From the third decade of life and due to multiple causes, muscle mass and strength are gradually lost, which affects the function of the musculoskeletal system.
This combined loss of muscle mass and strength with aging is called sarcopenia, and is associated with greater morbidity and mortality in the elderly. Early treatment is therefore essential, and physical exercise is the therapeutic approach that has given the best results.
This literature review intended to analyze the effect of physical exercise, excluding the role that other treatments proposed, including the nutritional approach, could play in the treatment of sarcopenia, refers to 12 articles.
In studies including high intensity strength exercises in isolation, either alone or combined with aerobic exercise, improvements were seen in muscle mass, muscle strength, and functional test times. There is also a significant increase in fat-free mass in individuals who exercised more frequently (more than two sessions per week).
Current evidence shows that strength-resistance training and its combination in multimodal programs with aerobic exercise show significantly beneficial effects on anthropometric and muscle function parameters. Programs of prescribed exercises including strength exercises adequate to the characteristics should therefore be adapted to the characteristics of each individual and replace the usual practice of prescribing aerobic exercises (walking) only.
A partir de la tercera década de la vida, y por causas multifactoriales, se pierde masa y fuerza muscular de forma progresiva, afectando a la funcionalidad del aparato locomotor.
A esta pérdida combinada de masa y fuerza muscular que aparece con el envejecimiento se le denomina sarcopenia, la cual se asocia a una mayor morbimortalidad en el sujeto anciano, por lo que el tratamiento precoz es fundamental, siendo el ejercicio físico la estrategia terapéutica que mejores resultados ha demostrado.
En esta revisión bibliográfica realizada para analizar el efecto individual del ejercicio físico, excluyendo el papel que podría representar en el tratamiento de la sarcopenia otras propuestas desde el enfoque nutricional, se incluyen 12 artículos.
En aquellos estudios que incluían ejercicios de fuerza de alta intensidad de forma aislada, exclusivamente o combinado con ejercicio aeróbico, se observa mejoría de la masa muscular, fuerza muscular y tiempos en pruebas funcionales. Existe asimismo un incremento significativo de masa libre de grasa en individuos que realizaban ejercicio con mayor frecuencia (más de 2 sesiones a la semana).
La evidencia actual demuestra que los entrenamientos basados en fuerza-resistencia y la combinación en programas multimodales con ejercicio aeróbico muestran efectos significativamente beneficiosos sobre parámetros antropométricos y de funcionalidad muscular, debiendo por tanto adecuarse los programas de ejercicios pautados, incluyendo ejercicios de fuerza adaptados a las características de cada individuo, y sustituir a la práctica habitual de prescribir en exclusiva ejercicios de tipo aeróbico (caminar).
The key feature of human aging is the loss of functional reserve.1,2 Since the third decade of life, the musculoskeletal system begins to experience a slow but progressive loss of muscle mass and strength. From 50 years of age, muscle mass decreases by 1%–2% a year, and muscle strength decreases by 1.5%–3% annually from 65 years of age.2 These physical and functional changes vary between sexes, with progression being slower in men and sharper in women, which is probably related to the coexistence of menopause.2,3
The term sarcopenia has recently been used to refer to this combined loss of muscle mass and strength associated with aging,4 with the added characteristic that such loss should be involuntary.2 A close relationship has been shown between a decreased muscle mass and an increased risk of institutionalization and mortality, regardless of other associated risk factors,5 and also with dependence, which increases 2–5-fold in subjects with sarcopenia as compared to subjects of the same age without this diagnosis.6
One of the main problems for incorporation of the term sarcopenia into daily clinical practice is the lack of a unified criterion for defining sarcopenia,7 because although there is agreement that muscle mass loss should be sufficient to cause symptoms8 and that the definition of sarcopenia should include three criteria: loss of muscle mass, loss of strength, and qualitative changes in muscle tissue,1 there is no accepted standard method for measuring muscle mass, and the level of loss of muscle mass and/or function from which an elderly person may be considered “pathologically sarcopenic” is also not clearly established.
Diagnosis of sarcopenia is therefore complex, and has been quite often based on the consensus criteria established by the European Working Group on Sarcopenia in Older People9 in 2018, in which sarcopenia is diagnosed in three steps: an initial screening test (SARC-F), followed by a strength test to establish the probability of sarcopenia, and finally a confirmatory test with of muscle mass assessment. There is also a complementary fourth step to assess severity of sarcopenia with function tests. The consensus criteria proposed in 2009 by the International Working Group in Sarcopenia consisting of a walking speed below 1 m/s and an objective decrease in muscle mass have also been used.10
Despite these difficulties to define the condition, it is clear that aging of the population has increased the importance and interest of this clinical situation, leading to an increase in therapeutic efforts aimed at preventing and/or reversing sarcopenia. This treatment approach focuses on three mainstays:
- 1.
Nutritional intervention based on covering the calorie and protein requirements of each individual, with supplemental supplies if required.11
- 2.
Pharmacological intervention such as use of vitamin D, testosterone or growth hormone, that has been ineffective or even counterproductive in various studies due to adverse effects in the elderly population.
- 3.
Physical exercise, which has been shown to be a very useful tool for fighting and preventing sarcopenia and is not contraindicated in elderly people when duly adapted.12 When considering a training program for the treatment of sarcopenia, it should be taken into account that there are different types of exercise, and a unique or mixed program may be planned combining the different types of exercise.
