Diabetes mellitus (DM) is a common cause of morbidity and mortality throughout the world. According to data from 2012, 13.8% of the Spanish population suffers from T2DM, although only 7.8% have been diagnosed.1 By comparison, the prevalence of T1DM is estimated at 0.08–0.2%, which represents 1–1.5% of all patients with diabetes.2
Patients with DM have a two to six times higher risk of hospitalisation in relation to their underlying disease compared to patients without diabetes.3,4 This means that one out of every six patients admitted to Spanish hospitals has been diagnosed with diabetes.5
Understanding the main causes and risk factors for hospitalisation is important as some may be modifiable, which could benefit patients by reducing the risk of admission, and have a beneficial impact on society with a reduction in associated costs.
The recent availability of big data analytics tools of clinical information has facilitated the identification of these possible risk factors.6 The “Electronic Health Records” (EHR) systems consist of the systematised collection of patient health information stored electronically in a digital format.7 This generated information is incorporated into tools such as Savana Manager® using “EHRead” technology, which enables the natural language of the EHRs to be extracted, thus guaranteeing confidentiality and enabling its analysis with artificial intelligence.8 We are therefore plunging into the era of “Big Data”, which allows the routine gathering of large amounts of data to be used, overcoming the limitations of traditional research at a much lower cost.9
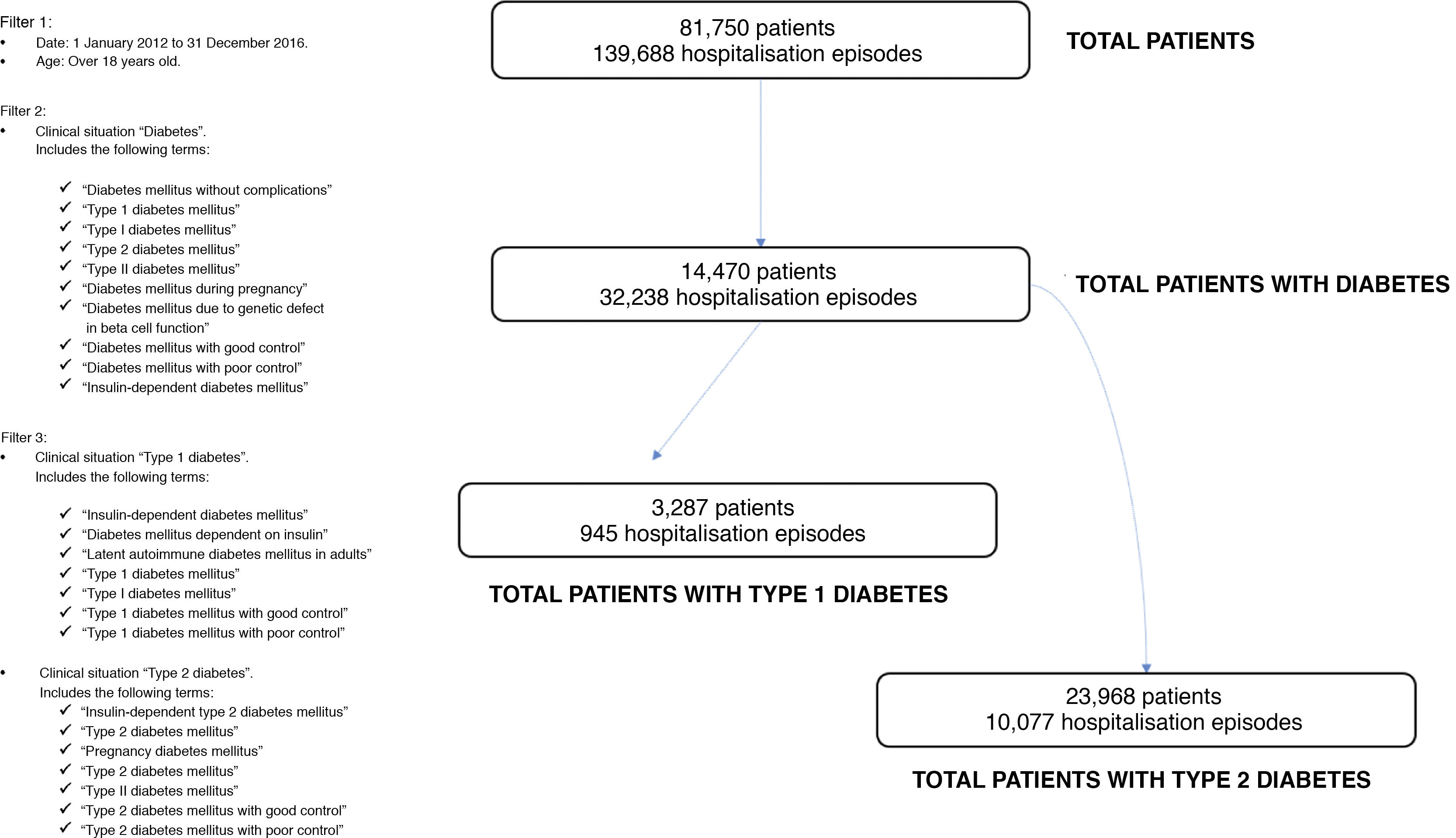
In order to assess the prevalence of hospitalised patients with diabetes and to identify the most common reasons for admission to our hospital in this population, after approval by our centre's Ethics Committee we used the Savana Manager©tool to select patients with a hospitalisation report in which “diabetes”, “type 2 diabetes mellitus” or “type 1 diabetes mellitus” were encoded either as the principal or secondary diagnosis or in personal history, in a hospital discharge report for a five-year period, from 1 January 2012 to 31 December 2016. Patients under 18 years of age at the time of hospitalisation were excluded. The patient inclusion flow chart is summarised in Fig. 1.
