Nonsuicidal self-injury (NSSI) and suicidal behavior (SB) have a significant prevalence in transsexual people. The published data is confusing as it does not distinguish between ideation and realization, age groups, gender, or the degree of medical intervention. Their actual prevalence in Spain is unknown.
ObjectiveOur objective was to investigate the prevalence of NSSI behavior and SB in adolescents and young transsexual adults, differentiating between ideation and consummated behavior, prior to their receiving any type of gender-affirming medical treatment.
Material and methodsWe retrospectively reviewed the medical history of a cohort of transsexual people aged between 10 and 35 years, treated at the Gender Identity Unit of the Valencian Community. We analyzed the data collected regarding the presence of four variables: NSSI ideation, NSSI behavior, ideas of suicide and suicide attempts, as well as differences according to age group and gender.
ResultsThe final sample consisted of 110 transsexual men and 90 transsexual women. Of these, 21% had made a suicide attempt, 50% had had suicidal ideas, 31% had a history of NSSI behavior and 35% had had NSSI ideas. No differences were found based on gender. Regarding age, subjects under 20 years of age presented a significantly higher prevalence regarding suicidal ideas compared to young adults (43% vs. 25%), while in the remaining variables, no statistically significant differences were found.
ConclusionsThe prevalence of a history of suicidal ideas and behavior in the Spanish adolescent and young transsexual population is significant and does not differ according to gender or age range. The prevalence of NSSI ideas and behavior differs and is more frequent in adolescent transsexuals.
Los comportamientos autolesivos (CA) y suicidas (CS) tienen una prevalencia significativa en personas transexuales. Los datos publicados son confusos al no distinguir ideación de conducta consumada, grupos de edad, género, ni grado de intervención médica. La prevalencia real en España es desconocida.
ObjetivoInvestigar la prevalencia de antecedentes de CA y CS en personas adolescentes y adultas jóvenes transexuales, diferenciando entre ideación y conducta consumada, antes de recibir tratamiento médico de afirmación de género.
Material y métodosRevisión retrospectiva de los antecedentes descritos en la historia clínica de una cohorte de personas transexuales de edad comprendida entre 10 y 35 años, atendidos en la Unidad de Identidad de Género de la Comunidad Valenciana. Hemos analizado los datos recogidos sobre la presencia de antecedentes de cuatro variables: ideas autolesivas, conductas autolesivas, ideas de suicidio e intentos de suicidio, así como diferencias por grupos de edad y género.
ResultadosLa muestra final constó de 110 hombres transexuales y 90 mujeres transexuales. A lo largo de su biografía el 21% habían realizado algún intento de suicidio, el 50% habían presentado ideación suicida, el 31% tenían antecedentes de conductas autolesivas y el 35% habían tenido ideas autolesivas. No se encontraron diferencias según género. Los sujetos menores de 20 años presentaron una mayor prevalencia, con diferencia significativa en ideación suicida con respecto a los adultos jóvenes (43% frente a 25%), en cambio, en el resto de variables, las diferencias encontradas no mostraron significación.
ConclusionesLa prevalencia de antecedentes de ideación y conducta suicida en población transexual adolescente y joven española es relevante y no difiere ni por género ni por rangos de edad. La prevalencia de antecedentes de ideas y conductas autolesivas difiere y es más frecuente en transexuales adolescentes.
The International Statistical Classification of Diseases, 10th revision (ICD-10) of the World Health Organisation (WHO) uses the term transsexualism to describe the persistent manifestation of personal conflict between gender assigned at birth and felt gender. In the latest revision of this tool, the ICD-11, transsexualism was removed from the chapter on mental disorders and added to the chapter “Conditions Related to Sexual Health”, and the use of the term “gender incongruence” was proposed. In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), however, transsexuality remains within categories of mental disorders with the term “gender dysphoria”.1 Although the WHO “depathologises” transsexuality, some transsexual people may suffer discomfort or unease (dysphoria) because of this conflict. They may also experience symptoms resulting from minority stress and, as a result, they may develop associated psychopathology or psychiatric problems.2–6
Among associated psychiatric comorbidities, those that cause the most alarm and require the most care are nonsuicidal self-injury (NSSI) and suicidal behaviour (SB). NSSI and suicide attempts are perhaps the highest expressions of dysphoria in transsexual people.