Aerobic exercise is continuous activity of several muscle groups that increases heart rate above its resting level for a sustained period of time, and should be adjusted based on maximum heart rate (HRmax). In an exercise program for elderly patients, an intensity of activity at 60%–75% of HRmax for 30 min three days a week is recommended.13
Strength exercise is an activity in which muscle builds strength against resistance. Depending on its intensity, there are other three subtypes14: low intensity, <40% of a maximum repetition (maximum weight with which a single repetition can be performed [1MR]); moderate intensity, = 40%–60% of 1RM; and high intensity, >60% of 1MR.
Neuromuscular exercise is the activity that works with balance and proprioception with the aim of improving posture and preventing falls. Exercises may be static or dynamic.
ObjectivesThe primary objective of this systematic review is to assess the effect of different types of physical exercise on sarcopenia. For this, the concept of sarcopenia is defined, the implications of this condition for health are detailed, and the type, frequency, and dosage of exercise are assessed to determine changes in muscle mass and strength.
MethodsA systematic review. An initial search was made in the Pubmed database using the keywords exercise, sarcopenia and elderly. The advanced search was adjusted to studies published in the last 10 years (2008–2018), clinical trials, and studies conducted in humans.
The search strategy was as follows: (exercise [MeSH Terms] OR exercise [All Fields]) AND (sarcopenia [MeSH Terms] OR sarcopenia [All Fields]) AND (aged [MeSH Terms] OR aged [All Fields] OR elderly [All Fields]) AND (Clinical Trial [ptyp] AND 2008/01/01 [PDat]: 2018/12/31 [PDat] AND humans [MeSH Terms]).
The following databases were subsequently reviewed: Scopus, Scielo, and Web Science.
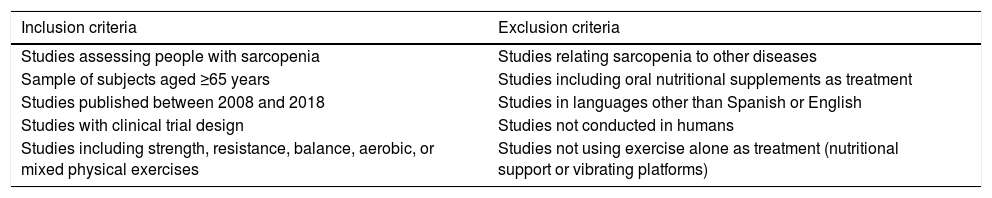
After an initial review of the abstracts, the full text of the articles that met the inclusion criteria were examined. The articles selected because they complied with the inclusion and exclusion criteria (Table 1) were evaluated using the PEDro scale15 to determine their methodological quality.
Inclusion and exclusion criteria of the articles reviewed.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Studies assessing people with sarcopenia | Studies relating sarcopenia to other diseases |
| Sample of subjects aged ≥65 years | Studies including oral nutritional supplements as treatment |
| Studies published between 2008 and 2018 | Studies in languages other than Spanish or English |
| Studies with clinical trial design | Studies not conducted in humans |
| Studies including strength, resistance, balance, aerobic, or mixed physical exercises | Studies not using exercise alone as treatment (nutritional support or vibrating platforms) |
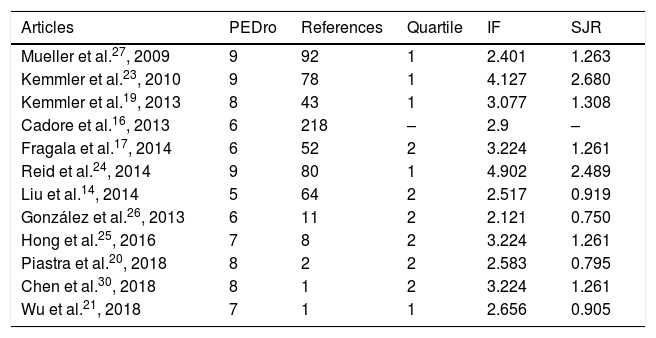
Methodological quality was also determined using other methods such as the number of citations received, the impact factor, the quartile, or the SCImago Journal Rank (Table 2).
Methodological quality of articles included in the systematic review.
| Articles | PEDro | References | Quartile | IF | SJR |
|---|---|---|---|---|---|
| Mueller et al.27, 2009 | 9 | 92 | 1 | 2.401 | 1.263 |
| Kemmler et al.23, 2010 | 9 | 78 | 1 | 4.127 | 2.680 |
| Kemmler et al.19, 2013 | 8 | 43 | 1 | 3.077 | 1.308 |
| Cadore et al.16, 2013 | 6 | 218 | – | 2.9 | – |
| Fragala et al.17, 2014 | 6 | 52 | 2 | 3.224 | 1.261 |
| Reid et al.24, 2014 | 9 | 80 | 1 | 4.902 | 2.489 |
| Liu et al.14, 2014 | 5 | 64 | 2 | 2.517 | 0.919 |
| González et al.26, 2013 | 6 | 11 | 2 | 2.121 | 0.750 |
| Hong et al.25, 2016 | 7 | 8 | 2 | 3.224 | 1.261 |
| Piastra et al.20, 2018 | 8 | 2 | 2 | 2.583 | 0.795 |
| Chen et al.30, 2018 | 8 | 1 | 2 | 3.224 | 1.261 |
| Wu et al.21, 2018 | 7 | 1 | 1 | 2.656 | 0.905 |
IF: impact factor; SJR: SCImago Journal Rank.
