Feeding behavior is integrated within a wide variety of eating behaviors, which depend on psychosocial, biological and environmental factors. These types of behavior can cause nutrition-related diseases such as obesity, which affects more than 650 million people worldwide. Ghrelin and leptin are key hormones that regulate appetite, food intake and energy metabolism. Research in genetics suggests that genetic variants of both hormones are associated with complex forms of eating behavior, such as a preference for palatable food, making individuals susceptible to the modern obesogenic environment. This review analyses the scientific evidence around polymorphisms in the ghrelin and leptin genes and their association with eating behavior. The understanding of these mechanisms is relevant since it could impact on the objectives of pharmacological or behavioral interventions for their treatment.
El comportamiento alimentario está compuesto por una amplia variedad de conductas alimentarias que dependen de factores psicosociales, biológicos y ambientales. Estas conductas pueden dar origen a enfermedades relacionadas con la nutrición como la obesidad, que afecta a más de 650 millones de personas en el mundo. La grelina y la leptina son hormonas que desempeñan un papel clave en la regulación del apetito, la ingesta de alimentos y el metabolismo energético. Las investigaciones en genética evidencian que variantes en los genes de ambas hormonas se asocian con conductas alimentarias complejas como la preferencia por alimentos palatables, lo que confiere susceptibilidad al entorno obesogénico moderno. Esta revisión analiza la evidencia científica en torno a polimorfismos en los genes de grelina y leptina y su asociación con conductas alimentarias. La comprensión de dichos mecanismos es relevante, dado que podría impactar en los objetivos de las intervenciones farmacológicas o conductuales para su tratamiento.
Ghrelin (GHRL) and leptin (LEP) play an important role in neuroendocrine control of energy homoeostasis. These hormones transmit information to the central nervous system about nutritional status.1 This information is integrated in the hypothalamus, which bears primary responsibility for homoeostatic regulation of eating.2 Both hormones act as molecular mediators that influence regulation of appetite and metabolism — GHRL by promoting food intake and LEP by inhibiting it.1 Eating behaviour encompasses a broad spectrum of behaviours that precede food intake3 and are determined by environmental, psychosocial and biological elements in constant interaction.4 Alterations in these factors may promote the onset of non-communicable nutrition-related diseases such as obesity. This disorder affects more than 650 million people around the world and is associated with more than 38 comorbidities, including type 2 diabetes mellitus, cardiovascular diseases and some types of cancer. The direct and indirect costs of obesity and added diseases vary by country; in the United States, they total an estimated 212 billion and in Brazil an estimated 10.1 billion. Hence, obesity is considered a modern global epidemic.5–8
The objective of this review is to present and analyse the scientific evidence on the association between genetic factors (single nucleotide polymorphisms [SNPs]) in GHRL and LEP genes as possible elements involved in the onset of obesity through the modulation of eating behaviours. The literature in the MEDLINE database was consulted via the PubMed interface using the following keywords and medical terms (Medical Subject Headings [MeSH]) in English to search for related articles: "single nucleotide polymorphism", "SNPs", "genotype", "genetics", "eating behavior", "feeding behavior", "ghrelin", "leptin", "food preference", "snack", "snacking", "eating in the absence of hunger" and "sweet cravings". The search was conducted in the following order: first the independent variable ("SNPs", "genotype", "ghrelin", "leptin", etc.), then the Boolean operator "AND", then the dependent variable ("eating behavior", "feeding behavior", etc.). The inclusion criteria were: analysis of at least one SNP in the GHRL and LEP genes and evaluation of at least one eating behaviour. Articles from 2007 to 2016 were included due to the limited information with the variables mentioned. Data on author, year, country, study population, study groups, gene, SNP, eating behaviour, significance level and odds ratio (OR) were taken.