NSSI ideation and behaviour refer to when people deliberately consider inflicting or inflict injuries to their bodies without suicidal intent, such as cutting, burning and hitting themselves, as a mechanism for emotional self-control and punishment. They must be distinguished from suicidal ideation and from suicidal behaviour (SB) and suicide attempts.7–9
The lifetime prevalence of NSSI in the general American population seems to be higher among adolescents10,11 and in women.12 In the English population, a higher prevalence has been reported in the transsexual population, especially young transsexual men.13,14 In the general Spanish population, there are few data on the prevalence of NSSI, and the figures that have been published refer to special risk groups (prison inmates, adolescents with eating disorders and individuals with borderline personality disorders). To our knowledge, no previous studies have assessed the prevalence of NSSI in the Spanish adolescent and young-adult transsexual population.
With respect to SB, the prevalence is higher in the transsexual population than in the general population.15–17 In A Swedish cohort it was 2.7 per 1000 people per year for suicide deaths and 7.9 per 1000 people per year for suicide attempts.17 In the case of Spain, only one study conducted in Andalusia provides prevalence data in a sample of 197 transsexuals and its data seem to reproduce the same results, with 22.8% for suicide attempts and 52% for suicidal ideation.6
The few previous studies on NSSI and SB in transsexual people come from cohorts that were not very uniform, meaning they consisted of diverse populations, which often yields confusing results. Published series do not usually distinguish between age groups, levels of pharmacological intervention, levels of surgical intervention, degrees of satisfaction with the results or any prior clinical psychopathologies related to identity conflict and/or minority stress. The results are discordant and difficult to interpret and do not distinguish between ideation and acts.
The new care models, in which it seems that early initiation of hormonal treatments is taking precedence over holistic assessment of individuals, require endocrinologists to be fully versed in not only the clinical management of these processes, but also more psychosocial and identity-related aspects. It is increasingly common for endocrinology to be the point of entry into the healthcare circuit for transsexual people; therefore, better knowledge of these processes will enable endocrinologists to treat them more holistically, beyond mere clinical use of hormones. Medical efforts should be aimed at relieving symptoms of dysphoria and, with that, achieving better management of NSSI and SB.
The Valencian Community has had a specific healthcare protocol for transsexuality since 2008. In addition, a law for comprehensive care for transsexuality has been in place since 2017. As a result of this law, three Gender Identity Units (GIUs) were set up, one in each province. Since its creation in 2008, the leading public health GIU for the province of Valencia (Hospital Universitari Doctor Peset [Doctor Peset University Hospital]) has treated a cohort of more than 1000 cases, 36.8% of whom were under 18 years of age.
In view of the above, our objectives for this study were twofold. First, we sought to determine the ratio of transsexual males to transsexual females in a group of adolescents and young adults with gender incongruence seeking healthcare and to investigate the prevalence of NSSI and SB in this population. Second, we aimed to identify any age-based or gender-based differences between adolescents and young adults for each of the NSSI and SB variables.
Material and methodsWe conducted a cross-sectional retrospective study on data extracted from medical records in a cohort of transsexual people who sought healthcare at the Hospital Universitari Doctor Peset GIU in Valencia to change their sexual characteristics due to a persistent feeling that their gender identity was not consistent with their gender and sex assigned at birth, and who asked to initiate a process of gender-affirming hormone therapy.
SubjectsThe cases analysed represent a sample of young transsexual people without any previous interventions who were treated at the Valencia GIU under a protective, non-pathologising healthcare and legislative framework.
The population was selected by consecutive sampling of people who requested healthcare due to gender incongruence (transsexuality or gender dysphoria) from 2014 to 2017, inclusive. We used the diagnostic criteria included in the manuals used at that time, the DSM-5 and the ICD-10 (American Psychiatric Association [APA], 2014; WHO, 2000), in addition to the standards of care described by the guidelines of the World Professional Association for Transgender Health (WPATH, 2011).
The inclusion criteria were meeting the diagnostic criteria for transsexualism (ICD-10) or gender dysphoria (DSM-5). The exclusion criteria were being under 10 or over 35 years of age and not meeting persistent identity criteria. Also excluded were those who declined to take part and those with an associated mental health disorder that confounded their identity manifestation. Cases arriving with previous medical and/or surgical treatments were not also excluded in order to eliminate any type of interference.
The WHO defines adolescence as the period of human growth and development that occurs after childhood and before adulthood, between the ages of 10 and 19. The age at which a person is considered to be a young adult varies from author to author, but tends to be from 20/25 to 35/40. On that basis, we divided the sample into adolescents (10−19 years of age) and young adults (20–35 years of age). The age of 35 was therefore considered the upper limit for a young adult.