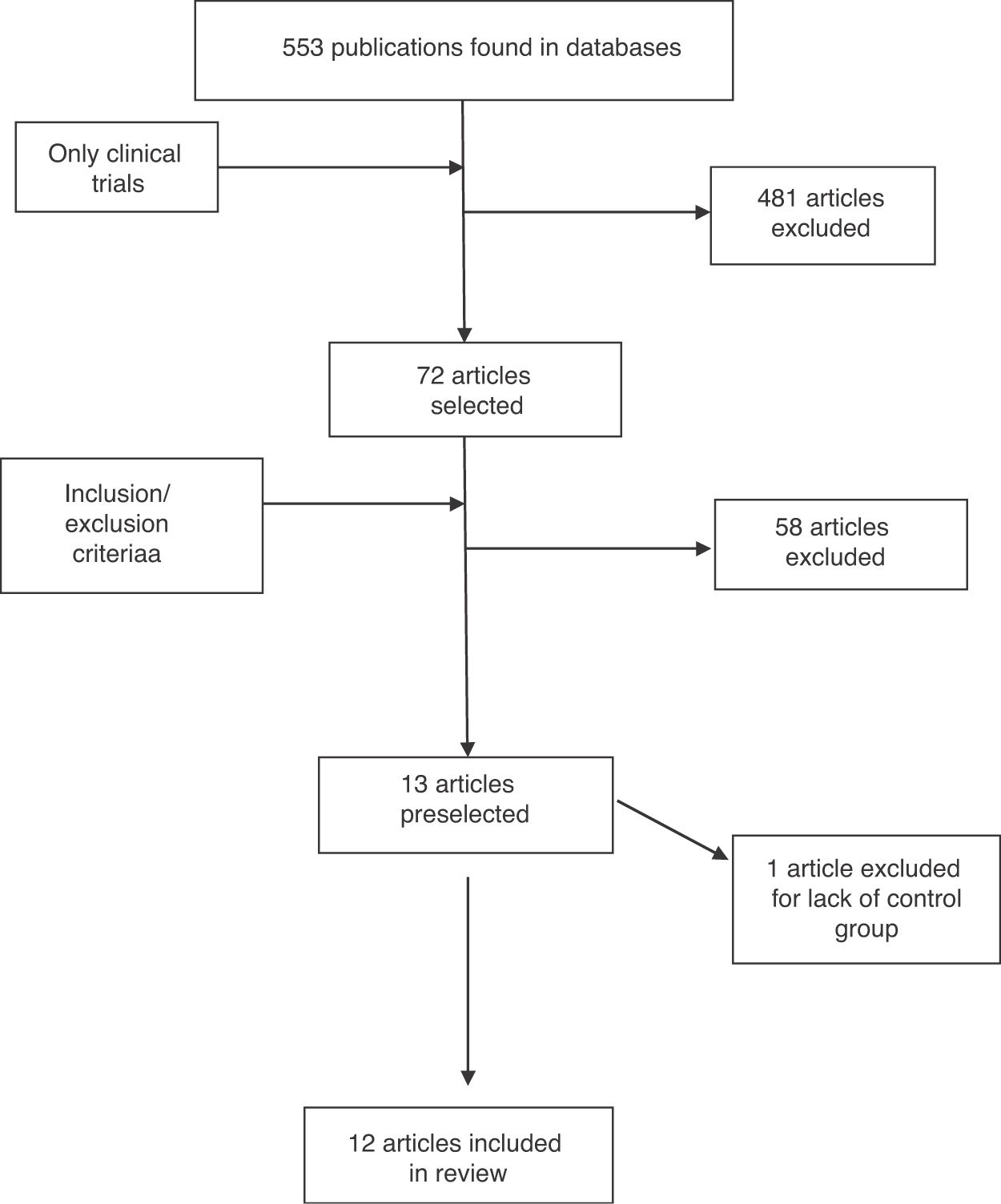
The flow chart shows the procedure for selecting the 12 articles making up the final sample of this systematic review (Fig. 1).
The parameters most commonly studied by the publications included in our study are muscle mass (MM), muscle strength (MS), and physical tests.
Given the variability of parameters included in the articles, only the most important variables are included methodologically in this description:
Morphological variables were assessed based on:
- •
Body fat: assessed by measurement of skin folds and/or bioimpedance.
- •
Fat-free mass or lean body mass (LBM): includes intra- and extracellular water, the bone mineral system, and muscle and visceral proteins. This was assessed by densitometry (DXA) or electrical bioimpedance (BIA).
- •
MM: assessed by computed tomography, DXA, or BIA.
- •
Appendicular MM: the sum of the lean mass of the legs and arms. It was assessed by DXA or BIA
- •
MS: assessed using a dynamometer.