Intake-regulating hormones and their role in obesityAlthough factors such as genetics, nutrition, sedentary lifestyle and food environment are involved in the development of obesity, research on evaluation of appetite and the mechanisms that regulate it highlight the importance of physiological processes, the gene expression of the hormones involved in regulation of calorie intake and expenditure, and neurotransmitter signalling in the brain.9,10
The hormones and neuropeptides involved in these processes can be classified according to their effects on food intake: on the one hand, there are appetite stimulants, including GHRL, neuropeptide Y and agouti-related protein, whose production is stimulated by feelings of hunger, resulting in promotion of food consumption; on the other hand, there are appetite suppressants, such as LEP, pro-opiomelanocortin and cocaine- and amphetamine-regulated transcript, which respond to feelings of satiety and inhibit food consumption.7 Some studies on appetite and metabolic biomarkers have included measurement of concentrations of at least one peptide (e.g. GHRL) and evaluation of at least one eating behaviour (e.g. food preference) 4, 7 and have shown that biological response can be altered in certain eating behaviours.1
Appetite is regulated through interactions between homoeostatic and hedonic mechanisms – that is, those produced in response to physiological changes in energy deposits in the three stages of eating (preprandial, prandial and postprandial); physiological mechanisms of pleasure, related to food palatability; and secretion of neurotransmitters such as dopamine and serotonin – as well as psychological factors including learning, memory and reward. The two processes, occurring in the hypothalamus, have different but not independent functions.2,4,6,11–13 As body weight is largely determined by calorie intake and expenditure, the pleasure derived from consuming certain types of foods – generally environmentally ubiquitous high-fat and high-sugar foods – can overpower homoeostatic satiety signals and promote weight gain.2,4,14
Genetic basis of eating behaviourAlthough the onset and maintenance of obesity are linked to various factors, genetic predisposition plays an important role.1,7 Research in recent decades on twin populations has found that genetics contribute to the development of obesity by 40%–70%.15 Genome-wide association studies (GWAS) have focused on identifying genetic variants involved in the onset of obesity; however, the influence that said variants in genes involved in regulation of intake and metabolism have over eating behaviours remains less explored. This mechanism could contribute indirectly to developing obesity.15
Given the diversity of biological, psychological and environmental elements involved in eating behaviour, it has been theorised that the genetic risk of developing obesity probably lies in the neurobiological regulation pathway that controls appetite. The hypothesis is that this genetic susceptibility manifests through certain eating behaviours that are stimulated by environmental signals and mediated by appetite.15,16
The following discrepancy is worthy of note: studies of point mutations in the LEP gene or its receptor (LEPR) have found that they are related to common forms of monogenic obesity, leading to severe early-onset obesity and hyperphagia and the resulting influence on appetite.17 Studies that have evaluated polymorphisms in genes for intake-regulating hormones, on the other hand, have not yielded conclusive results as to their effects on patterns of eating behaviour and polygenic obesity.18
This premise has been confirmed by GWAS conducted in different populations and by studies of associations between, on the one hand, SNPs in genes for peptides involved in appetite mechanisms, both in the hypothalamus and in the hippocampus (whose function is related to processes such as memory and learning), and, on the other hand, adiposity levels. However, only a limited number of eating behaviours have been examined. More extensive knowledge of these interactions could mean a better approach to prevention and treatment of obesity on one or more levels, since if behaviour is a mediator of the onset of the disease, including eating behaviour in gene association studies would lead to better understanding of the chain of causation.15,16,19
GWAS have identified SNPs in genes for peptides involved in regulation of food intake; however, it is not yet possible to account for variations in obesity across individuals exposed to the same food environment. Thus, predisposition to this condition lies in the sum of variants of a number of different genes, meaning that individually these SNPs correspond to a limited percentage (2%–3%) of the aetiology of obesity and are believed to jointly account for 20%–30% of cases of onset of this disease.16 Although various SNPs have been identified in genes for the main appetite-regulating hormones, few studies have examined the association between “obesity SNPs” and eating behaviours.15,16 Just as the heritability of behaviours has been proposed, it is important to note that SNPs, both in genes for appetite-regulating peptides and in their receptors, may alter physiological interactions between them and lead to the development of other metabolic disturbances, such as GHRL leptin or LEP resistance, which are also important factors linked to the development of obesity.1,20,21
