 48 years, poor adherence to comorbidity treatments, baseline cortisolemia at diagnosis>5μg/dl, history of adrenal crisis, poor knowledge about the disease, BMI<26.7kg/m2, waist circumference<90cm, low systolic blood pressure, fasting blood glucose<0.9g/l, and triglyceride<1g/l were the factors independently associated with non-adherence (Table 2). The daily dose of HC and the treatment regimen (three-dose or two-dose regimen) were not associated with the quality of adherence to glucocorticoid replacement therapy.
Factors associated with non-adherence to glucocorticoid replacement therapy in univariate and multivariate analysis.
| Parameters | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Adherents(n=31) | Non-adherents(n=27) | p value | p value | Adjusted OR [CI 95%] | |
| Age (years), means±SD | 51.3±10.6 | 45.1±15.3 | 0.04 | – | – |
| Age<48 years (%) | 35 | 70 | 0.01 | 0.02 | 4.8 [2.8–10.7] |
| Female gender (%) | 74 | 60 | 0.27 | – | – |
| Low level of instruction (%) | 26 | 37 | 0.35 | – | – |
| Low socioeconomic status (%) | 35 | 48 | 0.27 | – | – |
| Comorbidity (%) | 64 | 74 | 0.43 | – | – |
| Poor adherence to comorbidity treatments (%) | 3 | 56% | <0.01 | <0.01 | 5.0 [3.0–12.2] |
| Disease duration (years), means±SD | 12±11.2 | 7.1±8.7 | 0.04 | – | – |
| Disease duration<5 years (%) | 45 | 70 | 0.05 | 0.06 | 2.2 [0.9–5.2] |
| Cortisol level at diagnosis>5μg/dl (%) | 19 | 44 | 0.04 | 0.02 | 2.3 [1.2–6.2] |
| History of adrenal crisis (%) | 29 | 63 | 0.02 | 0.02 | 4.1 [2.0–8.3] |
| Number of adrenal crises, means±SD | 0.7±1.8 | 1.2±1.3 | 0.01 | – | – |
| Hydrocortisone dose (mg/m2/day), means±SD | 13.3±5.1 | 13.5±4.1 | 0.77 | – | – |
| Three-dose regimen (%) | 7 | 7 | 1 | – | – |
| Disease knowledge questionnaire score, means±SD | 5.4±2.2 | 4.1±2.2 | 0.02 | – | – |
| Poor knowledge about the disease (%) | 26 | 63 | <0.01 | 0.03 | 3.9 [1.2–7.2] |
| AddiQoL score (points), means±SD | 80.1±14.9 | 69.6±15.9 | 0.02 | – | – |
| AddiQoL score<75 (%) | 42 | 59 | 0.18 | – | – |
| Body mass index (kg/m2), means±SD | 27.8±5.3 | 24.9±4.8 | 0.02 | – | – |
| Body mass index<26.7kg/m2 (%) | 32 | 67 | 0.02 | 0.02 | 3.9 [1.1–6.9] |
| Waist circumference (cm), means±SD | 95.5±14.3 | 88.1±13.1 | 0.04 | – | – |
| Waist circumference<90cm (%) | 35 | 70 | <0.01 | 0.03 | 1.8 [1.1–2.9] |
| Low systolic blood pressure (%) | 0 | 30 | <0.01 | <0.01 | 4.8 [2.6–8.2] |
| Fasting blood glucose (g/l), means±SD | 1.0±0.4 | 0.9±0.4 | 0.01 | – | – |
| Fasting blood glucose<0.9g/l (%) | 45 | 70 | 0.05 | 0.03 | 2.5 [1.1–5.3] |
| Triglyceride (g/l), means±SD | 1.2±0.5 | 0.9±0.3 | 0.01 | – | – |
| Triglyceride<1g/l (%) | 27 | 70 | <0.01 | <0.01 | 2.2 [1.1–5.1] |
SD: standard deviation; OR: odds ratio; CI: confidence interval; AddiQoL: Addison's disease-specific quality-of-life questionnaire. Significant results are shown in bold.
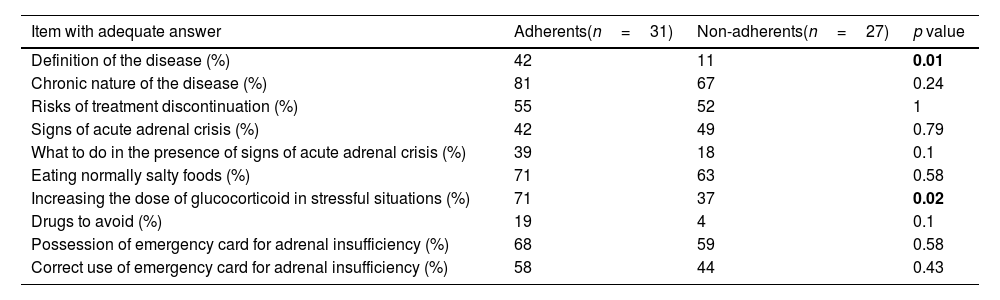
Twenty-five patients (43%) had a poor level of knowledge about their disease. The disease knowledge questionnaire score was significantly lower in non-adherent patients (p=0.02). Poor knowledge about the disease (questionnaire score<5/10) was independently associated with non-adherence (adjusted OR [CI 95%]=3.9 [1.2–7.2]) (Table 2). There was a positive correlation between the disease knowledge questionnaire score and the Girerd score (Fig. 1A). Table 3 shows the proportion of adequate answers in each item assessed by the disease knowledge questionnaire according to the quality of adherence to glucocorticoid replacement therapy. Disease definition and the need to increase glucocorticoid dose in stressful situations were the items significantly associated with a lower proportion of adequate answers in non-adherent patients.
