The SNP (rs7139228) of the DCN gene is a polymorphism that has been associated with metabolic disorder in subjects with obesity, and its effect on metabolic response after dietary intervention has not been evaluated.
ObjectiveOur objective was to analyse the effects of the polymorphism of the DCN gene rs7139228 on metabolic changes secondary to weight loss with a hypocaloric Mediterranean diet.
Design1000 obese Caucasian patients were evaluated. An anthropometric evaluation and a biochemical analysis were performed before and after 12 weeks of a hypocaloric Mediterranean diet. The statistical analysis was performed as a dominant model (GG vs GA+AA).
ResultsImprovements in anthropometric parameters, leptin levels and systolic blood pressure were similar in both genotype groups. In non- A allele carriers, levels of resistin, insulin, HOMA-IR, triglycerides and C-reactive protein decreased. The improvements were statistically significant in this group; resistin (−1.3+0.1ng/dL: p=0.02), triglycerides (−22.9+4.9mg/dl: p=0.02), CRP (−2.7+0 0.4mg/dl: p=0.02), insulin −6.5+1.8 mIU/L: p=0.02) and HOMA-IR (−2.2+0.8: p=0, 03). In addition, insulin, HOMA-IR and resistin levels were higher in A allele carriers than in non-carriers. Finally, the prevalence of metabolic syndrome and hyperglycaemia were higher in A allele carriers, and these percentages only decreased after intervention in non-A allele carriers.
ConclusionThe A rs7139228 allele is associated with a worse metabolic response (insulin, HOMA-IR, triglycerides and CRP) after weight loss with a hypocaloric Mediterranean diet. A non-significant decrease in the prevalence of metabolic syndrome and hyperglycaemia were detected in A allele carriers.
El SNP (rs7139228) del gen RETN es un polimorfismo que se ha asociado con trastorno metabólico en sujetos con obesidad y no se ha evaluado su efecto sobre la respuesta metabólica después de una intervención dietética.
ObjetivoNuestro objetivo fue analizar los efectos del polimorfismo del gen RETN rs7139228 sobre los cambios metabólicos secundarios a la pérdida de peso con una dieta hipocalórica de patrón mediterráneo.
DiseñoSe evaluó a 1000 pacientes caucásicos con obesidad. Antes y después de 12 semanas de dieta hipocalórica con patrón mediterráneo, se realizó una evaluación antropométrica y un análisis bioquímico. El análisis estadístico se realizó como un modelo dominante (GG vs GA+AA).
ResultadosLas variaciones en los parámetros antropometricos, los niveles de leptina y la presión arterial sistólica fueron similares en ambos genotipos. En los no portadores del alelo A, los niveles de resistina, insulina, HOMA-IR, triglicéridos y proteína C reactiva disminuyeron. Las modificaciones fueron estadísticamente significativas en los no portadores del alelo A; resistina (-1,3+0,1ng/dL: p=0,02), triglicéridos (-22,9±4,9mg/dl:p=0,02), PCR (-2,7±0,4mg/dl:p=0,02), insulina -6,5±1,8 mUI/L:p=0,02) y HOMA-IR (-2,2±0,8:p=0,03). Además, los niveles de insulina, HOMA-IR y resistina fueron más altos en los no portadores del alelo A. Por último, la prevalencia del síndrome metabólico e hiperglucemia fue más elevada en los portadores del alelo A y solo disminuyeron los porcentajes tras la intervención en los no portadores del alelo A.
ConclusiónExiste una asociación del alelo A rs7139228 con una peor respuesta metabólica (insulina, HOMA-IR, triglicéridos y PCR) tras pérdida de peso con dieta hipocalórica de patrón mediterráneo. Además, la disminución de la prevalencia de síndrome metabólico e hiperglucemia en los portadores del alelo A fue no significativa.
Resistin is a well-known adipocytokine initially associated with insulin resistance in in vivo models1. Resistin is secreted by adipocytes and macrophages in adipose tissue. Adipose tissue stores energy, but is also an endocrine organ that synthesises many adipocytokines. These adipocytokines play important roles in metabolism, insulin sensitivity, inflammation, satiety and appetite2 and one of the most relevant adipocytokines is the aforementioned resistin. For example, circulating levels of resistin have been associated with increased abdominal obesity, metabolic syndrome and type 2 diabetes mellitus3. However, other studies have failed to demonstrate these associations4, and therefore the literature regarding the role played by resistin in metabolism is contradictory.
The heritability of resistin levels has been described in the literature and a high percentage in the variation in circulating resistin levels can be explained by genetic factors. The gene that codes for resistin (RETN) is located on chromosome 19p13.2 and various genetic variants have been described at this locus5. For example, single-nucleotide polymorphisms (SNPs) of this gene have been reported to increase susceptibility to type 2 diabetes mellitus by increasing resistin levels6. One of these SNPs is rs7139228, which has been poorly evaluated in the literature. The intron variant SNP 5’UTR C/T (rs7139228) is a polymorphism that has been associated with elevated levels of resistin and appears in the DCN gene, which in turn encodes proteins that have been shown to be receptors for resistin7. Despite these previous data in cross-sectional studies, there are no studies in the literature evaluating the effect of the rs7139228 variant on metabolic changes after weight loss. One of the dietary regimens with the greatest beneficial effect on biochemical parameters after weight loss is currently the Mediterranean diet8. The Mediterranean diet has demonstrated cardiometabolic benefits, such as improvement in insulin resistance or lipid profile9. Some studies with other SNPs in the RETN gene have shown different metabolic responses to dietary interventions10, even after bariatric surgery11.