Ghrelin: biology and basicsGhrelin was identified in 1999 as the ligand for the growth hormone secretagogue receptor. Its essential function is to stimulate appetite at times of acute metabolic need in the preprandial period; hence, it is inversely related to body mass index (BMI).1,22
In addition to its function in the gastrointestinal system (gastric emptying and motility), its actions include regulation of the cardiovascular system as it improves endothelial function by increasing nitric oxide bioavailability. In the immune system, it exerts anti-inflammatory effects as it inhibits type 1 T helper cells and secretion of pro-inflammatory cytokines such as interleukin 6.1,7,22–24 It also plays a role in psychological processes such as reward, memory and motivated eating behaviour, through the action of the hormone on the dopaminergic system in the ventral tegmental area, where the growth hormone secretagogue receptor is found to be widely distributed, thus increasing the frequency and likelihood of dopamine release.2,7
GHRL is a hormone consisting of 28 amino acids that is secreted primarily by the endocrine cells of the oxyntic glands in the gastric fundus and, to a lesser extent, in tissues of other organs in the body such as the heart, lungs, pancreas, immune system, ovaries and thyroid gland.2,7,13,22,23
The GHRL gene is composed of 4 exons and codes for a precursor peptide consisting of 117 amino acids: preproghrelin. This is processed after translation into at least five products, the most important of which are obestatin and desacyl ghrelin.1 For GHRL to perform its appetite-suppressant activities, prior to its secretion, desacyl ghrelin needs to be acylated by the enzyme GHRL O-acyltransferase, at the serine at position 3 of the peptide; this enables it to then access the active binding site of the growth hormone secretagogue receptor.1,2,7,13 It has been postulated that the GHRL O-acyltransferase-GHRL system may act as a sensor of nutrient availability, in particular medium-chain fatty acids, as a signal of availability of high-calorie foods, which are used as substrates for acylation and promote the production and secretion of acyl-ghrelin.1,22
Circulating levels of GHRL vary by energy status; they increase under fasting conditions, decrease in the postprandial period and go up and down in accordance with an individual's eating patterns.1,2,22 Total plasma GHRL levels range from 300 to 800 pg/mL, and low levels have been linked to insulin resistance and type 2 diabetes mellitus. In addition, differences have been reported between people with type 2 diabetes mellitus and different body compositions. Under fasting conditions, people with obesity have lower plasma GHRL levels, while individuals with higher muscle mass have higher plasma GHRL levels. For this reason, an inverse relationship between plasma GHRL and BMI in healthy subjects and subjects with obesity has been postulated. It has also been reported that the postprandial decrease in serum GHRL is lower in groups with obesity versus controls with a normal BMI, since GHRL levels increase during dieting-induced weight loss.7,25
Ghrelin and eating behaviourAs mentioned above, eating behaviours depend on a wide variety of factors, and some studies in murine models have found that neurobiological processes of hormones such as GHRL (which is involved in homoeostatic and hedonic systems) may direct other behavioural responses beyond food intake.26
A study by Schéle et al., conducted in 201626 in male Sprague Dawley rats, consisted of intracerebroventricular injections of GHRL with the objective of determining whether the hormone is capable of directing food choices between standard chow and chow with a different distribution of nutrients (fat and sucrose) after night-time fasting. The researchers reported that GHRL may alter food choices in the acute food restriction period, with notable effects for promoting intake of low-fat and low-sucrose chow. These results were replicated in a 2017 study by Bake et al.;27 based on the same procedure, the effects of GHRL on food choices during binge-eating behaviours were evaluated. The findings supported the notion that GHRL acts as a modulator of food choices under experimental conditions, encouraging selection of more nutritious options.26,27
Eating behaviours are also regulated by social learning signals; however, the neurobiological mechanisms through which they are carried out have not been described in full. One hypothesis proposed is that GHRL signalling in the hippocampus promotes social learning of eating behaviours. A 2018 study by Hsu et al.28 used a procedure called “social transmission of food preference” with male Sprague Dawley rats divided into 2 groups: O (observers) and D (demonstrators). In the study, the O rats (who were administered GHRL) experienced social interaction with the D rats, who consumed chow with a specific flavour or odour. The results showed that pharmacological activation of the GHRL signalling pathway increased the rats' preferences for foods associated with social interaction with other rats.28 This evidence opens up new research prospects for studies in humans and contributes to existing knowledge of the molecular basis of eating behaviour and obesity.