ProcedureThe GIU is structured into three levels of care: level one for psychotherapeutic care, level two for endocrine care and level three for surgical care. The initial assessment of the request starts at level one. Users follow a personalised assessment and psychological monitoring protocol before moving on to level two. In level two, they are assessed for accompanying hormone therapy according to usual clinical criteria. In level three, surgical procedures are established. The care provided in level three is accessed from levels one and two.
In initial consultations in level one of psychological care, all the subjects completed a semi-structured clinical interview to collect the data required for assessment, counselling and monitoring. This type of interview is more flexible than a structured interview, as it is based on planned questions that can be adjusted to the interviewees. The advantage is the ability to adapt to the subjects with ample opportunity to motivate them, clarify terms, identify ambiguities and reduce formalities. With very young adolescents, given their particular stage of development, the data collection model used was a semi-structured interview with the parents and not directly with the minor. As a result, some of the data collected in their medical records differed in comparison to older adolescents and young adults.
We reviewed the medical records prepared in both level one (psychotherapeutic care) and level two (endocrinology), prior to initiation of hormone therapy. Data collection distinguished between four variables: NSSI ideation, NSSI attempts, suicidal ideation and suicide attempts or suicidal behaviour (SB).
These records were searched for specific data on NSSI and SB at the first visit or any other time. NSSI and SB data were only counted if their absence or presence was reflected in the records.
Interviews were conducted either individually or with a family member, generally the mother or father (in the case of minors). All the subjects who attended the Unit granted their informed consent so that their medical records and clinical assessment data could be used for research studies. Informed consent was also obtained from parents or legal guardians of participants under 18 years of age. The study was approved by our centre’s Independent Ethics Committee, the principles of the Declaration of Helsinki were followed and the study complied with the criteria of ethics and good health practices.
Data analysisThe analysis to determine the prevalence of NSSI and SB overall and in each assessed group was performed using descriptive statistical methods. The χ2 test was used to investigate the relationship between NSSI and SB. The level of significance used was p < 0.05. Statistical analyses were performed with the SPSS 22.0® statistical program.
ResultsThe final sample was of 190 people, of whom 110 (57.9%) were transsexual males and 80 (42.1%) were transsexual females, with ages ranging from 10 to 35 (median 18.9; interquartile range [IQR] 8). The ratio of transsexual males to transsexual females was 1.4:1. The groups were divided by age, with 108 (56.8%) adolescents and 82 (43.2%) young adults. The median age in transsexual males was 18 (IQR 5; range 11–33), and the median age in transsexual females was 20 (IQR 11; range 11–34).
In the adolescent group, 87 records provided specific data on the presence or absence of NSSI and 88 records provided specific data on the presence or absence of SB, with 81% of records reviewed. In the group of young adults, 61 (74%) records provided specific data for both.
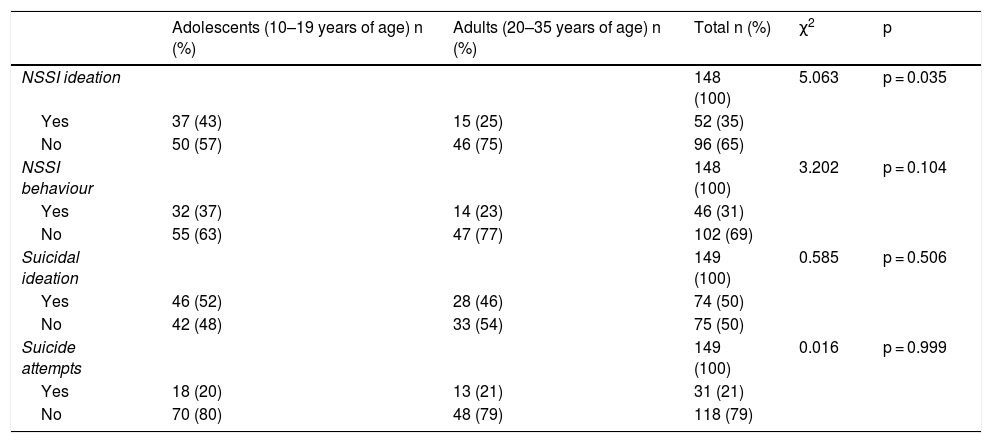
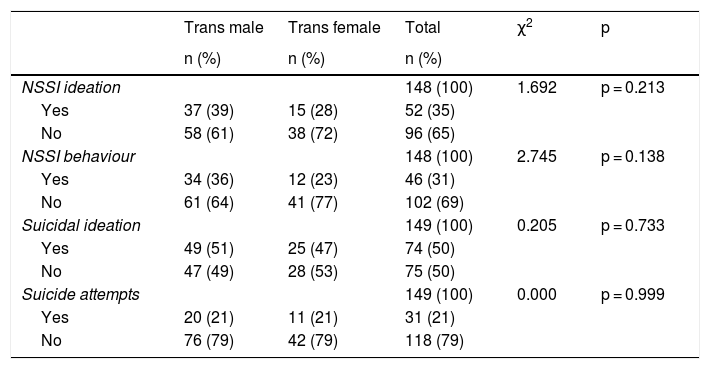
Figures for NSSI and SB prevalence by age range and gender are shown in Tables 1 and 2, respectively.