The objective of this study was to analyse the effects of the rs7139228 RETN gene polymorphism on metabolic changes secondary to weight loss following a hypocaloric Mediterranean diet.
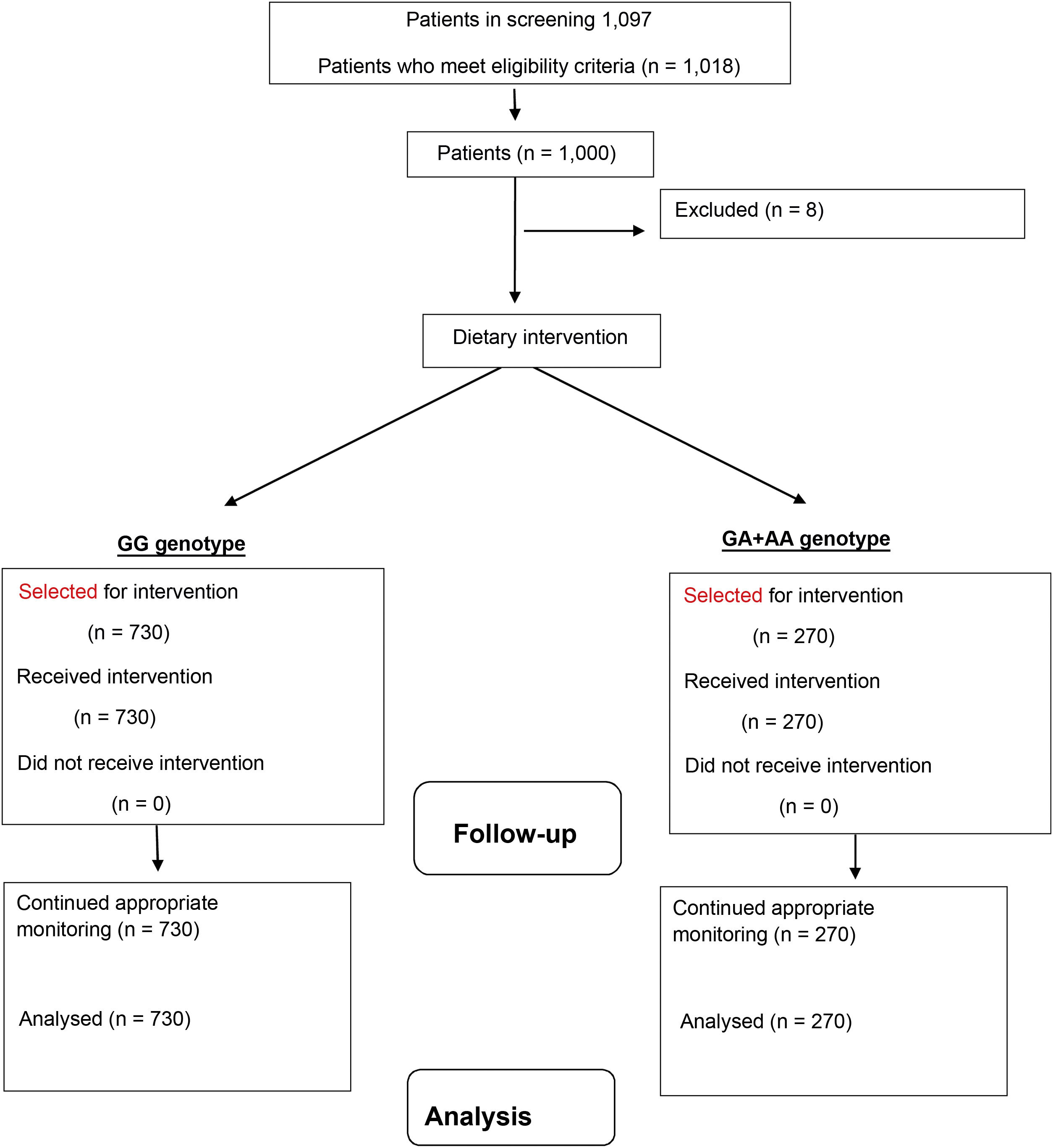
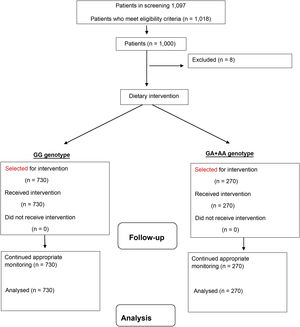
Material and methodsSubjectsWe recruited a sample of 1018 non-diabetic Caucasian adults with obesity and a body mass index (BMI) >30kg/m2) and a total of 1000 subjects were ultimately analysed (Fig. 1). Recruitment was at a single centre and took place from January 2017 to January 2022. In total, 18 patients were excluded because they had undergone dietary treatment in the six [months] prior to the start of the study. These patients were recruited prospectively with a consecutive non-probability sampling method from the obese patients of primary care physicians. The study was conducted in accordance with the Declaration of Helsinki and all procedures were approved by the HCUV Central Ethics Committee. All participants signed an informed consent form. For the inclusion of these patients, the following criteria were used: aged over 18 years, BMI>30kg/m2 and no diet for three months prior to the study. The exclusion criteria were as follows; cardiovascular events during the last 12 months, a history of diabetes mellitus, as well as the use of metformin, sulfonylureas, dipeptidyl peptidase-4 inhibitors, thiazolidinediones, insulin, GLP-1 receptor analogues, glucocorticoids, angiotensin receptor blockers, angiotensin-converting enzyme inhibitors, psychoactive agents and statins.