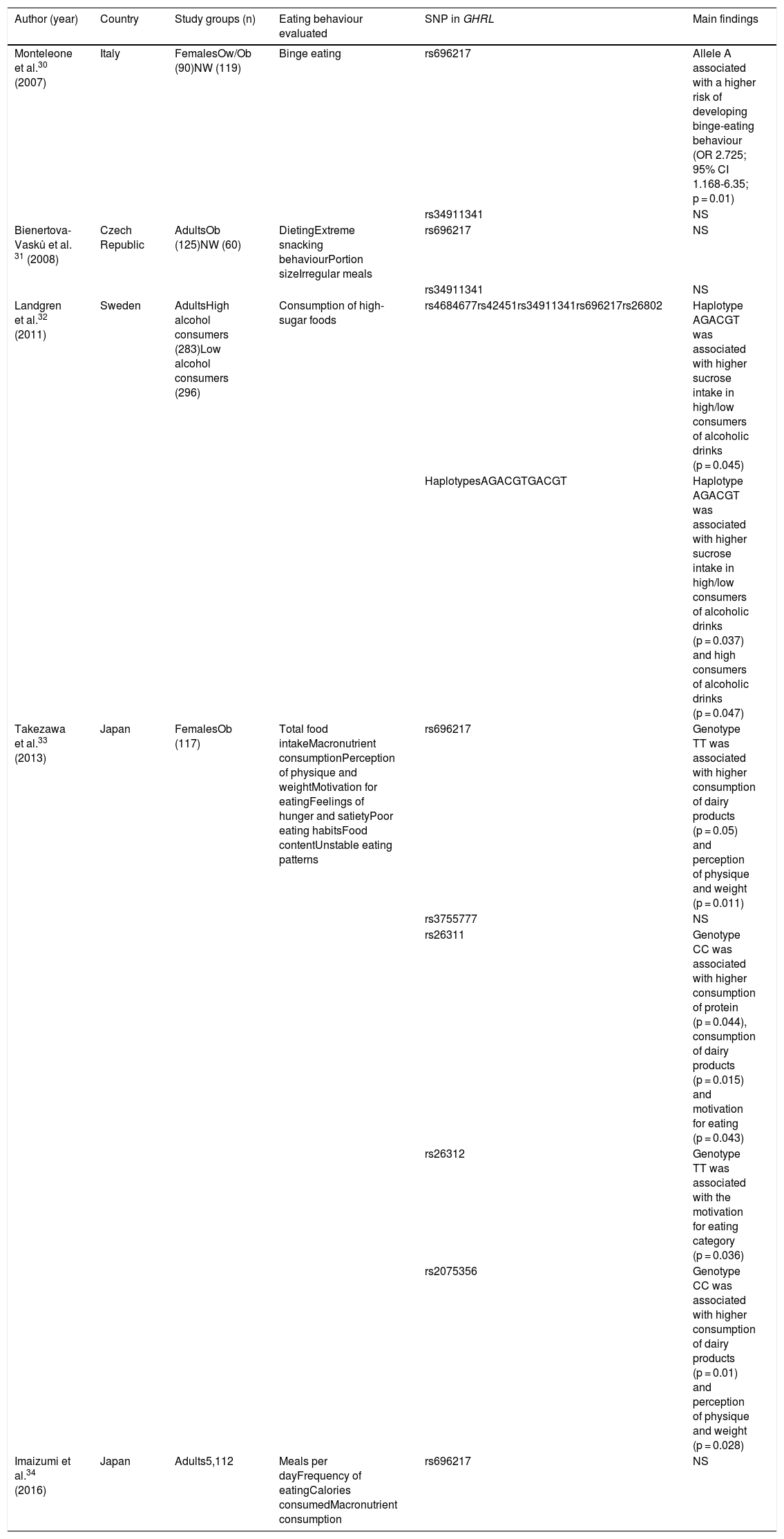
Association between SNPs in ghrelin and eating behavioursFive articles on the association between SNPs in the GHRL gene and eating behaviours were found; these five articles were conducted in adults of both sexes in European and Asian countries.29–33Table 1 features a summary of these studies.
Association between GHRL gene SNPs and eating behaviours.