Proportion of adequate answers in the items of the disease knowledge questionnaire according to adherence to glucocorticoid replacement therapy.
| Item with adequate answer | Adherents(n=31) | Non-adherents(n=27) | p value |
|---|---|---|---|
| Definition of the disease (%) | 42 | 11 | 0.01 |
| Chronic nature of the disease (%) | 81 | 67 | 0.24 |
| Risks of treatment discontinuation (%) | 55 | 52 | 1 |
| Signs of acute adrenal crisis (%) | 42 | 49 | 0.79 |
| What to do in the presence of signs of acute adrenal crisis (%) | 39 | 18 | 0.1 |
| Eating normally salty foods (%) | 71 | 63 | 0.58 |
| Increasing the dose of glucocorticoid in stressful situations (%) | 71 | 37 | 0.02 |
| Drugs to avoid (%) | 19 | 4 | 0.1 |
| Possession of emergency card for adrenal insufficiency (%) | 68 | 59 | 0.58 |
| Correct use of emergency card for adrenal insufficiency (%) | 58 | 44 | 0.43 |
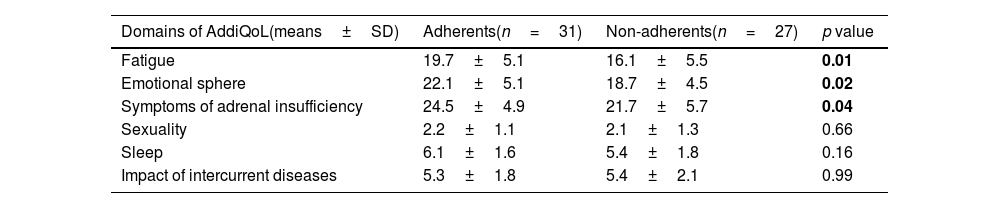
The AddiQoL score was significantly lower in non-adherent patients (p=0.02) (Table 2). There was a positive correlation between the AddiQoL score and the Girerd score (Fig. 1B). Table 4 shows the scores by domains in adherent and non-adherent patients. Fatigue, emotional sphere, and adrenal insufficiency symptoms domain scores were significantly lower in non-adherent patients.
Mean scores in the domains explored by the quality-of-life questionnaire (AddiQoL) according to adherence to glucocorticoid replacement therapy.
| Domains of AddiQoL(means±SD) | Adherents(n=31) | Non-adherents(n=27) | p value |
|---|---|---|---|
| Fatigue | 19.7±5.1 | 16.1±5.5 | 0.01 |
| Emotional sphere | 22.1±5.1 | 18.7±4.5 | 0.02 |
| Symptoms of adrenal insufficiency | 24.5±4.9 | 21.7±5.7 | 0.04 |
| Sexuality | 2.2±1.1 | 2.1±1.3 | 0.66 |
| Sleep | 6.1±1.6 | 5.4±1.8 | 0.16 |
| Impact of intercurrent diseases | 5.3±1.8 | 5.4±2.1 | 0.99 |
The present study is the first to assess AD patient's adherence to glucocorticoid replacement therapy, and to explore its association with patients’ disease knowledge and QoL. The Girerd questionnaire was used to assess the quality of adherence to glucocorticoid replacement therapy. A questionnaire was specially designed to assess patients’ level of knowledge about their disease. The AddiQol questionnaire, specific to AD, was used to assess the patients’ QoL. The study is, however, limited by the small sample size, which is essentially related to the rarity of the disease. In addition, the patients’ disease knowledge questionnaire and the Tunisian dialect version of the AddiQoL questionnaire have not yet been validated.