Functional test variables were assessed using:
- •
Timed up and go: this assesses if the subject is able to rise from a chair with armrests, walk three meters, turn, walk back those three meters, and down sit again.16–18
- •
Short Physical Performance Battery: this consists of three physical tests, a balance test, a short walk (4 m) at the usual pace, and rising from a chair five consecutive times. Score ranges from 0 (lowest) and 12 (best).16,19
- •
Chair rise test: this consists of measuring over 30 s how many times can a subject sit down on and rise from a chair.16,17
- •
Walking speed: time taken to walk five meters at a normal pace.16,20
Twelve articles were selected in this systematic review, and were analyzed and compared. All of them were prospective, randomized clinical trials except for the Wu et al. study,21 which was not randomized, and the retrospective analysis of data collected in the SEFIP study,22 published by Kemmler et al.23
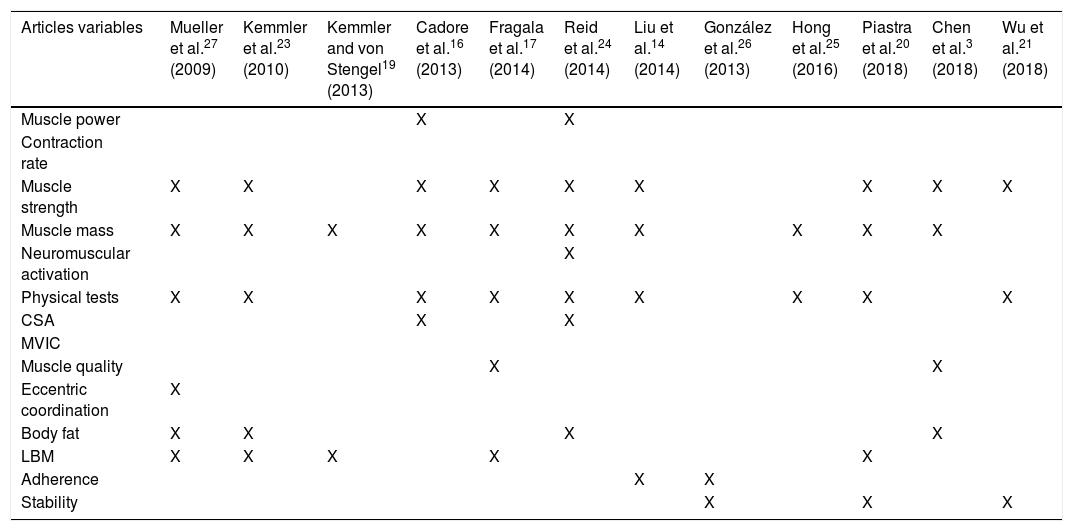
Because of the great variability of outcome variables analyzed in the different studies, only the most common and relevant variables, grouped in the categories of muscle power, contraction speed, muscle strength, muscle mass, neuromuscular activation, physical tests, cross-sectional area of muscle (CSA), metric contraction tests (MVIC), muscle quality index, extrinsic coordination, body fat, MBL, adherence, and stability were selected. Table 3 shows assessment of these variables in each of the studies evaluated in this review.
Main variables recorded in the articles analyzed in the review.
| Articles variables | Mueller et al.27 (2009) | Kemmler et al.23 (2010) | Kemmler and von Stengel19 (2013) | Cadore et al.16 (2013) | Fragala et al.17 (2014) | Reid et al.24 (2014) | Liu et al.14 (2014) | González et al.26 (2013) | Hong et al.25 (2016) | Piastra et al.20 (2018) | Chen et al.3 (2018) | Wu et al.21 (2018) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Muscle power | X | X | ||||||||||
| Contraction rate | ||||||||||||
| Muscle strength | X | X | X | X | X | X | X | X | X | |||
| Muscle mass | X | X | X | X | X | X | X | X | X | X | ||
| Neuromuscular activation | X | |||||||||||
| Physical tests | X | X | X | X | X | X | X | X | X | |||
| CSA | X | X | ||||||||||
| MVIC | ||||||||||||
| Muscle quality | X | X | ||||||||||
| Eccentric coordination | X | |||||||||||
| Body fat | X | X | X | X | ||||||||
| LBM | X | X | X | X | X | |||||||
| Adherence | X | X | ||||||||||
| Stability | X | X | X |
CSA: cross-sectional area of muscle; LBM: lean body mass; MVIC: contraction tests.
The training programs of the different studies were mainly based on two types of exercise: strength-only exercises17,19,24 and multimodal exercises,25,26 the latter including combinations of neuromuscular,16 resistance, and aerobic exercises, among which walking was the usual exercise of choice.17
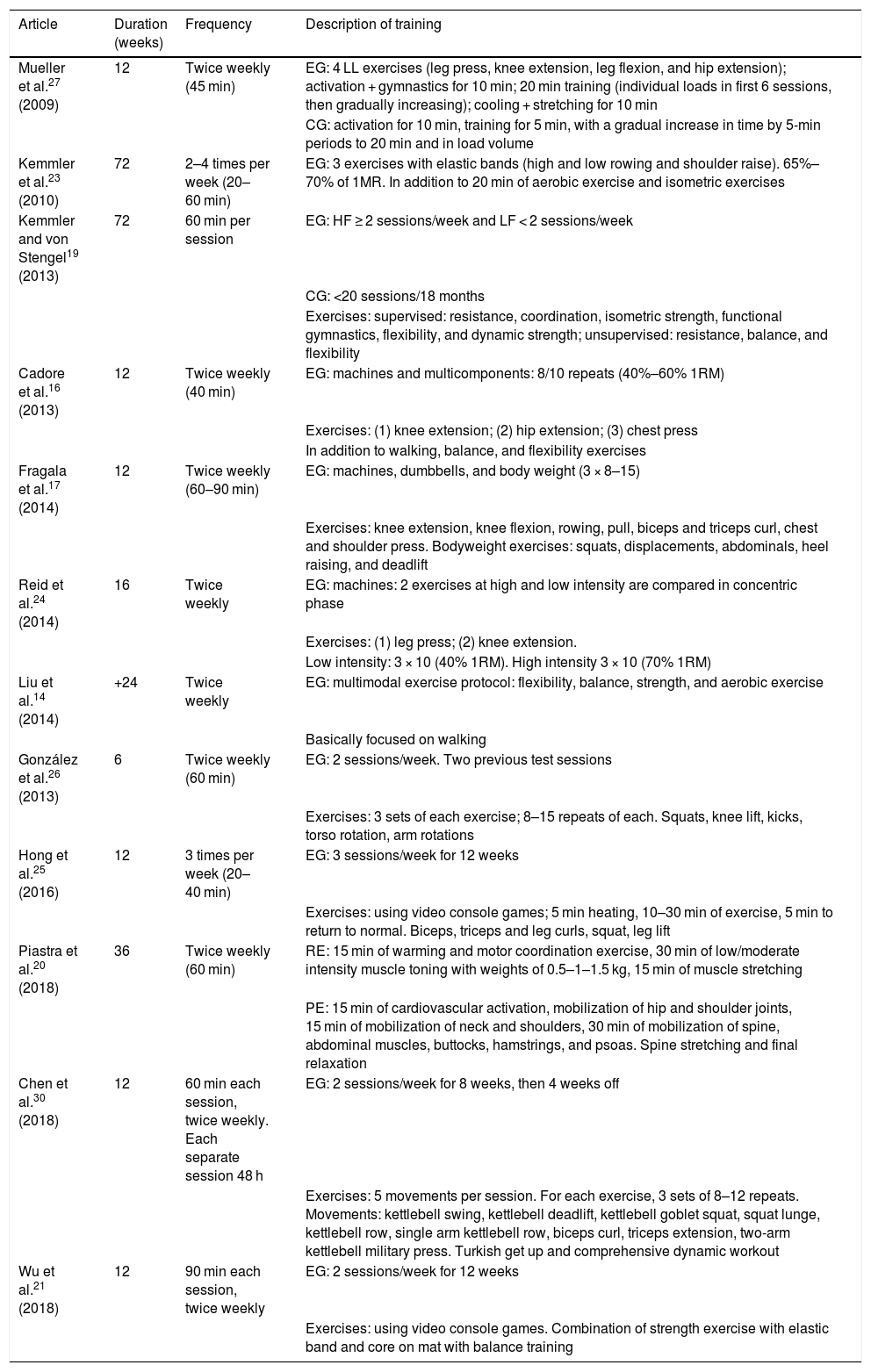
Table 4 gives a detailed description of the training protocols of each study, including their duration and number of weekly sessions. The training performed by the control group in studies intended to compare the efficacy of different training systems is also detailed where appropriate. In studies where training of the control group is not detailed, this group does not perform exercise.
Exercise protocol in studies included in the systematic review.
| Article | Duration (weeks) | Frequency | Description of training |
|---|---|---|---|
