Due to its effect on patient health and healthcare resources, the study of diabetic foot is essential. Despite the existence of classification and grading systems, further evidence is required. Current systems are prone to a lack of validation in specific populations, inadequate consideration of regional variations, and an incomplete evaluation of risk factors and outcomes. The prevalence and complications of diabetes, such as diabetic foot, are on the rise worldwide, necessitating regionally specific research. To fill these gaps, this study focuses on a Southeast Asian subpopulation.
ObjectiveThe study aims to evaluate the clinical characteristics of diabetic foot patients using the WIfI classification system, and to develop a risk calculator for patients to predict and evaluate potential outcomes.
MethodsA retrospective analysis was conducted on the medical records of patients with diabetic foot who visited a tertiary hospital in Vietnam between December 2021 and July 2022. Demographic data, clinical characteristics, and outcomes were collected and classified according to the WIfI (Wound, Ischemia, and foot Infection) classification system. Descriptive statistics were used to analyze the data, and a multivariable logistic regression model was employed to develop a risk calculator.
ResultsThe study included 60 patients with diabetic foot. Gender distribution was similar (56.7% male), with a mean age of 44 years. Most patients had ulcers of varying degrees, while ischemia contributed to higher grades, placing 43.3% at moderate-to-high risk of amputation (stages 3 and 4). HbA1c positively correlated with amputation risk (p<0.05), while ABI, TBI, and TP showed inverse correlations (p<0.001). The amputation risk equation based on the WIfI scale was: risk=3.701−0.788ABI−1.260TP. A risk calculator was developed using these predictors to estimate adverse outcomes.
ConclusionIn diabetic foot patients, early identification and management of risk factors are crucial. The findings of this study highlight the importance of ischemia and its association with amputation risk. Incorporating HbA1c, ABI, and TP, the risk calculator enables personalized assessments of amputation risk, thereby assisting healthcare professionals in treatment planning. Further validation and refinement of the risk calculator is required for broader clinical application.
Debido a su impacto en la salud del paciente y en los recursos sanitarios, el estudio del pie diabético reviste una importancia fundamental. A pesar de la existencia de sistemas de clasificación y gradación, es necesario recopilar más datos científicos. Los sistemas actuales son propensos a una falta de validación en poblaciones específicas, una consideración inadecuada de las variantes regionales y una evaluación incompleta de los factores de riesgo y los desenlaces. La prevalencia y las complicaciones de la diabetes, como el pie diabético, están aumentando en todo el mundo, lo que exige la realización de investigaciones específicas en cada región. Para solventar estas lagunas, este estudio se centra en una población del Sudeste Asiático.
ObjetivoEl estudio pretende evaluar las características clínicas de los pacientes con pie diabético utilizando el sistema de clasificación WIfI y desarrollar una calculadora de riesgo para los pacientes para predecir y evaluar los posibles desenlaces.
MétodosSe realizó un análisis retrospectivo de las historias clínicas de los pacientes con pie diabético que visitaron un hospital de atención terciaria en Vietnam entre diciembre del 2021 y julio del 2022. Se recogieron datos demográficos, características clínicas y desenlaces, que se clasificaron según el sistema de clasificación WIfI (heridas, isquemia e infección del pie, por sus siglas en inglés). Se utilizaron estadísticos descriptivos para analizar los datos y se empleó un modelo de regresión logística multivariable para desarrollar una calculadora de riesgo.
ResultadosEl estudio incluyó a 60 pacientes con pie diabético. La distribución de géneros fue similar (56,7% varones), con una media de edad de 44 años. La mayor parte de los pacientes tenían úlceras de diversos grados, mientras que la isquemia contribuía a unos grados más altos, situando a un 43,3% de los pacientes en un riesgo de amputación de moderado a alto (estadios 3 y 4). La HbA1c presentaba una correlación positiva con el riesgo de amputación (p <0,05), mientras que el índice tobillo-brazo (ABI), el índice dedo del pie-brazo (TBI) y la presión en el dedo del pie (TP) mostraban correlaciones inversas (p <0,001). La ecuación del riesgo de amputación basada en la escala WIfI fue: riesgo=3,701-0,788 ABI-1,260T P. Se desarrolló una calculadora de riesgo utilizando estos factores predictivos para estimar los desenlaces desfavorables.