ProceduresFasting (12h) venous blood samples were obtained by venipuncture and collected in Vacutainer tubes. The following parameters were measured at baseline and at 12 weeks: basal fasting glucose, C-reactive protein, insulin, insulin resistance (HOMA-IR), lipid profile (total cholesterol, LDL cholesterol, HDL cholesterol, plasma triglyceride concentration) and circulating adipocytokine levels (leptin, adiponectin and resistin). In the two study times mentioned above, the following parameters were measured: fat mass by bioelectrical impedance, weight and blood pressure. The rs7139228 variant of the RETN gene was assessed at baseline.
The Adult Treatment Panel III (ATP III) criteria were used to diagnose metabolic syndrome (MetS) in subjects12. The diagnosis of MetS required at least three of the following data: elevated fasting glucose or treatment for diabetes mellitus, elevated triglycerides (>150mg/dl) or treatment for hyperlipidaemia, low HDL cholesterol <40mg/dl (men) or <50mg/dl (women), elevated systolic or diastolic blood pressure (>130/85mmHg or antihypertensive treatment) and increased waist circumference (>94cm [men] or >80cm [women]).
rs7139228 DCN gene polymorphism genotypingGenomic DNA was obtained from peripheral blood leukocytes with the Vineo Extract DNA commercial kit (Biorad CA, LA, USA), according to the manufacturer's protocol. Real-time polymerase chain reaction (PCR) was performed with 50ng of this genomic DNA, 0.5μL of 100 μM of each oligonucleotide primer (forward primer: 5′- ACGTTGGATGGCAAAGATTCTGATCTCGGG -3′ and reverse primer 5′- ACGTTGGATGCCATCATTTTCAGCATGTATG -3′). The DNA was denatured at 95°C for three minutes; 45 cycles of denaturation were performed at 95°C for 15s, and then at 59.3°C for 45s. PCR was performed in a final volume of 25μL which contained 12.5μL of IQ Supermix (Bio-Rad®, Hercules, CA) with Taq DNA polymerase. If both strands grew in a sample, this sample was classified as heterozygous. If only one strand grew in a sample, this sample was classified as homozygous. The thermocycler software classifies each patient as homozygous wild-type (GG), heterozygous (GA) and homozygous mutant (AA). In addition, a negative control and control samples representing all genotypes were included in each reaction. The Hardy-Weinberg equilibrium was determined with a statistical test (χ2). The RETN genetic variant was in Hardy-Weinberg equilibrium (p=0.49).
Laboratory testsSerum biochemical analysis of glucose, insulin, C-reactive protein, total cholesterol, HDL cholesterol and triglycerides was measured with the COBAS INTEGRA 400 analyser (Roche Diagnostic, Basel, Switzerland). LDL cholesterol was calculated using the Friedewald formula (LDL cholesterol= total cholesterol − HDL cholesterol − triglycerides/5)13. Based on glucose and insulin levels, the homeostatic model assessment of insulin resistance (HOMA-IR) was obtained using the following equation (glucose × insulin/22.5)14. Finally, all adipokine levels were determined by enzyme-linked immunosorbent assay (ELISA); resistin (Biovendor Laboratory, Inc., Brno, Czech Republic) with a sensitivity of 0.2ng/ml and a normal range of 4−12ng/ml, leptin (Diagnostic Systems Laboratories, Inc., Texas, USA) with a sensitivity of 0.05ng/ml and a normal range of 10−100ng/ml, and adiponectin (R&D Systems, Inc., Minneapolis, USA) with a sensitivity of 0.246ng/ml and a normal range of 8.65–21.43ng/ml.
Blood pressure and anthropometric parametersBlood pressure was measured three times after a 10-min rest using a mercury sphygmomanometer (Omron, LA, CA, USA) and the results were averaged.
Body weight was measured using a scale with an accuracy of 100g (Omron, LA, CA, USA) and body mass index was calculated as weight (kg)/height (m2), classifying as obese those patients with a body mass index greater than 30kg/m2. Waist circumference was also measured with a tape measure (SECA Type, SECA, Birmingham, UK) (narrowest diameter between the xiphoid process and iliac crest). The total fat mass was obtained by impedance with an accuracy of 5 g15 (EFG BIA 101 Anniversary, Akern, It). The following formula was used (0.756 height2/resistance) + (0.110 × body mass) + (0.107 × reactance) – 5.463.