| Author (year) | Country | Study groups (n) | Eating behaviour evaluated | SNP in GHRL | Main findings |
|---|---|---|---|---|---|
| Monteleone et al.30 (2007) | Italy | FemalesOw/Ob (90)NW (119) | Binge eating | rs696217 | Allele A associated with a higher risk of developing binge-eating behaviour (OR 2.725; 95% CI 1.168-6.35; p = 0.01) |
| rs34911341 | NS | ||||
| Bienertova-Vasků et al. 31 (2008) | Czech Republic | AdultsOb (125)NW (60) | DietingExtreme snacking behaviourPortion sizeIrregular meals | rs696217 | NS |
| rs34911341 | NS | ||||
| Landgren et al.32 (2011) | Sweden | AdultsHigh alcohol consumers (283)Low alcohol consumers (296) | Consumption of high-sugar foods | rs4684677rs42451rs34911341rs696217rs26802 | Haplotype AGACGT was associated with higher sucrose intake in high/low consumers of alcoholic drinks (p = 0.045) |
| HaplotypesAGACGTGACGT | Haplotype AGACGT was associated with higher sucrose intake in high/low consumers of alcoholic drinks (p = 0.037) and high consumers of alcoholic drinks (p = 0.047) | ||||
| Takezawa et al.33 (2013) | Japan | FemalesOb (117) | Total food intakeMacronutrient consumptionPerception of physique and weightMotivation for eatingFeelings of hunger and satietyPoor eating habitsFood contentUnstable eating patterns | rs696217 | Genotype TT was associated with higher consumption of dairy products (p = 0.05) and perception of physique and weight (p = 0.011) |
| rs3755777 | NS | ||||
| rs26311 | Genotype CC was associated with higher consumption of protein (p = 0.044), consumption of dairy products (p = 0.015) and motivation for eating (p = 0.043) | ||||
| rs26312 | Genotype TT was associated with the motivation for eating category (p = 0.036) | ||||
| rs2075356 | Genotype CC was associated with higher consumption of dairy products (p = 0.01) and perception of physique and weight (p = 0.028) | ||||
| Imaizumi et al.34 (2016) | Japan | Adults5,112 | Meals per dayFrequency of eatingCalories consumedMacronutrient consumption | rs696217 | NS |
NS: not significant; NW: normal weight; Ob: obesity; Ow: overweight.
The most commonly analysed SNP was rs696217 (Leu72Met), located on exon number 2; it has been postulated that it may cause modifications in GHRL secretion.25,34 Among the eating behaviours evaluated, the most common was related to food/high-calorie food intake and food preferences, followed by snacking behaviours, binge eating, motivation for eating and portion size.
A study conducted in 2007 by Monteleone et al. in an Italian population had study groups consisting of 90 women with overweight or obesity and 119 women with normal weight. They were genotyped for two SNPs in the GRHL gene (rs696217 and rs34911341), and the association between those SNPs and binge-eating behaviour was evaluated through psychometric tests for assessment of eating-related psychiatric diseases. The statistical analysis indicated that allele A of the rs696217 variant was significantly more common in patients who presented binge-eating behaviour, and therefore was associated with a moderate risk of developing this behaviour (OR 2.725; 95% CI 1.168-6.35; p = 0.01).29
In 2008, Bienertova-Vasků et al. conducted a study in the Czech Republic in subjects of both sexes: 125 with obesity and 60 with normal weight. Two genetic variants in the GHRL gene were analysed (rs696217 and rs34911341) and food intake was evaluated using seven-day dietary recall, through which extreme snacking behaviours, dieting, extreme portion sizes and irregular meals were also analysed. According to the statistical analysis, none of the SNPs studied was a predictor of the eating patterns reflected in this population's dietary recall.30
A common reward mechanism for consumption of alcohol and sweets in both animals and humans has been hypothesised.35 Based on the known roles of GHRL in energy balance and in the reward system, in 2011, Landgren et al. performed a meta-analysis of haplotypes including six genetic variants in the GHRL gene (rs4684677, rs42451, rs35680, rs34911341, rs696217 and rs26802). The haplotypes analysed were AGACGT and GACGT in two study groups: high alcohol consumers (n = 283) and low alcohol consumers (n = 296), classified according to their alcohol and sucrose consumption, in an American population. Consumption of both was evaluated using a questionnaire on frequency of consumption of different alcoholic drinks and high-sugar foods. Haplotype AGACGT was associated with higher sucrose intake in subjects with high and low alcohol consumption (p = 0.045), and haplotype GACGT was associated with higher sucrose intake among individuals in both groups (p = 0.037) and with subjects with high alcohol consumption(p = 0.047); however, the association was not maintained after methodological adjustments were made for haplotype GACGT.31
In 2013, Takezawa et al.32 analysed five SNPs in GHRL (rs3755777, rs26311, rs26312, rs696217 and rs2075356) in 117 Japanese women with obesity to study the relationship between genotypes and eating trends by food group. They were evaluated using a self-administered dietary history questionnaire in which their food habits and macronutrient consumption were estimated through statements classified in categories according to food group using a frequency of consumption. Genotype CC of the rs26311 SNP was significantly associated with consumption of protein (g/day) (p = 0.044), consumption of dairy products (g/day) (p = 0.015) and with the motivation for eating category from the self-administered dietary history questionnaire (p = 0.043). Genotype TT of the rs26312 was associated with the motivation for eating category (p = 0.036). Genotype TT of the rs696217 SNP was associated with consumption of dairy products (g/days) (p = 0.050) and with the perception of physique and weight category (p = 0.011); genotype CC of the rs2075356 SNP was significantly associated with the same parameters (p = 0.014 and 0.028, respectively).32