ConclusiónEn pacientes con pie diabético, la identificación precoz y la gestión de los factores de riesgo resultan cruciales. Los resultados de este estudio subrayan la importancia de la isquemia y su asociación con el riesgo de amputación. Al incorporar la HbA1c, el índice ABI y la TP, la calculadora de riesgo permite una evaluación personalizada del riesgo de amputación, ayudando de este modo a los profesionales sanitarios en la planificación del tratamiento. Es necesario seguir validando y perfeccionando la calculadora de riesgo para una aplicación clínica más amplia.
Diabetic foot is a serious diabetes complication with serious health, economical, and societal consequences. Millions of people worldwide are affected by diabetic foot, which has a considerable influence on the patient's health and well-being, as well as the financial burden on the individual, their family, and society as a whole. Diabetic foot is characterized by ulcers, infections, and other foot-related disorders, owing to neuropathy and ischemia in the feet and legs. A major concern for patients and doctors is that this condition may result in amputation. The amputation rate among these patients is fairly high. For instance, Wukich et al. (2013) found an amputation rate of 51%, while Richard et al. (2011) found a 48% rate of amputation.1,2 This value can vary from 40% risk of major amputation up to 73%, taking into account minor amputation in emergency situations.1–3 Consequently, diabetic foot can adversely affect diabetes patients’ physical, emotional, and financial health, including reduced mobility, prolonged hospital stays, impaired quality of life, escalated healthcare expenses and other social burdens. Timely management and preventative strategies are vital to decreasing the disease's burden on individuals, families, and society as a whole.
The complexity of diabetic foot etiology compels an integrated classification strategy. The WIfI classification system is a relatively new classification system that was introduced by the European Society of Vascular Surgeons in 2014 to address the limitations of previous classification systems in predicting the risk of significant amputation among diabetic foot patients. The WIfI classification system relies on three compartments: wound (W), ischemia (I), and foot infection (fI) to assess the risk of amputation within 6 months or 1 year.4–8 It evaluates the size, depth, and severity of the wound, the ankle-brachial index or toe-brachial index to determine the extent of ischemia, and the foot infection status using the IDSA classification.
This adapts to the conventional Wagner and Texas classifications, which disregard the severity of infection or ischemia.3 The Fontaine and Rutherford classifications are also helpful but they may underestimate the severity of infection and wound characteristics, which have been addressed by the WIfI classification.6,8 Similarly, the Infectious Diseases Society of America (IDSA) classification lends weight to infection status but does not account for ischemia or other lesion characteristics.9 The WIfI system addresses this issue by incorporating the IDSA classification as a part of the grading procedure. Interestingly, the PEDIS classification system appears to be more comprehensive when multiple factors, such as neuropathy, infection, and ischemia, are considered, but it is too complex for routine clinical purposes.3,10 Acknowledging the perspective, the WIfI classification system is easy to use and readily applicable in clinical practice. The system's simplicity makes it an ideal instrument for use in clinical contexts where swift assessments are required. In addition, the WIfI grading also helps to predict ulcer healing in diabetic foot disease. Weaver et al. have shown that the ulcer healing rate of stages 1 and 2 WIfI is much higher than stages 3 and 4, with the figures of 77.3% versus 57.2%, respectively.8 However, a potential limitation of the WIfI classification system is that it does not account for other important factors that may contribute to the risk of significant amputation in diabetic foot patients, such as the presence of gangrene or other comorbidities. The recent nature of WIfI requires additional time and data among different populations with diverse backgrounds to reinforce its pros and cons.
This research aims to advance the field of diabetic foot management by characterizing patients comprehensively using the WIfI categorization system. By investigating the factors associated with the WIfI category in individuals with diabetic foot disease, this study offers crucial insights into the progression and severity determination of the disease. In addition, the study transcends its immediate context by establishing the groundwork for the creation of a risk calculator prototype designed specifically for diabetic foot patients worldwide. This novel approach has the potential to improve early risk assessment and personalized care, not only in the Vietnamese community, but also in other populations. By bridging the gap between theoretical knowledge and practical application, this study contributes substantially to the existing literature, and addresses a pressing issue in diabetic foot management.
Research subjects and methodsSubjectThe study aimed to include diabetic patients with foot disease who sought treatment at Hue Central Hospital from December 19, 2021 to July 29, 2022. The sample size for this study was determined to be 60 patients, based on feasibility considerations and the available resources.