Dietary interventionSubjects during this intervention study (12 weeks) received personalised advice from a single dietitian, blinded to the outcome of the evaluated polymorphism, on a hypocaloric Mediterranean diet. Caloric intake was calculated by subtracting 500 calories from the caloric intake obtained with the Harris-Benedict formula in our obese population (2,018.4±99.7kcal per day). The target percentage of energy derived from dietary carbohydrate, fat and protein was 45.7% carbohydrates, 34.4% fat and 19.9% protein. The distribution of dietary fats in the diet was: 21.8% saturated fat, 55.5% monounsaturated fat and 22.7% polyunsaturated fat (7g per day of omega 6 fatty acids, 2g per day of omega 3 fatty acids and an omega 6/omega 3 ratio of 3.5). The diet contained the following foods: extra virgin olive oil (at a rate of 30ml/day) (Oli Duero, Matarromera, Sl), three servings of fish a week, three servings of nuts a week and four to five servings a day of fresh fruit and vegetables. Follow-up for the dietary intervention was performed by phone call every 14 days by a dietitian, to increase adherence to the diet and follow-up of the protocol. All subjects were instructed to record their intakes on three different days. The records were evaluated by a dietitian using an online computer programme (https://calcdieta.ienva.org/?lang=es CIENC® diet calculator). The recommended physical exercise programme consisted of aerobic exercise at least three times a week (60min each, up to a total of 180min each week) and was recorded daily by the patient in a personalised notebook.
Statistical analysisThe sample size was calculated to detect differences greater than 1ng/ml in circulating resistin levels after following the diet with 90 % power and 5% significance (n=1000). The Kolmogorov-Smirnov test was used to determine the distribution of the variables. The data are shown as the average±standard deviation. Numerical variables with a normal distribution were analysed using a two-tailed Student's t-test. Categorical variables were evaluated with the χ2 test, with Yates's correction when necessary. Non-parametric variables were analysed using the Mann–Whitney U test. Differences in anthropometric and biochemical variables between the genotype groups were tested with analysis of covariance (ANCOVA) adjusted for age and gender, as well as baseline BMI and presence of MetS. Statistical analysis was performed with the GA and AA genotypes combined as a group (risk genotype, carriers of the A allele) and the GG genotype as a second group (wild-type genotype, non-carriers of the A allele), in a dominant model. A p value <0.05 was considered statistically significant. All analyses were performed with SPSS version 23.0. (IBM Corp., Armonk, NY, USA).
ResultsIn total, 730 (73%) were women and 270 (27%) men (n=1000). The mean age of the group was 51.2±5.2 years, with no significant age differences between men and women (51.4±5.1years vs 51.0±4.1years: ns).
After genotyping the 1000 subjects with obesity based on the rs7139228 polymorphism, the genotype distribution was as follows: 850 subjects with GG (84.8%), 146 subjects with GA (14.6%) and four subjects with AA (0.4%). The allele frequency was G (0.92) and A (0.08). By grouping the subjects to perform a dominant analysis, the following frequencies were obtained: 850 subjects with the wild-type GG genotype (84.8%), with a total of 613 women (72%) and 237 men (28%), and a total of 150 subjects (15.2%) with mutant genotype (GA+AA), 117 (78.8%) of which were women and 33 (21.2%) men.
The patients followed the dietary recommendations and in both genotypes they met the objectives regarding calorie intake and macronutrient distribution. Total caloric intake was similar in both genotypes (GG vs GA+AA) (1542.9±190.1 vs 1,495.1±119.1 calories/day; ns). The macronutrient percentage in both groups (GG vs GA+AA) was also similar: (carbohydrates: 36.0±3.1 vs 36.4±2.4%; p=0.24), (fats: 40.9+3.0 vs 41.0±2.9%; p=0.29) and (protein: 23.1±2.9 vs 22.6±1.5%; p=0.33). The distribution of dietary fats in both genotype groups (GG vs GA+AA) was similar: (monounsaturated fats; 57.9±4.1 vs 56.4±4.1%; p=0.41), (saturated fats: 21.9±3.1 vs 23.9±2.1%; p=0.39) and (polyunsaturated fats: 19.8±1.1 vs 20.1±1.9%; p=0.16). Baseline exercise was similar in both genotype groups (GG vs GA+AA) (120.9+21.4min/week vs 118.1+11.3min/week; p=0.61). No differences were detected at three months (125.1+11.3min/week vs 122.1+11.1min/week; p=0.33).
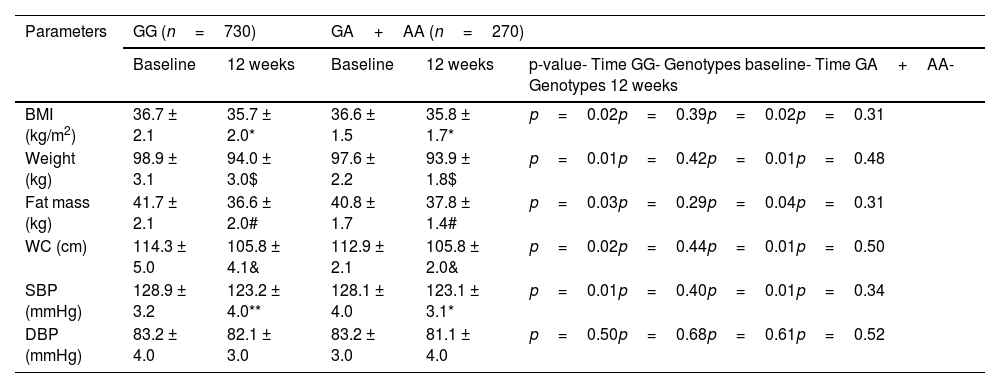
After following the hypocaloric Mediterranean diet, the following parameters decreased: weight, BMI, fat mass, systolic blood pressure and waist circumference. These significant changes were similar in both genotype groups, with no statistical differences between the two groups (Table 1). In the GG group, the weight loss was −4.9±1.2kg (decrease in carriers of the A allele −4.7±1.2kg; p=0.41), BMI −1.0±0.4kg/m2 (decrease in carriers of the A allele −0.8±0.2kg/m2; p=0.49), fat mass −3.3±1.0kg (decrease in carriers of the A allele −3.1±1.1kg; p=0.39) and for waist circumference the decrease was −9.0±2.0cm (decrease in carriers of the A allele −8.6±2.3cm; p=0.38). In non-carriers of the A allele, the decrease in systolic blood pressure was −5.7±1.4mmHg (decrease in carriers of the A allele −5.0±2.0mmHg; p=0.39), which was therefore similar in both groups. No differences in diastolic blood pressure were detected. Finally, no differences were detected between the baseline and post-treatment anthropometric parameter values between the GG vs GA/AA genotypes.