A retrospective study conducted by Imaizumi et al. in 201633 analysed the rs696217 variant of the GHRL gene in a Japanese population and evaluated lifestyle (quantity of macronutrients and eating patterns in the past six months) through dietary recall, as well as anthropometric parameters, in 5,112 adults, with no specific exclusion criteria in relation to body composition. The eating data analysed were number of meals per day, frequency of foods per month and number of calories per meal (kcal/meal), as well as quantity of salt, fat, carbohydrates and protein (g/meal). The statistical analyses did not show an association between the SNP in the GHRL gene and any eating variable, but they did point to an association between obesity and allele G (OR 1.40; 95% CI 1.13–1.74; p = 0.002).33
The studies presented offer new evidence on the genetic basis of eating behaviours; however, it is important to note that few have been conducted to date in different populations around the world, which makes it difficult to generalise their results in view of racial differences. GWAS represent an important opportunity to identify genetic variants of other peptides involved in appetite regulation, which would expand research on other eating behaviours.
Leptin: biology and basicsLeptin was discovered in 1994 and identified as a lipostat —i.e. a substance that promotes a response in the presence of lipids stored in adipocytes. Its main functions were subsequently found to include appetite suppression and regulation of energy expenditure through transmission of information to the brain about energy deposits in the body and their availability by suppressing the activity of neurons and neuropeptide Y and stimulating pro-opiomelanocortin neurons and cocaine- and amphetamine-regulated transcript in the arcuate nucleus of the hypothalamus.1,14,22
LEP is a protein consisting of 167 amino acids encoded by the LEP gene. It is primarily secreted by adipocytes, and although it is expressed in other tissues such as the bone marrow, ovaries, placenta, stomach and lymphoid tissue, adipose tissue is responsible for an estimated 95% of LEP production.1,14,22 LEP exerts its action through its receptor (LEPR), which is mostly expressed in the hypothalamus and brain tissues such as the cerebellum.1,22 LEP levels transmit information on energy reserves in the body to the nuclei in the hypothalamus that regulate homoeostasis. An increase in energy deposits increases its production, which triggers a physiological response to reduce food intake and promote energy expenditure.1
Due to the relationship between the amount of adipose tissue in an individual and LEP production, total plasma LEP levels in people with normal weight range from 3 to 18 ng/mL, and they are higher in women than in men; in individuals with a BMI exceeding 30, values of 30 ng/mL or even higher can be found. The phenomenon of LEP resistance has been reported; it is linked to alterations in plasma LEP levels commonly found in subjects with obesity and contributes to maintaining this disease.1 It has been hypothesised that said resistance results from abnormalities in LEP signalling. This is dependent on molecular mechanisms such as deficiencies in the passage of the hormone through the blood–brain barrier, leading to high circulating LEP levels, suppression of LEPR signalling and cellular inflammation, which are linked to intake of high-fat foods.1,36
Leptin and eating behaviourHedonic regulation of food intake has gained attention in the field of obesity research; studies have found that LEP behaves similarly to GHRL by not only acting on regulation of energy expenditure and food intake but also regulating the reward system in the brain by suppressing postprandial neural activity.10,37
Studies in murine models and the use of paradigms such as conditioned place preference, employed by Shimizu et al. in a 2017 study10 in male C57BL/6 mice to elucidate the effects of LEP on preferences for high-fat diets in thin mice and LEP-deficient obese mice, have shown that, under non-experimental conditions, LEP-deficient mice have a stronger preference for fatty diets, but that this preference changes when LEP is administered, with food intake dropping to levels comparable to those in thin rats.10
Another study related to food preference and flavour perception was conducted by Kawai et al. in 2000 in BALB and C57BL mice divided into groups: obese diabetic mice with LEPR deficiencies, normal-weight non-diabetic mice and normal-weight mice. Surgery was performed in which the nerves responsible for the peripheral response to sweet substances (the glossopharyngeal [ninth cranial] and chorda tympani nerves) were removed, LEP was administered to the normal-weight subjects and the response to sweet stimuli was shown to be suppressed; however, the same was not found in the mice with LEPR deficiencies. The results showed that LEP may suppress detection of sweet stimuli and in turn play a role in regulation of food intake.37 However, they were not conclusive; other molecular pathways, such as polymorphisms in sweet-sensing taste receptors, have been proposed to account for this phenomenon.