Nonsuicidal self-injury (NSSI) and suicidal behaviour (SB) according to age range.
| Adolescents (10–19 years of age) n (%) | Adults (20–35 years of age) n (%) | Total n (%) | χ2 | p | |
|---|---|---|---|---|---|
| NSSI ideation | 148 (100) | 5.063 | p = 0.035 | ||
| Yes | 37 (43) | 15 (25) | 52 (35) | ||
| No | 50 (57) | 46 (75) | 96 (65) | ||
| NSSI behaviour | 148 (100) | 3.202 | p = 0.104 | ||
| Yes | 32 (37) | 14 (23) | 46 (31) | ||
| No | 55 (63) | 47 (77) | 102 (69) | ||
| Suicidal ideation | 149 (100) | 0.585 | p = 0.506 | ||
| Yes | 46 (52) | 28 (46) | 74 (50) | ||
| No | 42 (48) | 33 (54) | 75 (50) | ||
| Suicide attempts | 149 (100) | 0.016 | p = 0.999 | ||
| Yes | 18 (20) | 13 (21) | 31 (21) | ||
| No | 70 (80) | 48 (79) | 118 (79) |
Nonsuicidal self-injury (NSSI) and suicidal behaviour (SB) according to felt gender.
| Trans male | Trans female | Total | χ2 | p | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| NSSI ideation | 148 (100) | 1.692 | p = 0.213 | ||
| Yes | 37 (39) | 15 (28) | 52 (35) | ||
| No | 58 (61) | 38 (72) | 96 (65) | ||
| NSSI behaviour | 148 (100) | 2.745 | p = 0.138 | ||
| Yes | 34 (36) | 12 (23) | 46 (31) | ||
| No | 61 (64) | 41 (77) | 102 (69) | ||
| Suicidal ideation | 149 (100) | 0.205 | p = 0.733 | ||
| Yes | 49 (51) | 25 (47) | 74 (50) | ||
| No | 47 (49) | 28 (53) | 75 (50) | ||
| Suicide attempts | 149 (100) | 0.000 | p = 0.999 | ||
| Yes | 20 (21) | 11 (21) | 31 (21) | ||
| No | 76 (79) | 42 (79) | 118 (79) |
Concerning age range, we found that NSSI ideation was more common among adolescents than adults (43% versus 25%), with these differences being statistically significant (p = 0.035). NSSI behaviour was also found to have a higher prevalence among adolescents, but this higher prevalence was not statistically significant compared to adults (37% versus 23%; p = 0.104). Regarding SB, 50% stated that they had had suicidal ideation, with no statistically significant differences between the two age groups. Suicide attempts were recorded in 21% of the records, with no differences by age group found.
From a gender perspective, of the 110 records for transsexual males reviewed, 95 contained NSSI data and 96 contained SB data, representing 87% of all trans males. The records of 53 (66%) transsexual females contained specific data.
Of the transsexual males, 39% had reported NSSI ideation and 36% had reported NSSI behaviour compared to 28% and 23%, respectively, of the transsexual females, although these differences were not statistically significant. Half of the transsexual males and females stated that they had had suicidal ideation, and 21% of both groups had made at least one suicide attempt, again with no differences between the groups assessed.