EligibilityDiagnostic criteriaThe diagnostic criteria for diabetic foot disease were established based on clinical guidelines and consensus. Patients were diagnosed with diabetic foot disease if they presented with one or more of the following: foot ulcers, infections, gangrene, or ischemia. The specific diagnostic criteria used for the classification of diabetic foot disease were documented in the patients’ medical records.
Exclusion criteriaPatients with incomplete or missing medical records were excluded from the study. This exclusion criterion was implemented to ensure the accuracy and comprehensiveness of the data collected for analysis.
MethodologyThis study followed a descriptive cross-sectional design. The data collection process involved utilizing convenience sampling, where all qualified patients who met the inclusion criteria were included in the study. This approach aimed to ensure the representation of the diabetic foot population at Hue Central Hospital during the specified time period.
Main variablesThe main variables of interest in this study included the WIfI classification system, ankle-brachial index (ABI), toe-brachial index (TBI), toe pressure (TP), and white blood cell count (WBC). These variables were assessed and measured according to the guidelines provided by the European Society of Vascular Surgery (SVS) in 2014. The WIfI classification system was utilized to evaluate the severity of the disease and classify patients into appropriate risk categories.
Furthermore, the study also considered the goal of controlling blood glucose levels, serum lipid levels, HbA1c (glycated hemoglobin), and plasma glucose indices. These parameters were managed in accordance with the guidelines outlined in the American Diabetes Association's (ADA) Standards of Medical Care in Diabetes for 2022.
Data collectionData regarding the aforementioned variables were collected from patients’ medical records and clinical examinations conducted during their hospital visits. The collected data were recorded in a structured format to facilitate analysis and interpretation.
Data analysisStatistical analysis was performed using SPSS 20.0 software. Univariate relationships between variables were assessed using the Pearson's χ2 test. The significance level was set at p<0.05 to determine statistically significant associations. Additionally, multivariable logistic regression analysis was conducted to identify factors related to the outcomes of interest, such as amputation risk and disease severity.
By employing these robust methods, the study aimed to comprehensively evaluate the clinical characteristics of diabetic foot patients and explore the factors associated with disease severity and amputation risk. The analysis of these variables will contribute to a deeper understanding of diabetic foot pathology and aid in the development of targeted interventions for improved patient outcomes.
EthicsThe study adhered to ethical considerations by ensuring patient confidentiality and obtaining informed consent. The research protocol was reviewed and approved by the institutional review board or ethics committee of Hue University of Medicine and Pharmacy.
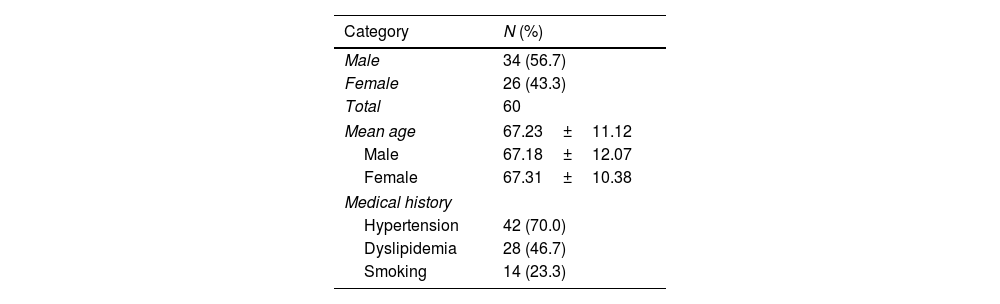
Results and discussionDemographic characteristicsTable 1 provides a comprehensive summary of the demographic characteristics of the patients. The study included a total of 60 participants, with a greater proportion of males (56.7%) than females (43.3%). The average age of our study participants was calculated to be 67.23±11.12 years. Notably, the average age of the female subjects was 67.31±10.38 years, while the average age of the male subjects was 67.18±12.07 years. The majority of patients had a history of other coexisting conditions in addition to diabetes, including hypertension, which affected approximately 71% of the subjects, and dyslipidemia, which affected 46.7% of the individuals. The significance of considering these comorbidities alongside diabetes in the context of the study population is highlighted by these results.