Baseline and post-intervention anthropometric parameters of obesity and blood pressure measurement (mean±SD).
| Parameters | GG (n=730) | GA+AA (n=270) | |||
|---|---|---|---|---|---|
| Baseline | 12 weeks | Baseline | 12 weeks | p-value- Time GG- Genotypes baseline- Time GA+AA- Genotypes 12 weeks | |
| BMI (kg/m2) | 36.7 ± 2.1 | 35.7 ± 2.0* | 36.6 ± 1.5 | 35.8 ± 1.7* | p=0.02p=0.39p=0.02p=0.31 |
| Weight (kg) | 98.9 ± 3.1 | 94.0 ± 3.0$ | 97.6 ± 2.2 | 93.9 ± 1.8$ | p=0.01p=0.42p=0.01p=0.48 |
| Fat mass (kg) | 41.7 ± 2.1 | 36.6 ± 2.0# | 40.8 ± 1.7 | 37.8 ± 1.4# | p=0.03p=0.29p=0.04p=0.31 |
| WC (cm) | 114.3 ± 5.0 | 105.8 ± 4.1& | 112.9 ± 2.1 | 105.8 ± 2.0& | p=0.02p=0.44p=0.01p=0.50 |
| SBP (mmHg) | 128.9 ± 3.2 | 123.2 ± 4.0** | 128.1 ± 4.0 | 123.1 ± 3.1* | p=0.01p=0.40p=0.01p=0.34 |
| DBP (mmHg) | 83.2 ± 4.0 | 82.1 ± 3.0 | 83.2 ± 3.0 | 81.1 ± 4.0 | p=0.50p=0.68p=0.61p=0.52 |
BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure; WC: waist circumference.
Statistically significant difference p<0.05, in each genotype group (* BMI, $ weight, # fat mass, & WC, ** SBP).
ANCOVA analysis adjusted for gender, age, baseline BMI and presence of MetS. First p: p value of dietary intervention after 12 weeks in the GG genotype; second p: p value between the GG versus GA+AA genotypes baseline; third p: p value of dietary intervention after 12 weeks in the GA+AA genotype; fourth p: p value between the GG versus GA+AA genotypes post-treatment.
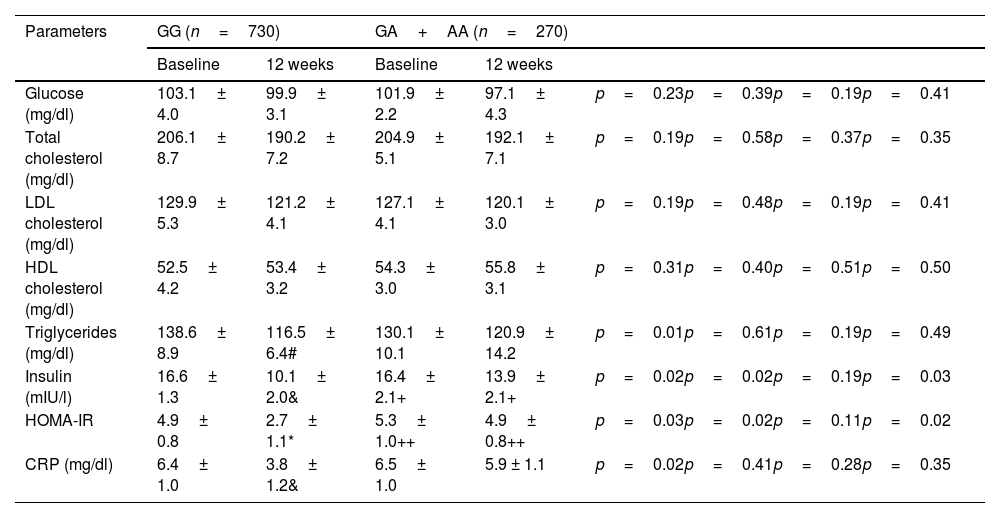
The changes in biochemical variables after the diet were not statistically significant in carriers of the A allele (Table 2). In non-carriers of the A allele, levels of insulin, HOMA-IR, triglycerides and C-reactive protein decreased. The decrease in these parameters in non-carriers of the A allele was statistically significant: triglycerides (−22.9±4.9mg/dl; p=0.02), CRP (−2.7±0.4mg/dl; p=0.02), insulin −6.5±1.8 mIU/l; p=0.02) and HOMA-IR (−2.2±0.8; p=0.03). Finally, statistical differences were detected in insulin and HOMA-IR between the baseline and post-treatment values of the variables between the genotype of the major allele (GG) and the genotype of the minor allele (GA+AA), which were higher in the latter patients.