| Mueller et al.27 (2009) | 12 | Twice weekly (45 min) | EG: 4 LL exercises (leg press, knee extension, leg flexion, and hip extension); activation + gymnastics for 10 min; 20 min training (individual loads in first 6 sessions, then gradually increasing); cooling + stretching for 10 min |
| CG: activation for 10 min, training for 5 min, with a gradual increase in time by 5-min periods to 20 min and in load volume | |||
| Kemmler et al.23 (2010) | 72 | 2–4 times per week (20–60 min) | EG: 3 exercises with elastic bands (high and low rowing and shoulder raise). 65%–70% of 1MR. In addition to 20 min of aerobic exercise and isometric exercises |
| Kemmler and von Stengel19 (2013) | 72 | 60 min per session | EG: HF ≥ 2 sessions/week and LF < 2 sessions/week |
| CG: <20 sessions/18 months | |||
| Exercises: supervised: resistance, coordination, isometric strength, functional gymnastics, flexibility, and dynamic strength; unsupervised: resistance, balance, and flexibility | |||
| Cadore et al.16 (2013) | 12 | Twice weekly (40 min) | EG: machines and multicomponents: 8/10 repeats (40%–60% 1RM) |
| Exercises: (1) knee extension; (2) hip extension; (3) chest press | |||
| In addition to walking, balance, and flexibility exercises | |||
| Fragala et al.17 (2014) | 12 | Twice weekly (60–90 min) | EG: machines, dumbbells, and body weight (3 × 8–15) |
| Exercises: knee extension, knee flexion, rowing, pull, biceps and triceps curl, chest and shoulder press. Bodyweight exercises: squats, displacements, abdominals, heel raising, and deadlift | |||
| Reid et al.24 (2014) | 16 | Twice weekly | EG: machines: 2 exercises at high and low intensity are compared in concentric phase |
| Exercises: (1) leg press; (2) knee extension. | |||
| Low intensity: 3 × 10 (40% 1RM). High intensity 3 × 10 (70% 1RM) | |||
| Liu et al.14 (2014) | +24 | Twice weekly | EG: multimodal exercise protocol: flexibility, balance, strength, and aerobic exercise |
| Basically focused on walking | |||
| González et al.26 (2013) | 6 | Twice weekly (60 min) | EG: 2 sessions/week. Two previous test sessions |
| Exercises: 3 sets of each exercise; 8–15 repeats of each. Squats, knee lift, kicks, torso rotation, arm rotations | |||
| Hong et al.25 (2016) | 12 | 3 times per week (20–40 min) | EG: 3 sessions/week for 12 weeks |
| Exercises: using video console games; 5 min heating, 10–30 min of exercise, 5 min to return to normal. Biceps, triceps and leg curls, squat, leg lift | |||
| Piastra et al.20 (2018) | 36 | Twice weekly (60 min) | RE: 15 min of warming and motor coordination exercise, 30 min of low/moderate intensity muscle toning with weights of 0.5–1–1.5 kg, 15 min of muscle stretching |
| PE: 15 min of cardiovascular activation, mobilization of hip and shoulder joints, 15 min of mobilization of neck and shoulders, 30 min of mobilization of spine, abdominal muscles, buttocks, hamstrings, and psoas. Spine stretching and final relaxation | |||
| Chen et al.30 (2018) | 12 | 60 min each session, twice weekly. Each separate session 48 h | EG: 2 sessions/week for 8 weeks, then 4 weeks off |
| Exercises: 5 movements per session. For each exercise, 3 sets of 8–12 repeats. Movements: kettlebell swing, kettlebell deadlift, kettlebell goblet squat, squat lunge, kettlebell row, single arm kettlebell row, biceps curl, triceps extension, two-arm kettlebell military press. Turkish get up and comprehensive dynamic workout | |||
| Wu et al.21 (2018) | 12 | 90 min each session, twice weekly | EG: 2 sessions/week for 12 weeks |
| Exercises: using video console games. Combination of strength exercise with elastic band and core on mat with balance training |
LL: lower limbs; PE: postural exercise; RE: resistance exercise; CG: control group; EG: experimental group.