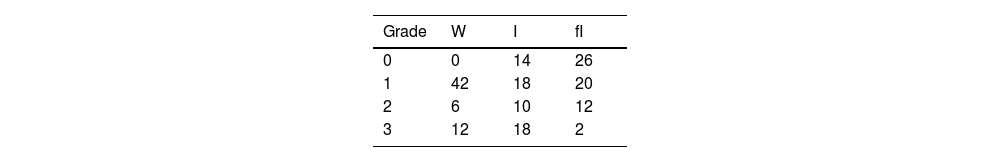
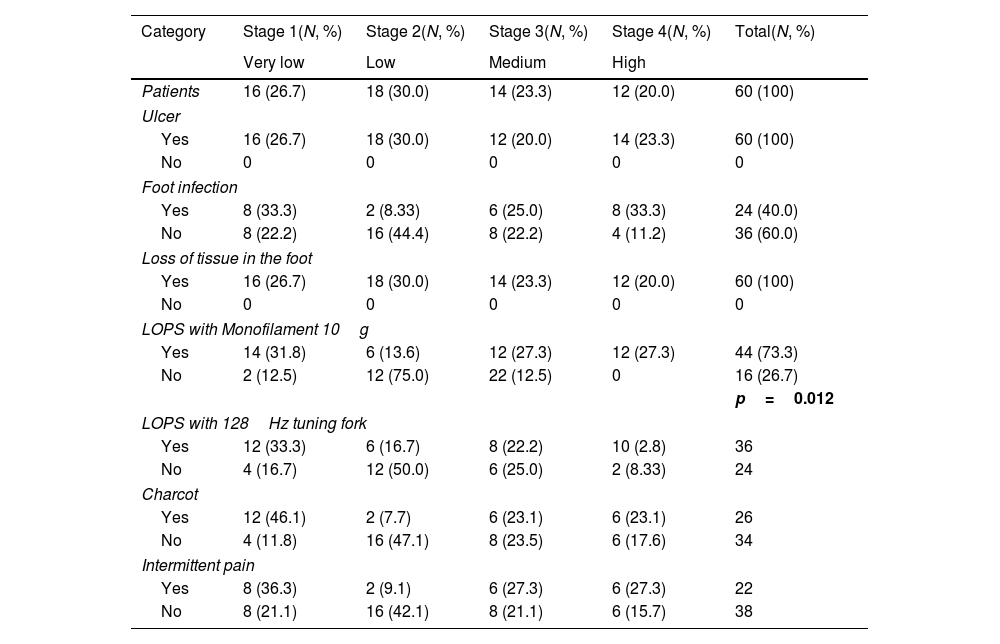
Clinical and subclinical manifestations according to the WIfI classificationTables 2–5 summarize key findings of this study regarding clinical and laboratory indices. The analysis of the WIfI classification components revealed that most patients in the study had ulcers/wound (W) of varying degrees; however, when examining the severity of the disease, component I (ischemia) was found to be more prevalent at grade 2 and grade 3, indicating a significant impact on the disease progression.
Clinical characteristics and risk of amputation among participants, according to the WIfI classification.
| Category | Stage 1(N, %) | Stage 2(N, %) | Stage 3(N, %) | Stage 4(N, %) | Total(N, %) |
|---|---|---|---|---|---|
| Very low | Low | Medium | High | ||
| Patients | 16 (26.7) | 18 (30.0) | 14 (23.3) | 12 (20.0) | 60 (100) |
| Ulcer | |||||
| Yes | 16 (26.7) | 18 (30.0) | 12 (20.0) | 14 (23.3) | 60 (100) |
| No | 0 | 0 | 0 | 0 | 0 |
| Foot infection | |||||
| Yes | 8 (33.3) | 2 (8.33) | 6 (25.0) | 8 (33.3) | 24 (40.0) |
| No | 8 (22.2) | 16 (44.4) | 8 (22.2) | 4 (11.2) | 36 (60.0) |
| Loss of tissue in the foot | |||||
| Yes | 16 (26.7) | 18 (30.0) | 14 (23.3) | 12 (20.0) | 60 (100) |
| No | 0 | 0 | 0 | 0 | 0 |
| LOPS with Monofilament 10g | |||||
| Yes | 14 (31.8) | 6 (13.6) | 12 (27.3) | 12 (27.3) | 44 (73.3) |
| No | 2 (12.5) | 12 (75.0) | 22 (12.5) | 0 | 16 (26.7) |
| p=0.012 | |||||
| LOPS with 128Hz tuning fork | |||||
| Yes | 12 (33.3) | 6 (16.7) | 8 (22.2) | 10 (2.8) | 36 |
| No | 4 (16.7) | 12 (50.0) | 6 (25.0) | 2 (8.33) | 24 |
| Charcot | |||||
| Yes | 12 (46.1) | 2 (7.7) | 6 (23.1) | 6 (23.1) | 26 |
| No | 4 (11.8) | 16 (47.1) | 8 (23.5) | 6 (17.6) | 34 |
| Intermittent pain | |||||
| Yes | 8 (36.3) | 2 (9.1) | 6 (27.3) | 6 (27.3) | 22 |
| No | 8 (21.1) | 16 (42.1) | 8 (21.1) | 6 (15.7) | 38 |
LOPS: loss of protective sensation.