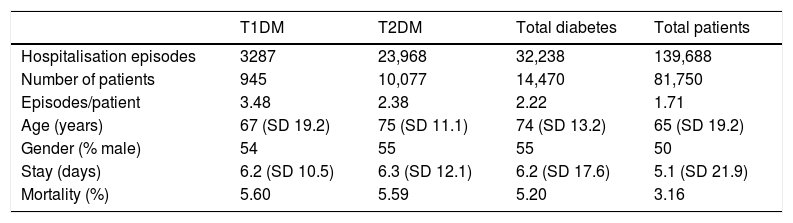
In the analysis period, 139,688 hospitalisation episodes were recorded in adult patients with an associated discharge report. The distribution of the principal characteristics by diabetes subtype is summarised in Table 1. It should be noted that 4983 patients diagnosed with diabetes were not subcategorised to T1DM or T2DM.
Clinical data of hospitalised patients based on history of diabetes.
| T1DM | T2DM | Total diabetes | Total patients | |
|---|---|---|---|---|
| Hospitalisation episodes | 3287 | 23,968 | 32,238 | 139,688 |
| Number of patients | 945 | 10,077 | 14,470 | 81,750 |
| Episodes/patient | 3.48 | 2.38 | 2.22 | 1.71 |
| Age (years) | 67 (SD 19.2) | 75 (SD 11.1) | 74 (SD 13.2) | 65 (SD 19.2) |
| Gender (% male) | 54 | 55 | 55 | 50 |
| Stay (days) | 6.2 (SD 10.5) | 6.3 (SD 12.1) | 6.2 (SD 17.6) | 5.1 (SD 21.9) |
| Mortality (%) | 5.60 | 5.59 | 5.20 | 3.16 |
The diagnosis most often associated with diabetes was congestive heart failure, identified in 17.9% of patients with T2DM and 20.1% of patients with T1DM, compared to 6.4% of all hospitalised patients in the period analysed. This was followed by admission motivated by glycaemic control disorders: 8.4% of patients with T2DM (6.1% decompensated diabetes; 2.3% hypoglycaemia) and 18.7% of patients with T1DM (11.3% decompensated diabetes; 5.9% hypoglycaemia; 1.5% diabetic ketoacidosis).
Diabetes and heart failure are two entities that often occur concomitantly, accounting for 20.1% of hospitalisations in patients with T2DM according to ministerial data.5 The results of our analysis underscore the importance of this association, suggesting that it is also likely to extend to patients with T1DM.
However, important limitations intrinsically associated with errors in the preparation of the EHRs from which the information is obtained must be taken into account. For example, in our results, we see that 4983 patients diagnosed with diabetes (15.45% of the total number of people with diabetes) are not subcategorised to type 1 or type 2 diabetes. Moreover, the prevalence of patients categorised as T1DM is excessive - it is 10 times higher in the data obtained in the hospitalised population than in the general population. This is probably due to confusion in the encoding in many cases by the healthcare professionals who write the hospitalisation discharge reports for insulin-dependent patients with T2DM or T1DM, since the Savana Manager® tool classifies the diagnosis “insulin-dependent diabetes mellitus” as “type 1 diabetes”, which makes it impossible for us to reach definitive conclusions with the data obtained in this subpopulation. Finally, it should be noted that this tool does not currently allow for statistical analysis of the data obtained, so it cannot yet fully replace traditional research.
As a final conclusion, big data still requires some adjustments, in which doctors must play a role. Despite this, big data analytics is becoming increasingly present in our lives and we are already obtaining the first results of its application. This new technology will very soon provide differential value, opening a new door to knowledge, which will mean a revolution never seen before in the world of health.
Authorship/collaboratorsD.E. Barajas Galindo was responsible for the conception and design of the study. D.E. Barajas Galindo, B. Pintor de la Maza, I. Cano Rodríguez and M.D. Ballesteros Pomar participated in the conduct of the study, writing of the manuscript and reviewing the final version.
The authors express their gratitude to the Savana Medica® team for their collaboration, which was necessary to the methodological review of this study.
Please cite this article as: Barajas-Galindo DE, Pintor-de la Maza B, Cano-Rodríguez I, Ballesteros-Pomar MD. Valoración de hospitalizaciones en pacientes con diabetes con herramientas de sistemas de información clínica. Endocrinol Diabetes Nutr. 2021;68:444–446.