Studies in murine models provide new ideas for studies in humans based on molecular and mechanistic explanations in animals, in which physiological and behavioural variables can be isolated to yield better understanding.
Association between SNPs in leptin and eating behavioursFive studies were found on associations between SNPs and the LEP gene and eating-related behaviours, They were conducted in adults of both sexes in countries in Europe and Asia.30,38–41 The studies are summarised in Table 2.
Association between LEP gene SNPs and eating behaviours.
| Author (year) | Country | Study groups (n) | Eating behaviour evaluated | SNP in GHRL | Main findings |
|---|---|---|---|---|---|
| De Krom et al.38 (2007) | The Netherlands | FemalesOb (72) | Portion sizeSnacking behaviour | rs791607 | Genotype CT was associated with more snacking (p = 0.01) |
| rs4577902 | Genotype CT was associated with more snacking (p = 0.006) | ||||
| rs2060736 | NS | ||||
| rs4731413 | NS | ||||
| Mizuta et al.39 (2008) | Japan | Adults3,653 | Preference for sweet foods | rs7799039 | NSGenotype AA: protective factor (OR 0.91; 95% CI 0.77-1.09) for preference for sweet foods |
| rs2167270 | NSGenotype GG: protective factor (OR 0.82; 95% CI 0.69-0.98) against preference for sweet foods | ||||
| Bienertova-Vasků et al.31 (2008) | Czech Republic | AdultsOb (125)NW (60) | DietingExtreme snacking behaviourPortion sizeIrregular meals | rs7799039 | NS |
| Bienertová-Vasků et al.40 (2010) | Czech Republic | AdultsOb (252)NW (157) | Macronutrient consumptionExtreme snacking behaviourPortion sizesIrregular meals | rs2167270 | Association of genotype AG with higher calorie intake at dinner (p = 0.05) |
| Dougkas et al.41 (2013) | United Kingdom | MalesOw (40) | HungerDesire to eatFullnessProspective consumptionFood intake | rs7799039 | Association of genotype GA with fullness (p = 0.02) and prospective consumption (p = 0.28) |
NS: not significant; NW: normal weight; Ob: obesity; Ow: overweight.
The most commonly analysed SNP was rs7799039 (G-2548A), located in the gene promoter; it has been found to influence plasma LEP levels. The most commonly evaluated eating behaviours were food preferences, followed by food intake, including determinant psychometric parameters, snacking behaviour and portion sizes.
A 2007 study by De Krom et al. included 72 women with obesity from the European Prospective Study into Cancer and Nutrition cohort in the Netherlands, selected with the following criteria: BMI ≥ 33 kg/m2; score in the top fifth percentile for snacking behaviour, based on 11 questions on snacking frequency; and a score in the top fifth percentile for food intake, based on 28 questions using photographs to estimate portion sizes. Four genetic variants in the LEP gene were analysed (rs791607, rs4577902, rs2060736 and rs4731413). Genotype CT of the rs791607 SNP and genotype CT of the rs4577902 SNP were found to be significantly associated with higher snack consumption (p = 0.01 and 0.006, respectively), but not portion sizes.38
In Japan, Mizuta et al. conducted a 2008 study with 3,653 adults of both sexes in which preferences for sweet foods were evaluated using a Likert questionnaire to form two study groups: case (those with higher scores for preferences for sweet foods) and control (those with lower scores). Two SNPs for the LEP gene were genotyped (rs7799039 and rs2167270). The statistical analysis showed an OR of 0.82 (95% CI 0.69-0.98) and a significant association for the dominant model (GG) of the rs2167270 variant in preferences for sweet foods; hence, this genotype can be considered protective against exhibiting this food preference. For the dominant model (AA) of the rs7799039 SNP, an OR of 0.91 (95% CI 0.77-1.09) was established.39 However, the results for this SNP should be interpreted with caution given the range of confidence intervals of the association test.