Laboratory indices and risk of amputation among participants, according to the WIfI classification.
| Category | Stage 1(N) | Stage 2(N) | Stage 3(N) | Stage 4(N) | Total(N) |
|---|---|---|---|---|---|
| Very low | Low | Medium | High | ||
| Plasma glucose | |||||
| <7.2mmol/L | 2 | 0 | 2 | 2 | 6 |
| ≥7.2mmol/L | 14 | 18 | 12 | 10 | 54 |
| HbA1C | |||||
| <7% | 12 | 14 | 4 | 2 | 32 |
| ≥7% | 4 | 4 | 10 | 10 | 28 |
| p=0.035 | |||||
| LDL cholesterol | |||||
| <1.8mmol/L | 6 | 2 | 10 | 4 | 22 |
| ≥1.8mmol/L | 10 | 16 | 4 | 8 | 38 |
| Triglycerides | |||||
| <1.7mmol/L | 8 | 16 | 10 | 10 | 44 |
| ≥1.7mmol/L | 8 | 2 | 4 | 2 | 12 |
| WBC | |||||
| <4K/mcL | 0 | 0 | 0 | 0 | 0 |
| 4–12K/mcL | 12 | 18 | 10 | 10 | 50 |
| >12K/mcL | 4 | 0 | 4 | 2 | 10 |
HbA1c: glycated haemoglobin; LDL: low-density lipoprotein; WBC: White Blood Cells.
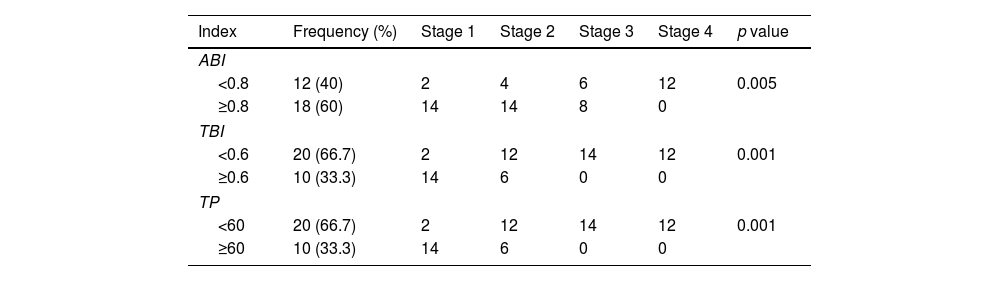
ABI, TBI and TP of the study subjects according to the stages of the WIfI classification.
| Index | Frequency (%) | Stage 1 | Stage 2 | Stage 3 | Stage 4 | p value |
|---|---|---|---|---|---|---|
| ABI | ||||||
| <0.8 | 12 (40) | 2 | 4 | 6 | 12 | 0.005 |
| ≥0.8 | 18 (60) | 14 | 14 | 8 | 0 | |
| TBI | ||||||
| <0.6 | 20 (66.7) | 2 | 12 | 14 | 12 | 0.001 |
| ≥0.6 | 10 (33.3) | 14 | 6 | 0 | 0 | |
| TP | ||||||
| <60 | 20 (66.7) | 2 | 12 | 14 | 12 | 0.001 |
| ≥60 | 10 (33.3) | 14 | 6 | 0 | 0 | |
ABI: Ankle/Brachial Index; TBI: Toe/Brachial Index; TP: The resting systolic toe pressure.