Baseline and post-intervention biochemical parameters (mean±SD).
| Parameters | GG (n=730) | GA+AA (n=270) | |||
|---|---|---|---|---|---|
| Baseline | 12 weeks | Baseline | 12 weeks | ||
| Glucose (mg/dl) | 103.1± 4.0 | 99.9± 3.1 | 101.9± 2.2 | 97.1± 4.3 | p=0.23p=0.39p=0.19p=0.41 |
| Total cholesterol (mg/dl) | 206.1± 8.7 | 190.2± 7.2 | 204.9± 5.1 | 192.1± 7.1 | p=0.19p=0.58p=0.37p=0.35 |
| LDL cholesterol (mg/dl) | 129.9± 5.3 | 121.2± 4.1 | 127.1± 4.1 | 120.1± 3.0 | p=0.19p=0.48p=0.19p=0.41 |
| HDL cholesterol (mg/dl) | 52.5± 4.2 | 53.4± 3.2 | 54.3± 3.0 | 55.8± 3.1 | p=0.31p=0.40p=0.51p=0.50 |
| Triglycerides (mg/dl) | 138.6± 8.9 | 116.5± 6.4# | 130.1± 10.1 | 120.9± 14.2 | p=0.01p=0.61p=0.19p=0.49 |
| Insulin (mIU/l) | 16.6± 1.3 | 10.1± 2.0& | 16.4± 2.1+ | 13.9± 2.1+ | p=0.02p=0.02p=0.19p=0.03 |
| HOMA-IR | 4.9± 0.8 | 2.7± 1.1* | 5.3± 1.0++ | 4.9± 0.8++ | p=0.03p=0.02p=0.11p=0.02 |
| CRP (mg/dl) | 6.4± 1.0 | 3.8± 1.2& | 6.5± 1.0 | 5.9 ± 1.1 | p=0.02p=0.41p=0.28p=0.35 |
CRP: C-reactive protein; HOMA-IR: homeostasis model assessment-insulin resistance.
Statistical differences p<0.05, in each genotype group (triglycerides # insulin, & HOMA-IR, * CRP).
Statistical differences p<0.05, between different genotypes (+ insulin, ++ HOMA-IR).
ANCOVA analysis adjusted for gender, age, baseline BMI and presence of MetS. First p: p value of dietary intervention after 12 weeks in the GG genotype; second p: p value between the GG versus GA+AA genotypes baseline; third p: p value of dietary intervention after 12 weeks in the GA+AA genotype; fourth p: p value between the GG versus GA+AA genotypes post-treatment.
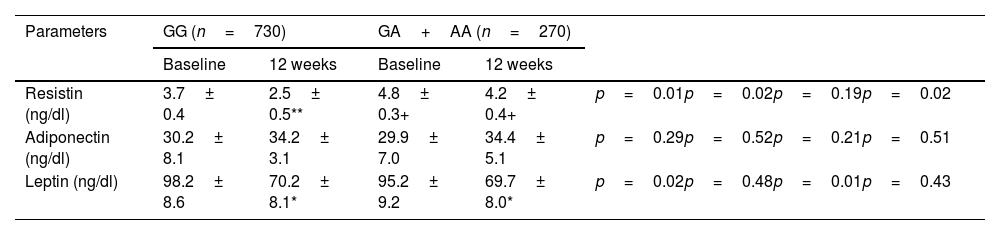
Leptin levels decreased similarly in both groups after the dietary intervention (−28.3±4.9ng/dl in non-carriers of the A allele vs −26.1±4.2ng/dl in carriers of the A allele; p=0.48) (Table 3). Resistin levels decreased in non-carriers of the A allele after the dietary intervention (−1.3±0.1ng/dl in non-carriers of the A allele vs −0.5±0.2ng/dl in carriers of the A allele; p=0.01), and did not change in carriers of the A allele. Adiponectin levels remained unchanged in both groups. Differences in resistin levels were detected between the baseline and post-treatment time between both groups of GG genotype vs GA/AA. Resistin values were higher in carriers of the A allele than in non-carriers.
Baseline and post-intervention levels of serum adipokines (mean±SD).
| Parameters | GG (n=730) | GA+AA (n=270) | |||
|---|---|---|---|---|---|
| Baseline | 12 weeks | Baseline | 12 weeks | ||
| Resistin (ng/dl) | 3.7± 0.4 | 2.5± 0.5** | 4.8± 0.3+ | 4.2± 0.4+ | p=0.01p=0.02p=0.19p=0.02 |
| Adiponectin (ng/dl) | 30.2± 8.1 | 34.2± 3.1 | 29.9± 7.0 | 34.4± 5.1 | p=0.29p=0.52p=0.21p=0.51 |
| Leptin (ng/dl) | 98.2± 8.6 | 70.2± 8.1* | 95.2± 9.2 | 69.7± 8.0* | p=0.02p=0.48p=0.01p=0.43 |
Statistical differences p<0.05, in each genotype group (* leptin, ** resistin).
Statistical differences p<0.05, between different genotypes (+ resistin).