DiscussionThe results of this study provide the first data on a history of suicidal ideation and behaviour in a Spanish adolescent and young-adult transsexual population. The demand for endocrine care for transsexual people has increased in recent years, especially among young transsexual males. In Spain, the most recently published study showed that the percentage of demand from under-18s in relation to total demand from over-18s ranged from 36.8% at the Valencia Unit to 12.7% at the Madrid Unit.18 This increase can be explained by sociocultural reasons, greater visibility and medical/legal backing, increased healthcare resources, pressure from protest movements and passage of protective laws.1,18,19
There are data to suggest that when the transsexual population has access to gender-affirming social and healthcare interventions and has family and social support, their levels of psychological suffering and psychiatric comorbidity are lower.20–26
An American study from the 1990s assessed the presence of SB in 571 transgender women 10–60 years of age.15 The data showed a lifetime prevalence for suicidal ideation of 53.5%, three times higher than the estimate for the general population.16 The rate of suicide attempts was 27.9%, almost ten times higher than that corresponding to the general population.
A very high prevalence of NSSI ideation and suicidal ideation (71.8%) has been reported in the Japanese transsexual population, but without clearly distinguishing between ideation and attempts.27 The population analysed in that series was very heterogeneous, as it included data since 1997, when gender-affirming care was not so well-established and medical and surgical results were not satisfactory. Unlike our study, in which the prevalence was lower, that series included older people with less uniform levels of intervention, so its data may have been affected by the frustration generated by poor medical and surgical results and the fact of having lived in less protective and supportive environments and times.
The only study to have been conducted in Spain, in a sample of 210 transsexual people from the Malaga Unit, also reported significant rates of NSSI and SB, both of them associated with social anxiety disorder, age, depression, current cannabis use, perceived violence during childhood and adolescence, and lack of employment.3 However, this series also did not make a clear distinction between ideation and attempts, and was very heterogeneous in terms of age, year of treatment initiation and level of intervention.
One meta-analysis analysed the impact that income level, race/ethnicity and level of education might have on NSSI behaviour in the transgender population in the United States and Canada and concluded that these could significantly influence SB.28 The results of the meta-analysis showed a prevalence of suicidal ideation of 46.55% and a prevalence of suicide attempts of 27.19%. These data were consistent with those of our study, although our population was younger.
Our study only found differences between adolescents and young adults in the prevalence of NSSI ideation, and not that of NSSI behaviour, suicidal ideation or suicidal behaviour.
A study in an adolescent population in California and Georgia reviewed 1333 electronic records of transsexual people 3–17 years of age and compared them to group of non-transsexual people of the same age.29 The results showed a greater presence of suicidal ideation (5%–10%) in the former group versus the latter group.
Preliminary results from the TransYouth Project, with a sample of prepubescent transgender children (3–12 years of age) supported in their identity, compared to a group of non-transgender children of the same age, suggested that it would be possible to reduce suffering and the development of these psychological problems, with disappearance of NSSI and SB.30
Our study showed no differences in this behaviour and ideation with respect to gender.
Classically, transsexual women have been considered the most vulnerable group, and so some studies have focused only on this group; a prevalence of SB of 20.2% has been reported, although without no distinction made between ideation and attempts.31 These results were similar to of our study, in which 21% had attempted suicide and 23% had engaged in NSSI behaviour.
There are few published studies with specific data on NSSI and SB in the young population that also distinguish between ideation and attempts and differentiate by age and gender. Data from Spanish series are even more lacking.
In a study conducted on a specialised unit in the Principality of Asturias, 25% of the sample of minors were found to have a history of suicidal behaviour.19
In an American series of transsexuals under 21 years of age treated between 1998 and 2010, the rate of suicide attempts was 9.3% and the rate of NSSI was 20.6%.32 These rates were lower than ours for suicide attempts but similar for NSSI. There have also been reported prevalences of 13.1% of suicide attempts and/or NSSI in the adolescent population33 and a higher rate of NSSI in adolescent transsexual girls, but with respect to suicide attempts there are no differences between genders.34
One longitudinal study analysed predictive factors for suicide in a young population with the potential to suffer minority stress due to problems of sexual orientation (not only due to transsexuality), finding a high rate of suicide attempts (31.6%), with transsexual people being those who presented the highest such rate.35
NSSI behaviour was also very high (24%) and was associated with depression and episodes of bullying in a cohort that included data from children and adolescents in the London metropolitan area.36 In that same series, NSSI was more common in transsexual males.
A Madrid series with a sample of 56 transsexual minors yielded similar results, finding that 6% had attempted suicide.19 This prevalence was lower than that in our study in those under 20 years of age. Perhaps this difference could be attributed to the higher proportion of prepubescent children.