When assessing the amputation risk based on the WIfI classification, it was found that 26.7% of hospitalized patients were at a very low risk, 30% at low risk, 23.3% at medium risk, and 20% at high risk of amputation. This highlights the importance of early identification and risk stratification in diabetic foot patients to provide appropriate interventions and prevent adverse outcomes.
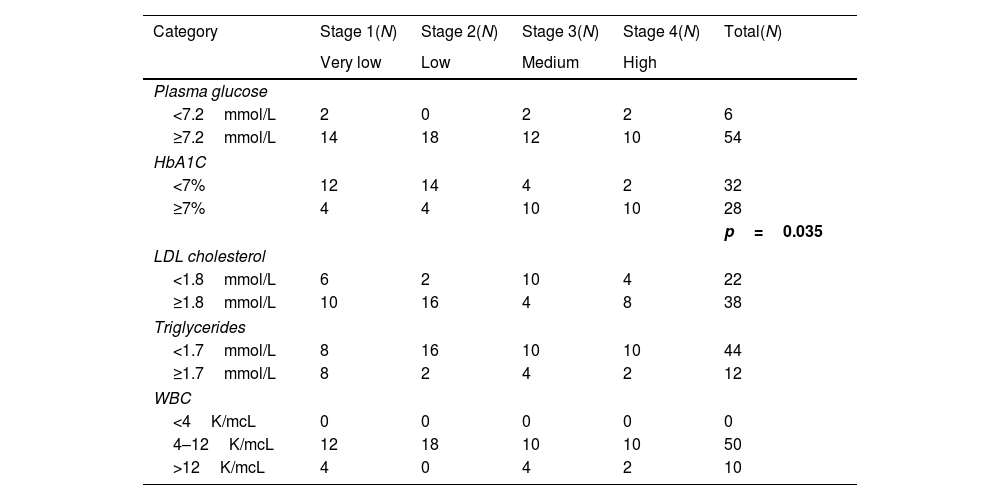
In terms of risk factors, the study revealed significant associations between HbA1c (glycated hemoglobin) levels≥7% and the risk levels according to the amputation stage in patients with diabetic foot (p=0.035). Elevated HbA1c levels indicate poor glycemic control and are associated with increased risk of amputation. Additionally, ABI (ankle-brachial index)≥0.8, TBI (toe-brachial index)≥0.6, and TP (toe pressure)≥60mmHg were all found to be statistically significant predictors of the risk stages of limb amputation according to the WIfI classification (with p-values of 0.05, 0.01, and 0.01, respectively). Lower values of these parameters indicate impaired blood flow and decreased tissue perfusion, which contribute to the risk of amputation in diabetic foot patients.
The study also highlighted the significance of the Monofilament Foot Sensory Examination method in detecting loss of protective sensation (LOPS) across different stages of diabetic foot (p=0.012). This emphasizes the importance of regular sensory assessments in identifying patients at risk of foot complications and implementing appropriate preventive measures.
Overall, the findings of this study provide valuable insights into the characteristics and risk factors associated with diabetic foot, specifically utilizing the WIfI classification. The identification of HbA1c levels, ABI, TBI, and TP as significant predictors of amputation risk underscores the importance of comprehensive risk assessment in diabetic foot management. These findings have implications for improving risk stratification, developing targeted interventions, and ultimately reducing the burden of amputations in diabetic foot patients. Further research and validation studies are warranted to confirm these findings and enhance our understanding of diabetic foot management.
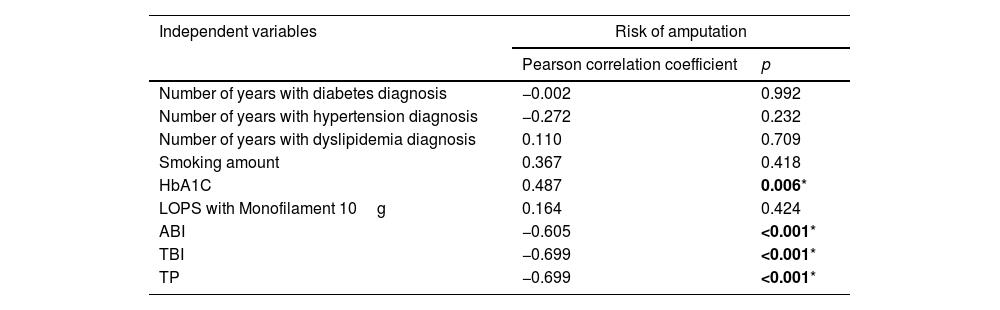
Relationship between stages of the WIfI classification and risk factorsIn the statistical analysis, it was found that HbA1c (glycated hemoglobin) levels were positively correlated with the risk of amputation (p<0.05). This indicates that higher HbA1c levels are associated with an increased likelihood of amputation in patients with diabetic foot. On the other hand, variables such as ABI, TBI, and TP showed an inverse correlation with the risk of amputation (p<0.001). Lower values of these variables were associated with a higher risk of amputation.