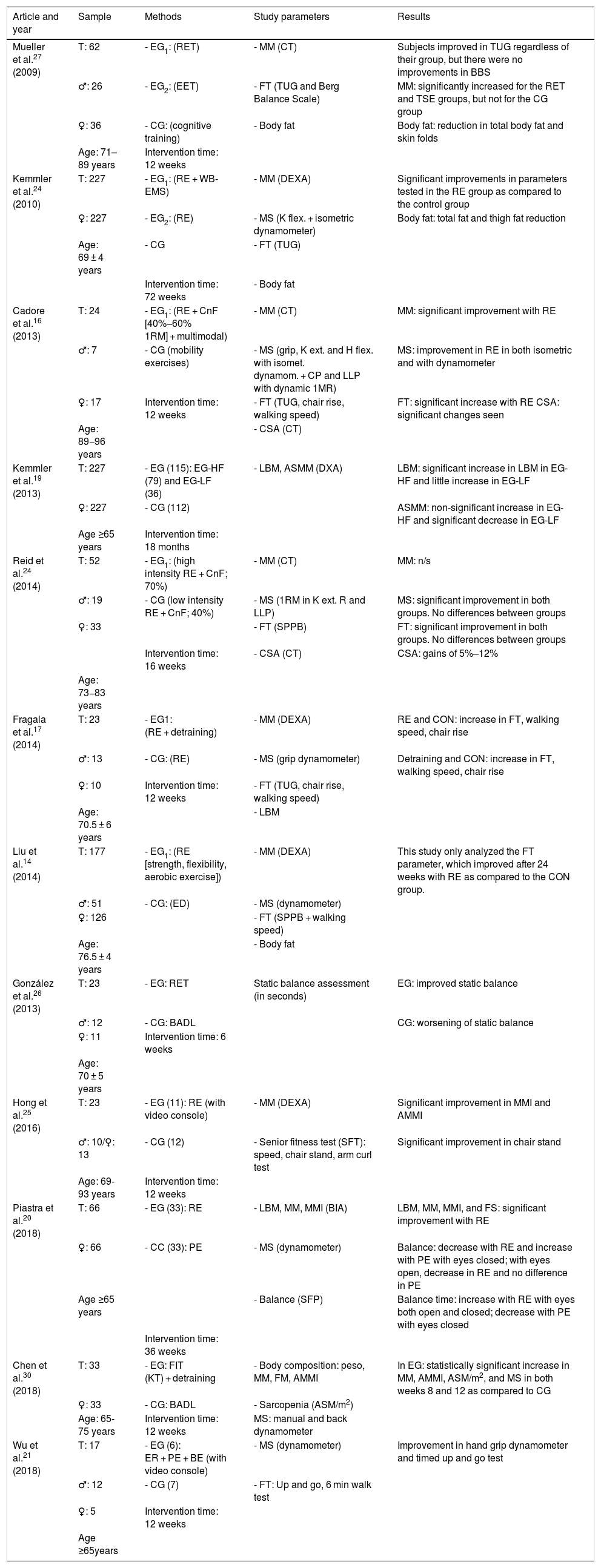
Table 5 lists each of the articles examined for this review and provides details on the sample size, age, and sex distribution of participants, and description and duration of the intervention. The last column summarizes the most significant results as regards the impact of exercise prescribed in sarcopenia, assessed as changes in MM and/or MS and/or functional tests.
Results in the main variables in articles included in the review.