ANCOVA analysis adjusted for gender, age, baseline BMI and presence of MetS. First p: p value of dietary intervention after 12 weeks in the GG genotype; second p: p value between the GG versus GA+AA genotypes baseline; third p: p value of dietary intervention after 12 weeks in the GA+AA genotype; fourth p: p value between the GG versus GA+AA genotypes post-treatment.
To analyse the relationship between resistin levels, rs7139228 SNP genotypes and the presence of MetS, resistin values in both genotypes were compared. Serum resistin levels were higher in carriers of the A allele with MetS (MetS 4.9±0.4ng/ml vs non-MetS 4.7±0.3ng/ml; p=0.03). However, there were no differences in resistin serum levels in patients who did not carry the A allele (MetS 3.9±0.5ng/ml vs non-MetS 3.5±0.8ng/ml; p=0.43).
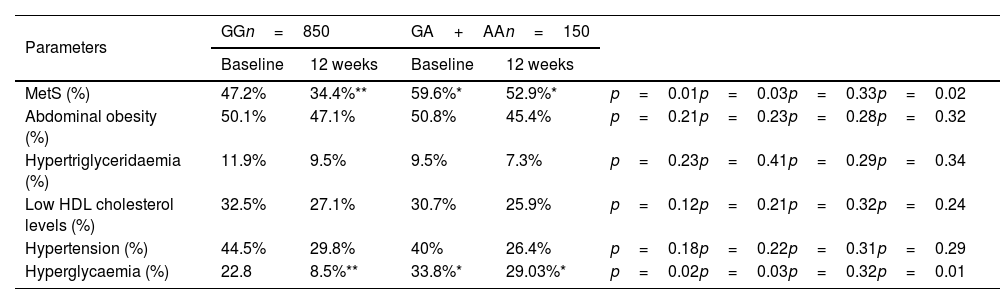
The overall prevalence of MetS in the sample was 52.1% (Table 4). The percentage of patients with metabolic syndrome and its different components (abdominal obesity, low HDL cholesterol levels, hypertriglyceridaemia, hypertension or hyperglycaemia) are shown in Table 4. The percentage of subjects with obesity who had hyperglycaemia (OR=1.65, 95% CI=1.16–2.34; p=0.03) and metabolic syndrome (OR=1.49, 95% CI=1.12–1.97; p=0.03) were higher in non-carriers of the A allele than in carriers of this risk allele. In contrast, after the dietary intervention, in non-carriers of the A allele the prevalence of metabolic syndrome (47.2 vs 34.4%; p=0.01) and the prevalence of hyperglycaemia (22.8% vs 8.5%; p=0.02) decreased, and this decrease was not significant in patients carrying the A allele (Table 4).
Metabolic syndrome and components of metabolic syndrome (MetS).
| Parameters | GGn=850 | GA+AAn=150 | |||
|---|---|---|---|---|---|
| Baseline | 12 weeks | Baseline | 12 weeks | ||
| MetS (%) | 47.2% | 34.4%** | 59.6%* | 52.9%* | p=0.01p=0.03p=0.33p=0.02 |
| Abdominal obesity (%) | 50.1% | 47.1% | 50.8% | 45.4% | p=0.21p=0.23p=0.28p=0.32 |
| Hypertriglyceridaemia (%) | 11.9% | 9.5% | 9.5% | 7.3% | p=0.23p=0.41p=0.29p=0.34 |
| Low HDL cholesterol levels (%) | 32.5% | 27.1% | 30.7% | 25.9% | p=0.12p=0.21p=0.32p=0.24 |
| Hypertension (%) | 44.5% | 29.8% | 40% | 26.4% | p=0.18p=0.22p=0.31p=0.29 |
| Hyperglycaemia (%) | 22.8 | 8.5%** | 33.8%* | 29.03%* | p=0.02p=0.03p=0.32p=0.01 |
The cut-off points for the criteria of abdominal obesity (waist circumference >80cm in women and >94cm in men), hypertension (systolic BP>130mmHg or diastolic BP>85mmHg or specific treatment), hypertriglyceridaemia (triglycerides >150mg/dl or specific treatment) or hyperglycaemia (fasting plasma glucose >110mg/dl or drug treatment for elevated blood glucose).
First p: p value of dietary intervention after 12 weeks in the GG genotype; second p: p value between the GG versus GA+AA genotypes baseline; third p: p value of dietary intervention after 12 weeks in the GA+AA genotype; fourth p: p value between the GG versus GA+AA genotypes post-treatment.
This is the first research paper in the literature that analyses the effects of a hypocaloric diet and the rs7139228 DCN genetic variant on metabolic response after weight loss. In this study analysing this genetic variant of the DCN gene, a significant association between the A allele of this SNP and a worse response of insulin resistance, basal insulin, triglycerides, C-reactive protein and circulating resistin was observed after weight loss with a hypocaloric Mediterranean diet. Furthermore, weight loss in carriers of the A allele did not lower the prevalence of MetS or hyperglycaemia. Finally, patients with obesity and who are carriers of the A allele had worse levels of insulin, HOMA-IR and resistin, as well as a higher prevalence of MetS.