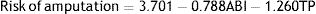
The variables included in the regression model were able to explain 83.3% of the variation in the risk of amputation. However, the variable TBI was excluded from the model due to perfect multicollinearity, which means it had a high correlation with other variables in the model. Additionally, the HbA1c variable was not found to be statistically significant (p>0.05), indicating that it did not have a significant independent effect on the risk of amputation. Regarding blood pressure indices, only two variables, ABI and TP, were found to be statistically significant in predicting the risk of amputation according to the WIfI scale. Details are represented in Table 6.
Table of correlation coefficients between the risk of amputation according to WIfI and independent variables.
| Independent variables | Risk of amputation | |
|---|---|---|
| Pearson correlation coefficient | p | |
| Number of years with diabetes diagnosis | −0.002 | 0.992 |
| Number of years with hypertension diagnosis | −0.272 | 0.232 |
| Number of years with dyslipidemia diagnosis | 0.110 | 0.709 |
| Smoking amount | 0.367 | 0.418 |
| HbA1C | 0.487 | 0.006* |
| LOPS with Monofilament 10g | 0.164 | 0.424 |
| ABI | −0.605 | <0.001* |
| TBI | −0.699 | <0.001* |
| TP | −0.699 | <0.001* |
In our study, we observed a similar proportion of male participants (56.7%) compared to females (43.3%) (Table 1). This finding is in line with previous studies conducted by Hicks et al. (2017) and Darling et al. (2015), which reported male rates of 60.3% and 59%, respectively.11,12 However, there are some differences in the mean age of our study subjects compared to previous research. The average age in our study was 67.23, which is higher than the mean age reported by Hicks et al. (2017) of 59 and Robinson et al. (2016) of 65.7,11 This variation in age could be attributed to the concentration of chronic disease patients among the elderly population in Vietnam. The high mean age of participants reflects the distribution of chronic disease burden among the elderly population in Vietnam. Additionally, there may be a tendency for patients to seek hospitalization when their conditions become severe and prolonged.
Regarding the medical history of the participants, apart from diabetes, a significant proportion of patients had comorbidities such as hypertension (71%) and dyslipidemia (46.7%). These findings are consistent with studies conducted by Zhan (2015), Robinson (2016), and Hicks (2017), which also reported high prevalence rates of hypertension, ranging from 82.9% to 86%; and dyslipidemia, ranging from 57% to 74%.7,12,13 Furthermore, we found that 23.3% of the study subjects were smokers, which is lower than the rates reported by Robinson et al. (2016) of 68%, Darling (2015) of 61%, and Hicks (2017) of 54.5%.7,11,12 These demographic characteristics provide important insights into the diabetic foot population in our study. The significant prevalence of comorbidities, such as hypertension and dyslipidemia, highlights the need for comprehensive management of these conditions in diabetic foot patients. Understanding the demographic characteristics of diabetic foot patients is crucial for tailoring interventions and developing targeted strategies for prevention, early detection, and management.
In our study, we found that the majority of patients exhibited ulcers (W) of varying degrees. However, in terms of disease severity, component I (ischemia) demonstrated a higher prevalence at grade 2 and grade 3. This finding emphasizes the importance of screening for foot ischemia using tools such as toe pressure (TP), ankle-brachial index (ABI), and toe-brachial index (TBI), as ischemia may manifest before the onset of ulcers. Notably, we found that 43.3% of hospitalized patients were at moderate and high stages (3 and 4) of amputation risk according to WIfI. This figure is consistent with the study conducted by Weaver et al., which reported a rate of 70.67%, but differs from other studies by Hicks et al. (47.6%), Robinson et al. (53%), and Zhan (55.7%).7,12,13 These results highlight the elevated risk of amputation among diabetic patients with foot disease, underscoring the need for continued monitoring and prospective management in the near future.