Our series found a higher rate of NSSI among transsexual adolescents compared to young adults, but when ideation and attempts were analysed separately, although there was more NSSI ideation than NSSI behaviour, no differences were found.
In the general non-transsexual population, rates of NSSI are as high as 14% and are clearly higher among young women.12,13 However, in the transsexual population, they seem to be higher among young men. The higher rate in young transsexual men than in transsexual women compared by age suggests that gender patterns in NSSI could be associated with the sex assigned at birth and the initial gender of upbringing of the individuals rather than with their felt gender.
The results of our study pointed in the same direction as previous studies published in English-speaking settings. One-third of the subjects in the sample had a history of NSSI (ideation or attempts), with a somewhat higher prevalence in adolescents. Our results also highlighted that, compared to transsexual females, transsexual males have had more episodes of NSSI, although the differences shown did not reach rates of statistical significance.
For SB, the results were similar according to age group and gender. Half of our population had a history of suicidal ideation, with no differences between adolescents and young adults, although ultimately the rate of people who made suicide attempts dropped to 21%, both in adolescents and in young adults. Similarly, half of the men and half of the women reported having had suicidal ideation, but in the end only 21% attempted suicide.
The main strength of our study was its clear distinction between ideation and acts or behaviour in assessing NSSI and/or SB. Other strengths included the large sample size for the population group studied, the collection of data consistent with or similar to the literature published to date and the inclusion of patients naïve to any type of previous treatment, which helped prevent bias. The series was more homogeneous and only considered adolescents and young adults prior to the start of any type of intervention. Comparison to other older age groups was definitely a distorting element as many of older people will not have benefited in their youth from quality, supportive assistance and may have experienced more situations of conflict. The resulting series had fewer elements that might influence the results and concerned a younger, more uniform population sample.
The main limitations of this study were its lack of control group for comparison, meaning that the study data had to be compared to the published data for the general population, and the fact that the population studied may have represented not the total population, but the population that sought clinical care. Another limitation was that it was a retrospective study based on a semi-structured interview, and therefore a certain percentage of the population was excluded for lack of a record of NSSI or SB. This could be explained by the fact that, for younger adolescents, information was collected through their parents. Although it was not the objective of the study, we lacked data after the start of treatment to assess changes in psychiatric comorbidity once support was being provided.
In conclusion, our results showed higher demand for care from transsexual males than from transsexual females in recent years in adolescents and young adults (1.4:1). Despite protective laws and regulated healthcare, the percentage of young transsexuals with a record of NSSI or SB remains notably high in the Valencian Community (Spain). NSSI ideation was significantly more common in adolescents than in young adults, and transsexual males had more NSSI ideation and attempts compared to transsexual females (although there was no statistically significant difference between the latter groups). Half of the sample reported having had suicidal ideation and 20% even attempted suicide, with no differences between age groups or genders. The results therefore suggested that suitable psychosocial intervention remains necessary to help prevent these serious problems affecting the particularly vulnerable young and adolescent transsexual population, and confirmed that NSSI and SB continue to be a significant public health problem in people with gender incongruence.
Suicide prevention is a global imperative in the Comprehensive Mental Health Action Plan 2013–2020 of the World Health Organization (WHO). These strategies include detection of at-risk groups. Therefore, not only mental health professionals but also endocrinologists are responsible for finding ways to resolve these matters, or at least contributing to efforts to do so.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that this article contains no patient-identifying data and that data confidentiality was maintained.
Right to privacy and informed consentThe authors declare that all participants signed an informed consent to take part in the study. Informed consent was also obtained from parents or legal guardians of participants under 18 years of age. The study was approved by our centre’s Independent Ethics Committee and the principles of the Declaration of Helsinki were followed, complying with criteria of ethics and good practices in health.
FundingNo funding was received for the research reported in this article.
Conflicts of interestThe authors received no funding to conduct this study. They also did not sign any agreement by which they would receive benefits or fees from any commercial organisation. Furthermore, no commercial organisation has made or will make payments to any foundations, educational institutions or other non-profit organisations with which the authors are affiliated.
Please cite this article as: Modrego Pardo I, Gómez Balaguer M, Hurtado Murillo F, Cuñat Navarro E, Solá Izquierdo E, Morillas Ariño C. Antecedentes de comportamientos autolesivos y autolíticos en población adolescente y adulta joven transexual, atendida en una unidad especializada en identidad de género en España. Endocrinol Diabetes Nutr. 2021;68:338–345.