| Article and year | Sample | Methods | Study parameters | Results |
|---|---|---|---|---|
| Mueller et al.27 (2009) | T: 62 | - EG1: (RET) | - MM (CT) | Subjects improved in TUG regardless of their group, but there were no improvements in BBS |
| ♂: 26 | - EG2: (EET) | - FT (TUG and Berg Balance Scale) | MM: significantly increased for the RET and TSE groups, but not for the CG group | |
| ♀: 36 | - CG: (cognitive training) | - Body fat | Body fat: reduction in total body fat and skin folds | |
| Age: 71–89 years | Intervention time: 12 weeks | |||
| Kemmler et al.24 (2010) | T: 227 | - EG1: (RE + WB-EMS) | - MM (DEXA) | Significant improvements in parameters tested in the RE group as compared to the control group |
| ♀: 227 | - EG2: (RE) | - MS (K flex. + isometric dynamometer) | Body fat: total fat and thigh fat reduction | |
| Age: 69 ± 4 years | - CG | - FT (TUG) | ||
| Intervention time: 72 weeks | - Body fat | |||
| Cadore et al.16 (2013) | T: 24 | - EG1: (RE + CnF [40%−60% 1RM] + multimodal) | - MM (CT) | MM: significant improvement with RE |
| ♂: 7 | - CG (mobility exercises) | - MS (grip, K ext. and H flex. with isomet. dynamom. + CP and LLP with dynamic 1MR) | MS: improvement in RE in both isometric and with dynamometer | |
| ♀: 17 | Intervention time: 12 weeks | - FT (TUG, chair rise, walking speed) | FT: significant increase with RE CSA: significant changes seen | |
| Age: 89−96 years | - CSA (CT) | |||
| Kemmler et al.19 (2013) | T: 227 | - EG (115): EG-HF (79) and EG-LF (36) | - LBM, ASMM (DXA) | LBM: significant increase in LBM in EG-HF and little increase in EG-LF |
| ♀: 227 | - CG (112) | ASMM: non-significant increase in EG-HF and significant decrease in EG-LF | ||
| Age ≥65 years | Intervention time: 18 months | |||
| Reid et al.24 (2014) | T: 52 | - EG1: (high intensity RE + CnF; 70%) | - MM (CT) | MM: n/s |
| ♂: 19 | - CG (low intensity RE + CnF; 40%) | - MS (1RM in K ext. R and LLP) | MS: significant improvement in both groups. No differences between groups | |
| ♀: 33 | - FT (SPPB) | FT: significant improvement in both groups. No differences between groups | ||
| Intervention time: 16 weeks | - CSA (CT) | CSA: gains of 5%–12% | ||
| Age: 73−83 years | ||||
| Fragala et al.17 (2014) | T: 23 | - EG1: (RE + detraining) | - MM (DEXA) | RE and CON: increase in FT, walking speed, chair rise |
| ♂: 13 | - CG: (RE) | - MS (grip dynamometer) | Detraining and CON: increase in FT, walking speed, chair rise | |
| ♀: 10 | Intervention time: 12 weeks | - FT (TUG, chair rise, walking speed) | ||
| Age: 70.5 ± 6 years | - LBM | |||
| Liu et al.14 (2014) | T: 177 | - EG1: (RE [strength, flexibility, aerobic exercise]) | - MM (DEXA) | This study only analyzed the FT parameter, which improved after 24 weeks with RE as compared to the CON group. |
| ♂: 51 | - CG: (ED) | - MS (dynamometer) | ||
| ♀: 126 | - FT (SPPB + walking speed) | |||
| Age: 76.5 ± 4 years | - Body fat | |||
| González et al.26 (2013) | T: 23 | - EG: RET | Static balance assessment (in seconds) | EG: improved static balance |
| ♂: 12 | - CG: BADL | CG: worsening of static balance | ||
| ♀: 11 | Intervention time: 6 weeks | |||
| Age: 70 ± 5 years | ||||
| Hong et al.25 (2016) | T: 23 | - EG (11): RE (with video console) | - MM (DEXA) | Significant improvement in MMI and AMMI |
| ♂: 10/♀: 13 | - CG (12) | - Senior fitness test (SFT): speed, chair stand, arm curl test | Significant improvement in chair stand | |
| Age: 69-93 years | Intervention time: 12 weeks | |||
| Piastra et al.20 (2018) | T: 66 | - EG (33): RE | - LBM, MM, MMI (BIA) | LBM, MM, MMI, and FS: significant improvement with RE |
| ♀: 66 | - CC (33): PE | - MS (dynamometer) | Balance: decrease with RE and increase with PE with eyes closed; with eyes open, decrease in RE and no difference in PE | |
| Age ≥65 years | - Balance (SFP) | Balance time: increase with RE with eyes both open and closed; decrease with PE with eyes closed | ||
| Intervention time: 36 weeks | ||||
| Chen et al.30 (2018) | T: 33 | - EG: FIT (KT) + detraining | - Body composition: peso, MM, FM, AMMI } | In EG: statistically significant increase in MM, AMMI, ASM/m2, and MS in both weeks 8 and 12 as compared to CG |
| ♀: 33 | - CG: BADL | - Sarcopenia (ASM/m2) | ||
| Age: 65-75 years | Intervention time: 12 weeks | MS: manual and back dynamometer} | ||
| Wu et al.21 (2018) | T: 17 | - EG (6): ER + PE + BE (with video console) | - MS (dynamometer) | Improvement in hand grip dynamometer and timed up and go test |
| ♂: 12 | - CG (7) | - FT: Up and go, 6 min walk test | ||
| ♀: 5 | Intervention time: 12 weeks | |||
| Age ≥65years |
BADL: basic activities of daily living; ASMM: appendicular skeletal muscle mass; BIA: bioelectrical impedance analysis; CSA: cross-sectional area of muscle; Cniso: isometric contraction; CnS: slow contraction; CnF: Fast contraction; DEXA: dual X-ray absorptiometry; BE: balance exercise; EET: eccentric exercise; ED: education group; PE: postural exercise; RE: resistance exercise; H ext.: hip extension; K ext.: knee extension; Ex. S: explosive strength; IS: isometric strength; MS: muscle strength; FIT: fitness; K flex.; knee flexion; CG: control group; EG-HF: experimental group-high frequency; EG: experimental group; EG-LF: experimental group-low frequency; MMI: muscle mass index; LBM: lean body mass; MM: muscle mass; MVIC: isometric contraction test; FT: functional test; SFP: static force platform; LLP: lower limb press; CP: chest press; RET: conventional resistance exercise; RM: maximum repetition; MRI: magnetic resonance imaging; SL: high intensity strength/high volume; SPPB: short physical performance battery; SS: high intensity strength/low volume; CT: computed tomography; TUG: timed up and go; WB-EMS: whole body electromyostimulation.