Furthermore, this study demonstrated a significant relationship between HbA1c levels and the risk levels according to the amputation stage in patients with diabetic foot (p=0.035). This finding is consistent with previous studies conducted by the teams of Weaver and Robinson, highlighting the importance of glycemic control in managing diabetic foot disease.7,8 Higher HbA1c levels indicate poorer glycemic control, leading to worsening of diabetic foot disease through mechanisms such as hypoperfusion, loss of protective sensation, and wound necrosis. Furthermore, the 10g Monofilament Foot Sensory Examination method proved to be a valuable tool in detecting loss of protective sensation (LOPS) across different stages of diabetic foot (p=0.012). This finding is supported by the study conducted by Hicks, where LOPS was also statistically significant (p<0.01).12 LOPS should be given special attention during diabetic foot screening, as it may not be visibly apparent but can be indicative of underlying ischemia and increased risk of complications. It is important to note that LOPS may not be consistently observed in many studies, leading to its exclusion from certain classifications.
Additionally, ABI, TBI, and TP were all found to be statistically significant in predicting the risk stages of limb amputation, according to the WIfI classification (with p values of 0.05, 0.01, and 0.01, respectively). Based on the regression analysis, the equation for estimating the risk of amputation according to the WIfI scale is as follows:
This equation allows for the calculation of an individual's risk of amputation based on their values for ABI and TP. The coefficients for ABI and TP indicate the strength and direction of their influence on the risk of amputation. In accordance with the findings of the three teams of Robinson, Weaver, and Hicks, the risk of amputation will increase when ischemia indicators in the diabetic foot decrease.7,8,12 Currently, there are no contradictory studies regarding ischemia. Moreover, the equation paved the wave to design and implement an online risk estimator for patients with diabetic foot, which is readily accessible at no cost. The development of online assessment tools, such as scoring systems or risk calculators, has promising implications for diabetic foot patient care. These instruments provide a simple and accessible method for assessing individual risk profiles and can facilitate early risk identification and timely interventions. By utilizing the findings of this study, we establish a preliminary risk calculator tailored to the requirements of diabetic foot patients in Vietnam (https://banchandaithaoduong.vn).
The incorporation of these online assessment tools into clinical practice has the potential to revolutionize diabetic foot management. Healthcare professionals would be able to assess amputation risk and tailor treatment programs accordingly. These instruments can aid in patient triage, ensuring that those with a greater risk receive priority for further evaluation and intervention. In addition, they can empower patients by improving their comprehension of their own risk profile, allowing them to actively engage in self-care and preventive measures.
LimitationsThe relatively small sample size of 60 patients, which may limit the generalizability of the findings, is one of the limitations of this study. In addition, the study was conducted at a solitary center, which may have introduced bias and limited its ability to represent the diabetic foot patient population in Vietnam as a whole. Additionally, the study's cross-sectional design hinders the ability to establish causal relationships between risk factors and amputation risk. To validate the findings and provide more robust evidence, longitudinal studies with larger sample sizes and multicenter collaborations are required. The use of convenience sampling may introduce selection bias, as the patients included in the study may not completely represent the diabetic foot patient population as a whole.
ConclusionThis study provides, for the first time, valuable insights into the characteristics of diabetic foot patients and their risk of amputation using the WIfI classification system among a Southeast Asian population. Elevated HbA1c levels were found to be associated with increased risk levels, while lower values of ABI, TBI, and TP were significantly correlated with higher risk stages, indicating the significance of impaired blood flow and perfusion in the development of amputation risk. The study also revealed a higher proportion of males among the study subjects, and identified comorbidities such as hypertension and dyslipidemia as common in diabetic foot patients. These findings have significant implications for future research and clinical practice. The development of a risk calculator tailored to diabetic foot patients based on the WIfI classification system holds promise for facilitating early risk assessment and personalized management strategies. The implementation of such online assessment tools could improve the identification of patients at higher risk of amputation, enabling timely interventions and improved patient outcomes. Nonetheless, it is important to acknowledge the limitations of this study, and future research should aim to validate these findings in larger, more diverse populations, and across multiple centers to strengthen the evidence base.
FundingThis research is supported by Vingroup Innovation Foundation (VINIF) in code VINIF.2022.TS011. The authors declare that this study received funding from the Vingroup Innovation Foundation (VINIF). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of interestsThe authors have no conflict of interests to declare.