As mentioned above, there is discordance over the role of resistin in metabolism and there are very few intervention studies evaluating the relationship of this molecule with some of the polymorphisms of its gene. For instance, some studies have observed that resistin levels are related to obesity and its comorbidities16, while other studies have failed to demonstrate these associations17. Furthermore, the effect of dietary or other weight loss interventions on resistin levels has not been widely studied and results are contradictory. Some studies with hypocaloric diets10 have found that resistin levels do not change following dietary intervention and secondary weight loss. However, other studies have demonstrated a decrease in resistin levels after weight loss18 or even a paradoxical increase in serum levels after weight loss19. As we have observed, the biological response of resistin is complex. For example, a group of obese patients after surgery with adjustable gastric banding demonstrated a biphasic response with an initial decrease in resistin levels and an increase after one year of follow-up20. Such disparate responses to weight loss could be explained by the nutrients found in the low-calorie diets followed, as well as genetic variants of the RETN gene that could modulate responses. For instance, Cabrera et al.21 demonstrated that the level of resistin is positively associated with the intake of saturated fats and inversely correlated with the intake of monounsaturated fats. In an intervention study22, resistin levels decreased after a dietary intervention supplemented with wakame and carob. Interestingly, based on different components of the Mediterranean diet (omega 3 fatty acids, monounsaturated fatty acids, resveratrol, quercetin, etc.), it has been suggested that the bioactive molecules of the Mediterranean diet may improve different cardiovascular risk factors through modulation of gene expression23.
The role of the genetic variants of resisitin gen has already been evaluated. For example, in a study11 with a 1500-calorie hypocaloric diet and a macronutrient distribution of 52% calories in the form of carbohydrates, 25% in the form of lipids (50% monounsaturated fats) and 23% in the form of protein, a differentiated metabolic response was demonstrated based on the rs10401670 genetic variant of the RETN gene. These results were similar with a diet that met the same caloric restriction, around 1500 calories, but with a higher fat percentage of 41% with 60% monounsaturated fats24. The composition of this latter diet is very similar to that of our current study.
A relevant result of our study is the increase in resistin levels in carriers of the A allele with worse metabolic status (insulin and HOMA-IR). It has been shown that resistin induces the synthesis of inflammatory cytokines in adipose tissue macrophages and that inflammation induces the expression of the resistin gene25, creating a vicious circle. It is well-known that the inflammatory environment is involved in the pathogenesis of insulin resistance, and circulating resistin could link inflammation and insulin resistance. For example, resistin has been shown to elevate TNF-alpha levels26 and resistin decreases the secretion of anti-inflammatory adipokines such as adiponectin27. In our intervention study, subjects with obesity and who were carriers of the A allele did not exhibit improved inflammatory parameters (CRP), insulin or HOMA-IR, with the same weight loss as non-carriers of the risk allele. The observed improvement in triglyceride levels may also be related to the improvement in the inflammatory state of patients observed after weight loss in non-carriers of the A allele. This role of resistin as an inflammatory molecule has been demonstrated in other conditions not related to obesity, such as rheumatoid arthritis and prothrombotic state28.
The increase in resistin levels found in our study in carriers of the A allele can be explained by several theories. The first is that it could be associated with the specific binding of the transcription factors Sp1 and Sp3 to a promoter element that leads to an increase in promoter activity as has been shown with other SNPs29. Second, this genetic variant may be in linkage disequilibrium with another SNP that modulates resistin expression. Third, this genetic variant could be part of a sequence of regulatory elements that mediates the binding of co-regulatory proteins involved in the regulation of RETN gene expression. Finally, this SNP could be part of a micro-RNA transcription, which regulates the transcription stability of a gene involved in the pathophysiology of metabolic syndrome.
The relationship of this SNP with MetS is interesting for detecting obese patients at high risk of developing this syndrome in clinical practice. This relationship can be explained through the elevation of resistin levels in patients carrying the A allele; resistin suppresses the differentiation of adipocytes, which leads to an overload of fatty acids and high lipotoxicity by increasing production of LDL cholesterol and degradation of LDL receptors in muscle and liver tissue, leading to increased occurrence of metabolic syndrome30. And second, circulating resistin induces insulin resistance by decreasing insulin-induced suppression of gluconeogenesis in the liver, as well as high glucose levels, by decreasing glucose transport in muscles.
There are some limitations to our work. First, only one genetic variant in the DCN gene has been assessed. Second is the lack of a control group without a dietary intervention to compare the effect of weight loss. Third, further studies are needed to validate these findings in overweight patients, as well as in diabetic patients and other high-risk populations. Finally, the short duration of the dietary intervention prevents us from observing what would happen to resistin levels and its implications over a longer period.
In summary, there is an association between the A allele with the rs7139228 variant of the decorin gene and a worse metabolic response (insulin, HOMA-IR, triglycerides and CRP) after weight loss with a hypocaloric Mediterranean diet. In addition, the decreased prevalence of metabolic syndrome and hyperglycaemia in carriers of the A allele was not significant, these being patients with a higher rate of these complications. More studies are needed to assess the importance of the presence of the A allele in obese patients, to detect patients at high metabolic risk and with a poorer response to a hypocaloric diet, and to therefore provide personalised nutrition for our patients.
Authors' contributionsDaniel Antonio de Luis and Rocío Aller designed the study and wrote the article. Olatz Izaola and Rocío Aller conducted nutritional assessments. D. Primo and D. de Luis performed biochemical evaluation.
FundingThis study did not receive any type of funding.
Conflicts of interestThe authors declare that they have no conflicts of interest.