Muscle mass results from studies with groups of subjects who followed training programs in which aerobic exercise (walk) predominates showed no positive results in MM. The number of people with criteria for sarcopenia even increased at the end of the study, as occurred in the Mueller et al. study27 with subjects in the control group.
This review found that all studies where a significant change was seen in MM gain included strength exercises with dumbbells, machines or elastic bands, with modest results in studies based on low-intensity strength exercises24 where MM increased by approximately 1%, and markedly better results in those based on high intensity functional training, with an MM gain of 2%–5%16,17 in similar time periods. These differences are clearly exemplified by the Piastra et al. study20, which compared two groups with high- versus low-intensity strength training. Benefits were not only seen in anthropometric parameters (LBM, MM, MMI, MS), but also in static balance26 and functional parameters, with improved times in the timed up and go test17,23 and in walking speed.
The study with the best overall results was the one performed by Cadore et al.16, reporting a positive increase in all parameters analyzed (MM +3.3%, MS +144%, and physical tests +58%) using a multimodal exercise program consisting of two weekly 40 min sessions combining three series of high-intensity strength exercises (8–10 repetitions) with balance and aerobic exercises. Another unique feature of this study was that it included older patients (89–96 years), showing that a multifunctional exercise-based intervention can be effective and well tolerated by nonagenarians.
As regards training frequency, the results of the Kemmler et al. study19 showed a significant increase in LBM in subjects who exercised more frequently (more than two sessions per week) than in those with more limited frequency of exercise (less than two sessions per week). No increase related to the greater frequency of training was seen in appendicular muscle mass, but this significantly decreased in subjects with low training frequency.
DiscussionMM and MS are significantly related, with reduction in one of them leading to reduction in the other,18 triggering the occurrence of sarcopenia.17 Physical exercise is known to have positive effects on MM and especially on MS, and is therefore currently considered the main tool for managing sarcopenia to avoid increased comorbidity, falls in elderly patients, and the resultant dependence.28
The purpose of this study was to conduct a systematic review to separately study the effectiveness of exercise in sarcopenia, comparing different training protocols and types of exercise, observing improvements in body composition in older people with a muscle mass lower than desired.
In the MM results reported by studies based on aerobic (walking) exercise protocols only, no positive results were seen in MM,16 and the number of people with criteria for sarcopenia was even higher at the end of the study. By contrast, studies where a significant change was seen as MM gain and improved functionality and static balance always included strength exercises, either alone or combined with mixed strength and aerobic exercise programs, with the latter providing the best results.16
A separate comment should be made of the frequency and duration of the proposed training sessions, which will undoubtedly have an impact on the changes generated by the exercise, particularly in the elderly. In this regard, the conclusions of the Kemmler et al. study,19 which showed benefits when training frequency was higher than 2 weekly sessions, are interesting. The recommendation to establish 48 h of rest in training of the same muscle group should however be taken into account, as it has been shown in the general population that this is not only helpful for muscle rest, but also to achieve better results.29 The Chen et al. study30 was the only one including this recommendation in its exercise protocol.
At least two systematic reviews have been previously published on this subject,31,32 and their conclusions are in line with the above considerations; the most marked benefit is achieved with high-intensity strength exercise programs. It should be noted however that both reviews include studies also including nutritional supplementation, and it cannot therefore be concluded that the benefit seen only comes from the prescribed exercise, which limits the conclusions drawn from them. To our knowledge, this is the first systematic review including only studies based on assessment of physical exercise.
Limitations for drawing conclusions include the difficulty to analyze and compare the results, as there is no consensus established for measurement and homogenization, particularly as regards functional tests, but also for anthropometric tests, and each study assessed different variables. Another important limitation is the great variability in the age ranges of the different studies, from 65 to over 90 years. No study assessed the potential differences in the efficacy results by age range. No sex differences in results have been evaluated either, though some studies such as the one reported Mueller et al.27 specified in the methodology that different initial weight loads were applied in strength exercises depending on sex.
These are usually short-term studies, except for the Kemmler et al. study,23 which lasted up to 72 weeks, and therefore report short-term results. When a structured, long-term training plan is made, it should be taken into account that the muscle, when subject to the same stimulus, adapts and generates a physiological plateau without achieving changes in physical qualities such as strength. Changes should be made either in strength weight, in the number of series or repetitions or in exercise duration in order to achieve better results, such as an increasing exercise load in elderly subjects with sarcopenia, something which must still be specifically analyzed with new studies.
ConclusionsExercise has significant benefits in elderly patients with sarcopenia. Aerobic (walking) exercises routinely prescribed in clinical practice do not achieve significant benefits.
Current evidence shows that training based on strength-resistance and its combination in multimodal programs with aerobic and balance exercise have significantly beneficial effects on anthropometric and muscle function parameters, and that exercises should be adapted to the characteristics of each subject.
AuthorshipD.E. Barajas Galindo, E. González Arnáiz, and P. Ferrero Vicente are responsible for the conception and design of the study. All authors participated in the writing and review of the final version of the manuscript.
Conflict of interestNone.
Please cite this article as: Barajas-Galindo DE, González Arnáiz E, Ferrero Vicente P, Ballesteros-Pomar MD. Efectos del ejercicio físico en el anciano con sarcopenia. Una revisión sistemática. Endocrinol Diabetes Nutr. 2021;68:159–169.