Prevalence of non-adherence to glucocorticoid replacement therapy in ADNon-adherence to glucocorticoid replacement therapy was noted in 46% of the patients. Only 9% had full adherence. Delay in medication intake was the most affected domain of adherence. Forgetting to take treatment, unavailability of drugs, and patient's bad feeling about the number of drugs to take were reported by nearly half of the patients. Little is known about the quality of adherence to hormonal treatment in AD (PAI). No studies have assessed therapeutic adherence in patients with PAI specifically. Two studies assessed the quality of treatment adherence and self-management of the disease in both patients with secondary and PAI. The first study is that of Chapman et al. published in 2016, and conducted in 81 patients with secondary and PAI from 5 European countries.10 The prevalence of non-adherence to glucocorticoid replacement therapy was higher than in our study, with a frequency of 85.2%. The questionnaire used to assess the quality of treatment in this study was the modified MARS (Medication Adherence Report Scale) questionnaire composed of eight items assessing both attitudes about medications and actual medication-taking behavior.19 The second study, published in 2016, is that of Van Eck et al., conducted in the Netherlands in 52 patients with PAI and 64 patients with secondary adrenal insufficiency. Therapeutic adherence was assessed using a pre-established questionnaire designed for the study. The score for medication adherence was considered high by the authors, reflecting good adherence to glucocorticoid replacement therapy.11
Association between adherence and patients’ disease knowledgeNumerous studies have shown that the level of knowledge in patients with adrenal insufficiency was poor or unsatisfactory.16,20,21 In our study, the prevalence of patients with a poor level of knowledge about the disease concerned around four out of 10 patients. The relationship between treatment adherence and patient's knowledge about their disease is well demonstrated in many chronic diseases22 but no studies have investigated this relationship in patients with PAI. The study of Chapman et al. examined the association between adherence to glucocorticoid replacement therapy, illness perception, and concerns about treatment in patients with secondary and PAI. The authors found that patients who expressed dissatisfaction with information about glucocorticoids and concerns about their adverse effects were more likely to be non-adherent.10 In the present study, a positive and significant correlation between adherence questionnaire score and patients’ disease knowledge questionnaire score was observed. Thus, the higher the level of knowledge, the better the adherence to treatment was. Disease definition and the need to increase glucocorticoid dose in stressful situations were less well known by non-adherent patients.
Association between adherence and patients’ quality of lifeNo study has explored the association between treatment adherence and QoL. In the present study, a positive and significant correlation between treatment adherence score and patients’ QoL score was observed. Thus, the QoL would be poorer in non-adherent patients with AD. The cross-sectional design of the study does not allow us to conclude whether it is the QoL that influences the quality of treatment adherence or the opposite. However, it has been demonstrated that underexposure to cortisol was associated with poor QoL.23,24 The QoL domains associated with non-adherence were fatigue, emotional sphere, and symptoms of adrenal insufficiency. Accordingly, non-adherence leading to underexposure to cortisol may result in fatigue and higher frequency of symptoms’ disease.
Other factors associated with non-adherence to glucocorticoid replacement therapyNon-adherence to glucocorticoid replacement therapy was more common in younger patients. Chapman et al. and Van Eck et al. found similar results.10,11 In studies focusing on the quality of treatment adherence in other chronic diseases, non-adherence was often more frequent among the youngest.25 Non-acceptance of the disease in younger patients may explain these results. We also demonstrated that poor adherence to comorbidity treatments was associated with poor adherence to glucocorticoid replacement therapy. This suggests that common factors, independent of the disease and the nature of the medications, influence the quality of treatment adherence.
Non-adherence to glucocorticoid replacement therapy was also more frequent in patients with higher cortisol level at diagnosis. This may reflect residual endogenous cortisol production, allowing occasional drug intake without clinical consequences in these patients.26 It has been described in several studies that the more severe the clinical signs of the disease were, the better the adherence to the treatment in chronic diseases was.27,28
In addition, non-adherent patients had lower systolic blood pressure, BMI, waist circumference, glucose, and triglyceride levels than adherent patients. To date, there are no studies that have assessed the relationship between the cardio-metabolic parameters and the quality of treatment adherence in AD. However, the correlation between serum cortisol level, blood pressure, glucose level and lipid profile is well known. Cortisol deficiency leads to a decrease in gluconeogenesis with an increase in insulin sensitivity.29 Mineralocorticoid deficiency causes hypovolemia and glucocorticoid deficiency decreases renin synthesis leading to a decrease in blood pressure.29 Underexposure to cortisol in non-adherent patients could, therefore, explain these results.
Finally, adrenal crisis was more frequent in non-adherent patients. This is an expected result since the glucocorticoid replacement therapy is necessary to avoid this serious complication.
ConclusionNon-adherence to glucocorticoid replacement therapy was common in patients with AD and was associated with more frequent adrenal crisis and poorer QoL. Patients’ disease knowledge was correlated with the quality of treatment adherence. Therefore, therapeutic education is essential to reduce the frequency of non-adherence, especially among young patients, who are more likely to be non-adherent. Non-adherence should be suspected in patients with low systolic blood pressure and low glucose and triglyceride levels.
Availability of dataData are available on request due to ethical reasons.
Informed consentWritten informed consent was obtained from each patient.
Ethical approvalThe study was approved by the Ethics Committee of La Rabta Hospital.
FundingThe study required no external funding.
Conflicts of interestNone.