Bienertova-Vasků et al. conducted a study in the Czech Republic in 2008 in subjects of both sexes: 125 with obesity and 60 with normal weight. One SNP in the LEP gene (rs7799039) was analysed and food intake was evaluated using a seven-day dietary recall, through which extreme snacking behaviours, dieting, extreme portion sizes and irregular meals were also analysed. The results showed no significant association between this SNP and the eating patterns reported by the participants in this population.30
Although the above study did not reveal any significant association, due to the trends towards specific nutritional behaviours observed, in 2010, Bienertová-Vasků et al. conducted another study in 409 individuals divided into two groups: 252 with obesity and 157 with normal weight. They analysed the rs2167270 SNP and evaluated seven-day dietary recall to determine the distribution of dietary macronutrients and dietary patterns such as extreme snacking behaviours (with calorie intake exceeding 25% of the daily total), portion sizes and irregular meals. Genotype AG of the SNP was significantly associated (p = 0.05) with higher calorie intake, as well as a trend towards higher intake at dinner.40
Dougkas et al., for their part, conducted a 2013 study in 40 men with overweight in the United Kingdom in which they analysed the rs7799039 variant of the LEP gene and evaluated, using a Likert visual analogue scale, appetite profile (hunger, desire to eat, fullness and prospective consumption), as well as grams of food and calories consumed (kJ) during an experimental session. Genotype GA was significantly associated with fullness (p = 0.02) and prospective consumption (p = 0.028).41
SNPs in the LEP gene broaden knowledge of genetic influences on eating behaviours as possible causative agents in obesity. As indicated, special attention must be paid to the limited nature of study populations, not only for genetic reasons but also for behavioural ones, since eating behaviours are exhibited depending on the different food environments to which individuals are exposed. One consideration in studies of polymorphisms of the hormones presented relates to the number of subjects and the study groups in each study. On the one hand, numbers of individuals were low, and although those who met the criterion of a certain anthropometric indicator (overweight or obesity) were included, the majority of the studies lacked a comparator group (e.g. normal-weight individuals) to compare and contrast the association between them.
ConclusionsMany factors contribute to the complexities of eating behaviour in general and to exhibition of specific eating behaviours.4 The hormones GHRL and LEP are two key mediators in regulating metabolism and energy balance that act on the hypothalamic nuclei in the central nervous system by integrating environmental signals that indicate the availability of food and the start and end of the eating episode. Interaction between the above elements determines food intake, composition of meals and portion sizes, among other things, and is reflected in variations in body weight across individuals.1,4,13
Studies that have examined the role of these hormones and eating behaviours and their consequences (e.g. obesity) have made it possible to propose that a possible cause of alterations in the molecular mechanisms of peptides might be SNPs in the genes that code for them, which could lead to changes in the production and/or actions of the hormones.7
This article examined studies of association of GHRL and LEP gene SNPs with eating behaviours. It is important to point out that there is evidence of significant associations between certain SNPs and some eating behaviours. While the association of variables such as sedentary lifestyle, high intake of calorie-dense foods and hormonal factors with the prevalence of obesity has been demonstrated, it is imperative to identify and characterise the genetic mechanisms involved, as this could change the objectives for pharmacological, behavioural or psychological interventions.15
AuthorshipASEG and ZRC participated in conceiving of the idea for the manuscript. ASEG drafted the manuscript. ZRC and AGMM critically reviewed the article and contributed to improving it. All authors have read and expressed their approval of the final manuscript.
FundingThis study was conducted thanks to funding from the Consejo Estatal de Ciencia y Tecnología de Jalisco [Jalisco State Science and Technology Council] (COECYTJAL), call for bids FODECIJAL-2019, to address state problems (project No. 7942), granted to ZRC. ASEG received a grant from the Consejo Nacional de Ciencia y Tecnología [Mexican National Science and Technology Council] (CONACYT) for postgraduate studies (grant No. 779720).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Espinoza García AS, Martínez Moreno AG, Reyes Castillo Z. Papel de la grelina y la leptina en el comportamiento alimentario: evidencias genéticas y moleculares. Endocrinol Diabetes Nutr. 2021;68:654–663.